Literature in this issue

01
Background of the study
The average operative mortality rate for type A or non-A non-B acute aortic coarctation involving the aortic arch is 20% to 25% [1]. If combined with distal malperfusion syndrome, patient mortality increases significantly. Emergency repair of the proximal aorta prevents acute rupture of the aorta and relieves dynamic types of organ malperfusion, but is less effective in static or mixed types of malperfusion [4]. In addition, prolonged extracorporeal circulation and deep hypothermia arrest can lead to secondary ischemia and increased ischemia-reperfusion injury in distal organs, resulting in poor postoperative outcomes.
Professor Hu Jia's team was the first to propose the concept of reverse staged hybridization [6-7], which prioritizes the use of interventional techniques to improve the perfusion of distal poorly perfused organs, and then performs a two-stage hybridization surgery to repair the proximal aorta after the function of the organs is improved. In this paper, five patients with acute aortic coarctation syndrome who underwent reverse staged hybridization at West China Hospital were included, which initially demonstrated the safety and efficacy of this technique, and helped to increase the perioperative survival rate of the patients and improve the near- and long-term clinical outcomes.
02
Clinical information
Patients with acute aortic coarctation combined with distal malperfusion syndrome involving the aortic arch at the Department of Cardiac Major Vascular Surgery, West China Hospital, Sichuan University, from May 2019 to December 2022 were included, all of whom had preoperative CTA showing aortic coarctation involving the involvement of the aortic arch and the presence of malperfusion of at least one distal organ vessel, such as the celiac trunk arteries, superior mesenteric arteries, renal arteries, or arteries of the lower limbs (Figure 1) Significant laboratory abnormalities and signs and symptoms of organ insufficiency were present.
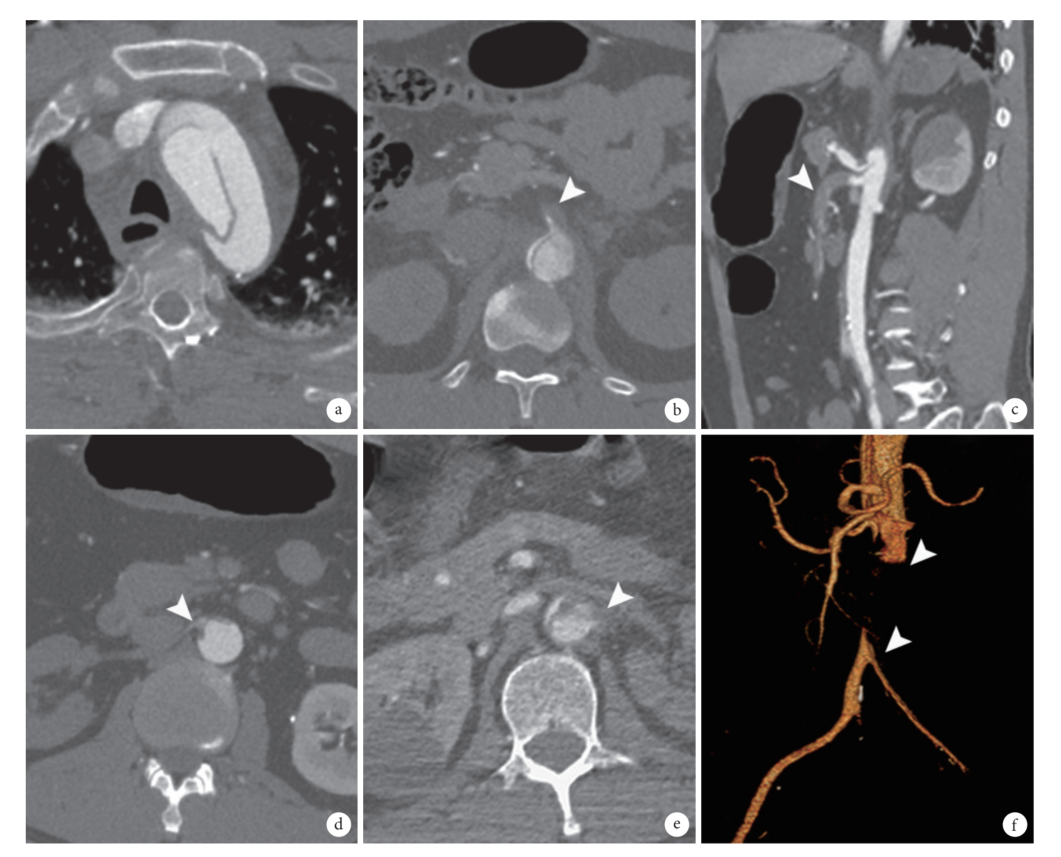
Figure 1 : Involving the aortic arch
Characterization of the impact of acute aortic coarctation combined with malperfusion syndrome
a: rupture of entrapment in the aortic arch
b: Poor perfusion of the celiac trunk artery
c: poor perfusion of the superior mesenteric artery
d: poor perfusion of the right renal artery
e: Poor perfusion of the left renal artery
f: Poor perfusion of lower extremity arteries
03
Surgical method
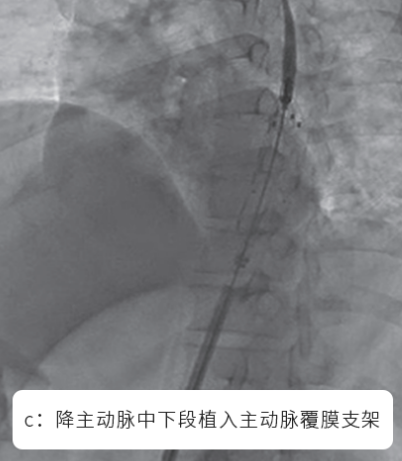
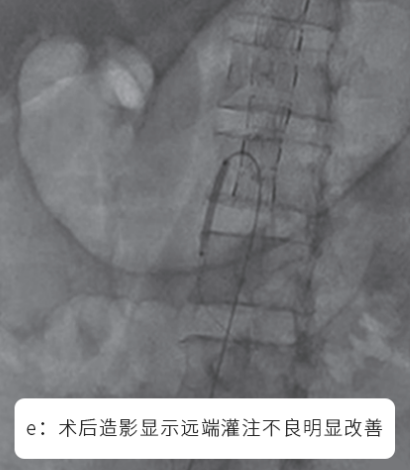
Depending on the recovery of distal perfusion, a bare stent is articulated distally using the PETTICOAT technique to better facilitate distal true lumen expansion (Figure d). Based on the improvement of distal perfusion, balloon dilatation, stenting, or aortic endarterectomy of the branch arteries of the target organ is performed if necessary (Figure e). After the final imaging confirms that the perfusion of the poorly perfused organ has significantly improved, the interventional device is withdrawn (Figure f), the access vessel is sutured and pressure bandaged, and the patient returns to the monitoring room to continue supportive treatment.



The recovery of poorly perfused organs was assessed according to the laboratory tests and CTA after the first stage of intervention, and the proximal aorta was repaired by a second-stage hybridization procedure after the recovery of the organs.
04
Results
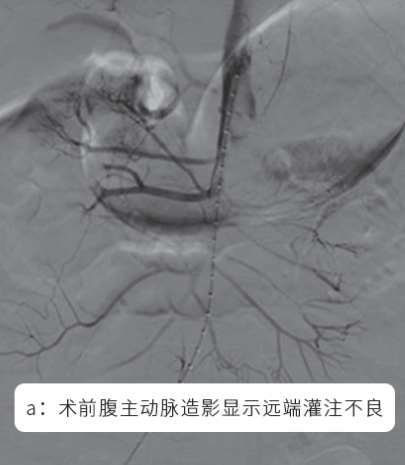
The preoperative data are shown in Table 1. 4 cases of type A aortic coarctation, 1 case of non-type A and non-type B aortic coarctation, 3 cases of lower limb ischemia and renal insufficiency as the main manifestations, and 2 cases of intestinal malperfusion as the main manifestations. In the first stage of surgery, 4 cases were dynamic type of malperfusion, only the descending aorta was implanted with overlay stent, and 1 case was mixed type of malperfusion, which was articulated distally with a bare stent using PETTICOAT technique, and at the same time, localized balloon dilatation of the superior mesenteric artery was carried out. The average waiting time for the second-stage surgery was 3.2 d. The surgical procedures included 2 cases of type I hybridization, 1 case of type II hybridization, and 2 cases of type III hybridization, and the surgical success rate was 100.0%; see Table 1.
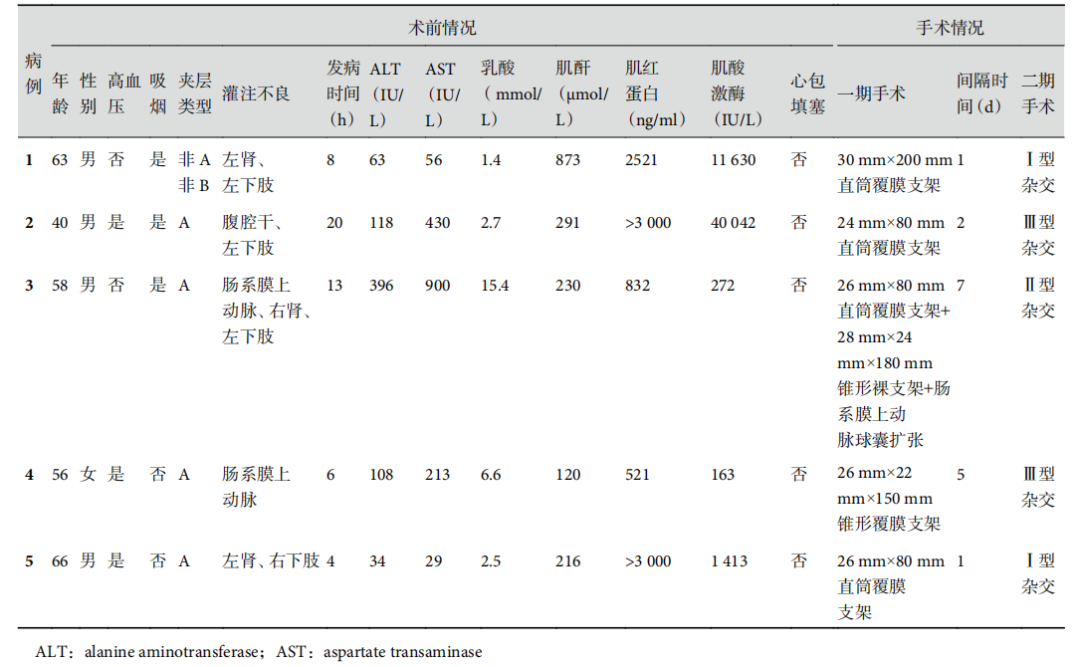
Table 1 Preoperative and intraoperative data of 5 patients
All patients were successfully discharged from the hospital after surgery, with an average hospitalization time of 14.4 d. CTA before discharge showed that the distal malperfusion was completely relieved, and the organ function returned to normal. All patients had no perioperative adverse events such as permanent neurological abnormalities, intestinal ischemic necrosis, osteofascial compartment syndrome, limb necrosis amputation, lifelong renal failure, reoperation and other adverse events, and the 30d survival rate was 100.0%; see Table 2.
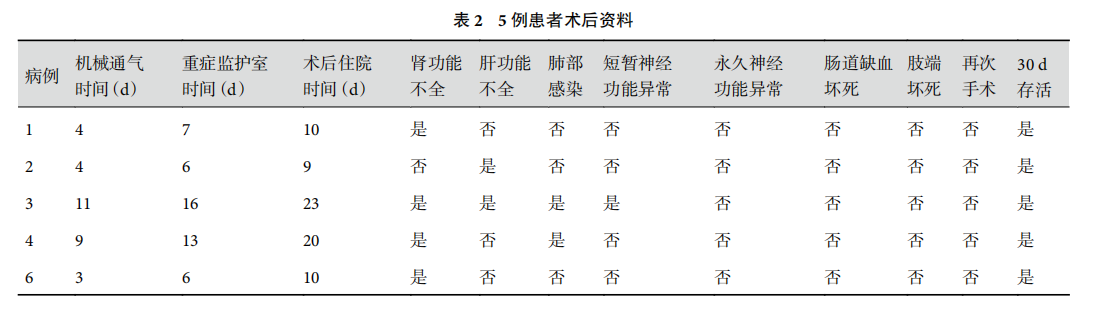
表 2 5 例患者术后资料
05
Discussions
In recent years, the advantages of hybridization in the surgical treatment of aortic coarctation involving the aortic arch have been gradually recognized by more and more colleagues [24-27].Table 2 Postoperative data of 5 patients Reverse staged hybridization technique compared with traditional one-stage repair of the proximal aorta avoids the need to suffer again at the edge of poorly perfused circulatory failure in the organ extracorporeal circulation and deep hypothermia arrest, prioritizing the restoration of distal organ perfusion with minimal hemodynamic manipulation. Then
improve the organ function and correct the internal environment disorder before repairing the proximal aorta by second-stage open surgery, improve the patient's tolerance to second-stage open surgery, and improve the postoperative survival rate. Meanwhile, hybridization surgery can extend the thoracic aortic repair segment and promote benign remodeling of the thoracic aorta in the distant stage [26, 28].
In conclusion, the reverse staged hybridization technique is safe and effective for the treatment of acute aortic coarctation combined with distal malperfusion syndrome involving the aortic arch, but further validation is needed in large-sample clinical studies and long-term follow-up results.
Introduction of experts
References:


