From September 12-14, 2024, the 9th China Vascular Conference (CVC 2024) was successfully held at the Chengdu Century City International Convention Center. During the International and Greater China Region Special Session, Professor Boonprasit Kritpracha from the Songklanagarind Hospital, Prince of Songkla University, Thailand, shared his experience and clinical data on endovascular treatment choices for short-neck or juxtarenal aneurysms.

Short-Neck/ Juxtarenal Abdominal Aortic Aneurysm (AAA)
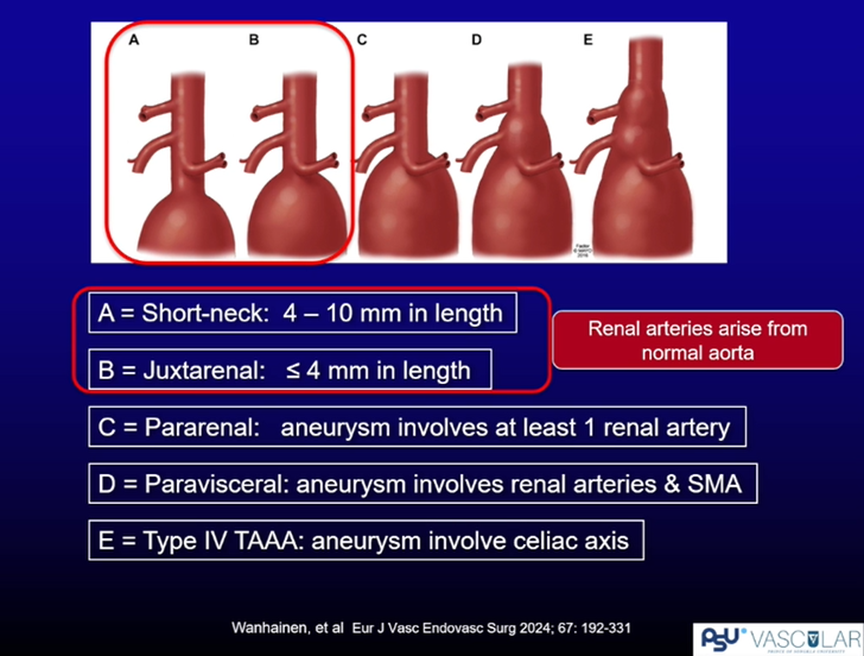
Definition of Short-Neck/Juxtarenal AAA
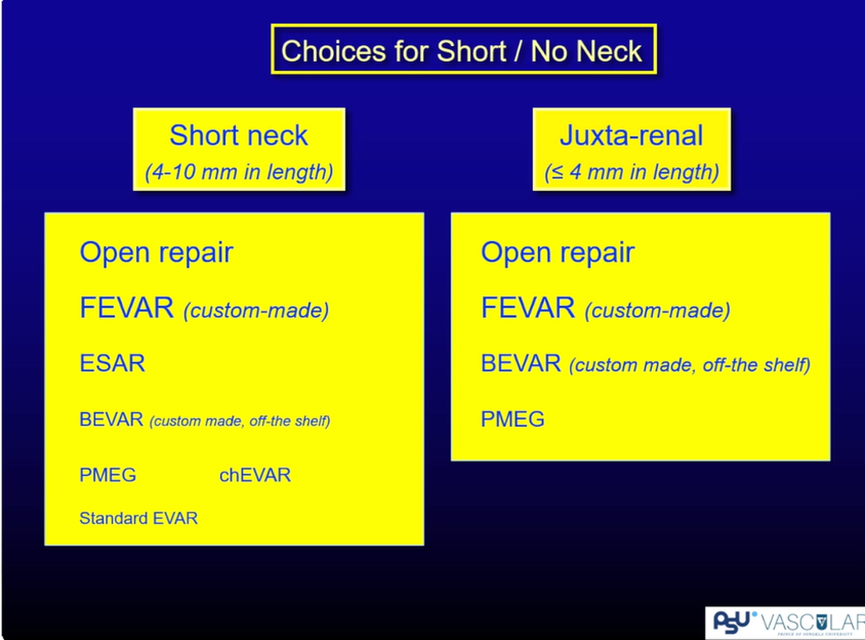
According to the 2024 European Society for Vascular Surgery (ESVS) guidelines on abdominal aortic and iliac artery aneurysms, short-neck is defined as a proximal neck length of 4-10 mm, while juxtarenal is defined as a neck length of ≤4 mm.
Treatment Strategies
For these scenarios, two main approaches are available.
1. Extend the anchoring zone using new stent-grafts (fenestrated devices, branched devices), or surgeon-modified stent-grafts [parallel grafts (chimney), surgeon-modified endografts (PMEG)].
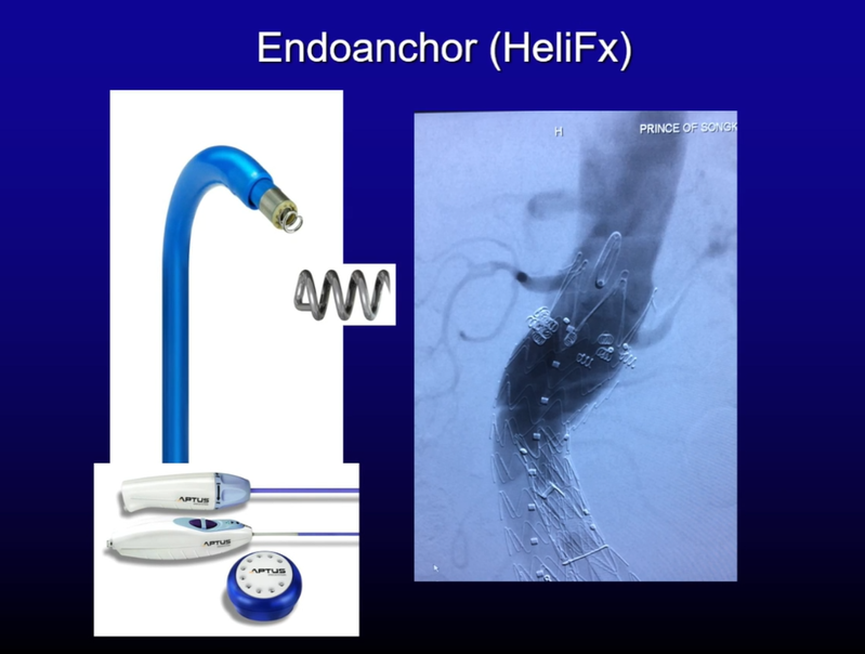
2. Enhance the anchoring zone using Endoanchor. Below is a detailed analysis of the suitability of different treatment options for short-neck or juxtarenal AAAs.
Treatment Strategies for Short-Neck or Juxtarenal AAA
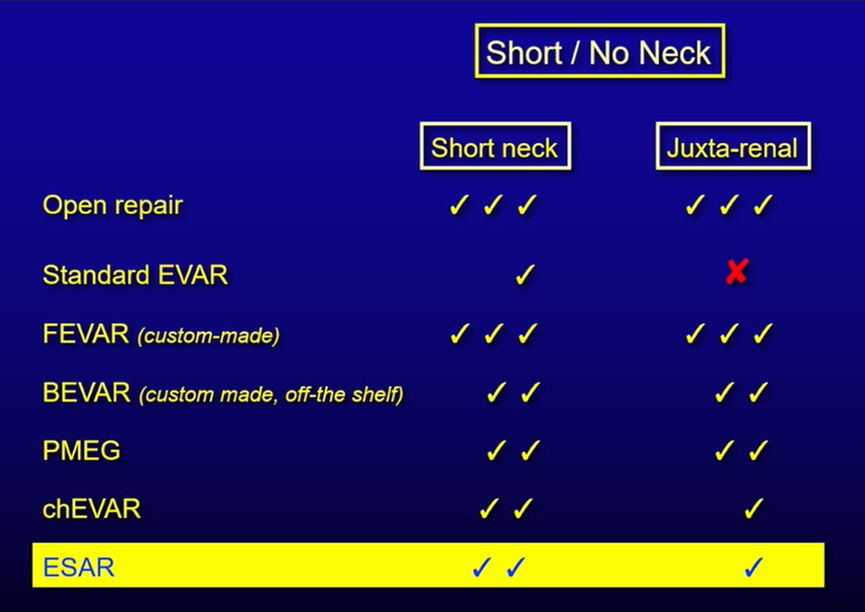
Open Surgery
For short-neck or juxtarenal AAAs, open surgery is still considered a viable treatment option.
Standard EVAR
Standard EVAR may be suitable for short-neck AAAs but is not recommended for juxtarenal AAAs.
Fenestrated EVAR (FEVAR)
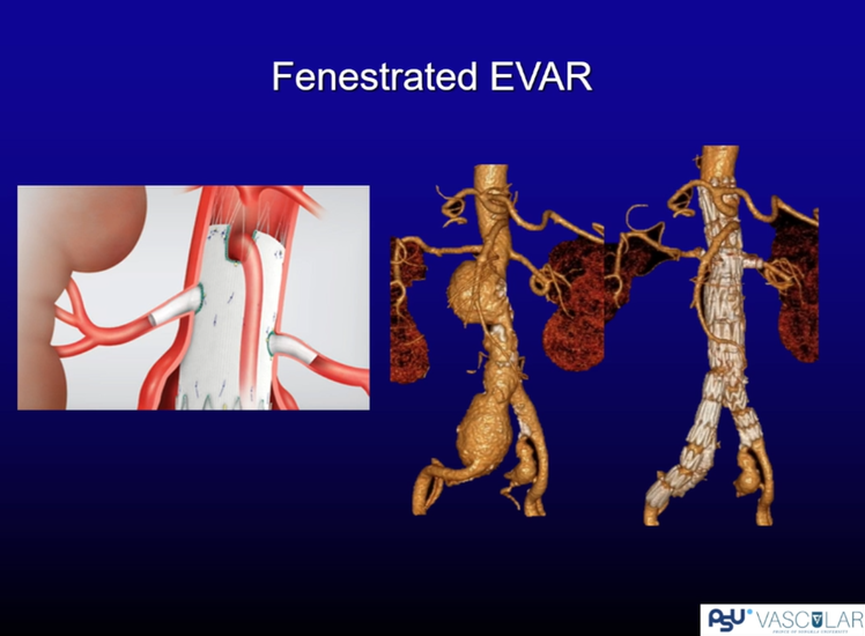
Study 1
A 2021 prospective multicenter study published in J Vasc Surg evaluated the use of the Zenith fenestrated AAA endograft for juxtarenal AAAs. Freedom from AAA-related mortality was 96.8%, and overall survival was 88.8%. There were no aneurysm ruptures or conversions to open repair. However, due to stent design limitations, only 34% of the 195 patients met the anatomical criteria for inclusion.
Study 2
A 2023 single-center study from Germany evaluated mid-term outcomes of fenestrated EVAR in AAA treatment. Among the 349 AAA patients included, 47 (13.5%) had short-neck AAAs, 240 (68.8%) had juxtarenal AAAs, and 62 (17.8%) had suprarenal AAAs. The 30-day mortality rate was 0.9%, with a 5-year survival rate of 69.3% ± 3.1% and a 5-year aneurysm-related mortality rate of 98.8%. The estimated 5-year reintervention-free rate was 86.5%. Moreover, reinterventions did not affect mid-term survival. During the study, the complexity of graft designs increased from 1-2 fenestrations to 3-4, and the average anchoring zone length extended from 22.2 ± 7 mm to 45.3 ± 14 mm by 2019.
Guideline Recommendations
The guidelines recommend considering fenestrated and branched EVAR as a first-line treatment for complex abdominal aneurysms in high-risk patients. However, custom-made devices have stringent criteria and are unavailable in many hospitals/countries.
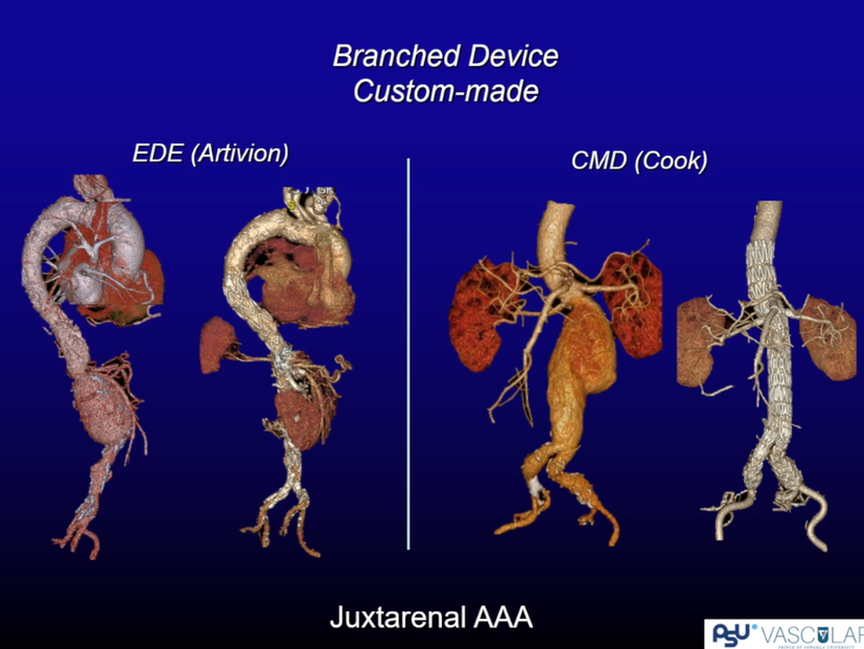
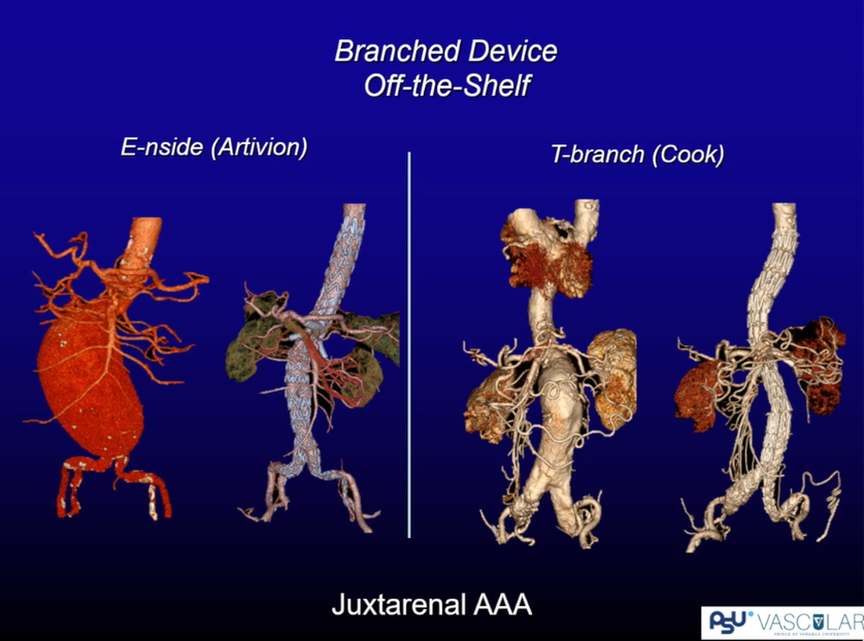
Branched EVAR (BEVAR)
Currently, two types of branched devices are available in Thailand: Inner Branch (Artivion) and Outer Branch (Cook). Custom-made devices are highly tailored to the patient’s anatomy, and a long anchoring zone is not needed. However, for emergencies, off-the-shelf devices can be used. The concern is that stent coverage above the celiac artery increases ischemic risk. Therefore, BEVAR may not be the first choice for short-neck or juxtarenal AAAs.
Customized branch equipment
Finished product branch equipment
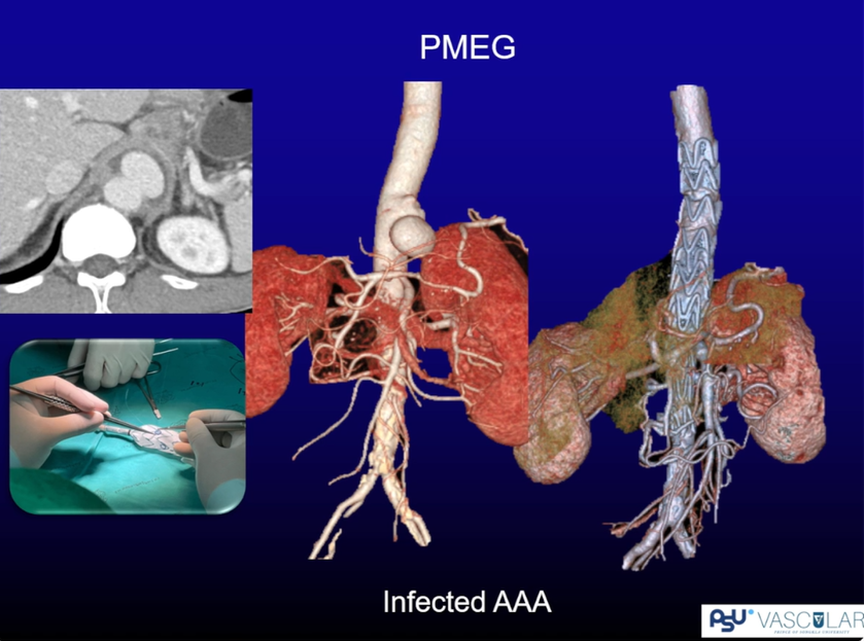
PMEG is a good choice clinically. Professor Boonprasit Kritpracha’s center has treated several cases of infected AAA using PMEG. However, the procedure requires specific equipment and high surgical skills, limiting its use to specialized centers.
Infected AAA
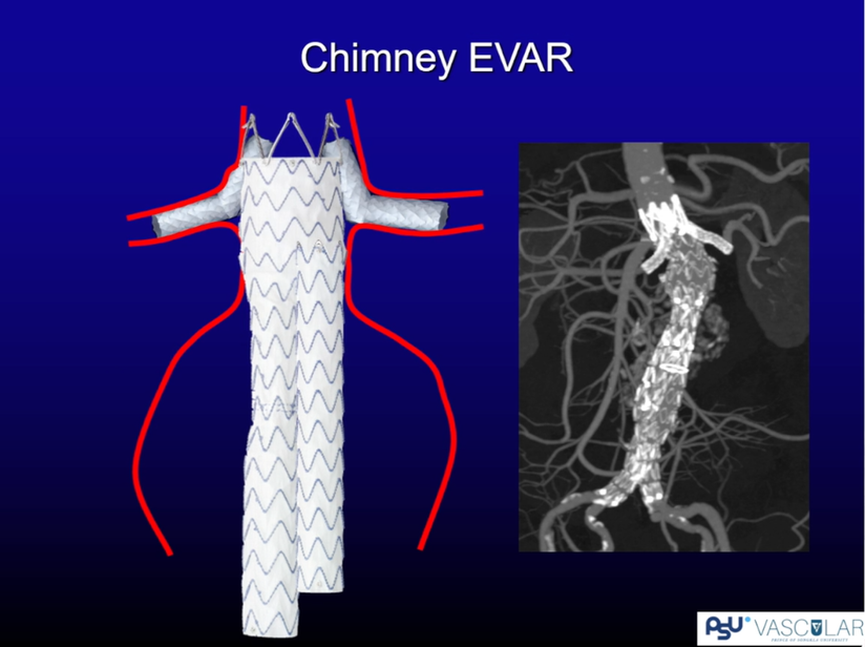
Chimney EVAR (chEVAR)
Research Results
The PERICLES registry, which included 517 patients from nine European and four U.S. centers (2008-2014), showed that 62.2% used Endurant stents and 54.2% used Zenith stents. The average AAA diameter was 65.9 ± 16.5 mm, and the neck length was 4.8 ± 7.4 mm. The theoretical anchoring length increased to 21.1 ± 12.7 mm with the chimney strategy. The technical success rate was 97.1% (502/517) without proximal endoleaks. The 30-day mortality rate was 4.9% (25/517). For ruptured cases, the 30-day mortality rate was 24.1% (7/29), while for elective cases, it was 3.7% (18/488). The 5-year primary patency rate was 90.5%.
Indications for chEVAR
Chimney EVAR is suitable for:
•Open surgery or fenestrated devices are unavailable.
•Emergency cases.
•Juxtarenal AAAs (1-2 renal arteries), ± perirenal (including SMA).
•Neck diameter<30 mm.="">
•Achievable length of ±20 mm.
•Aortic stent-graft oversize by 30%.
•Prefer suprarenal fixation.
The perioperative and long-term results of chEVAR are promising based on current studies.
Guideline Recommendations
Guidelines recommend using parallel grafts (chimney) only in emergency situations or as a bailout strategy, ideally limiting chimneys to ≤2 branches.
ESAR (Endoanchor-Assisted Repair)
ANCHOR Registry
The ANCHOR registry included 319 patients (2012-2013) from 43 centers in the U.S. and Europe. The early results showed high technical and procedural success rates with low reintervention rates.
Further Analysis of Short-Neck Cohort
Among 70 short-neck patients (neck length 4-9 mm) treated with Endurant + EndoAnchor, the 5-year results showed 90% freedom from aneurysm-related mortality and 77% freedom from any secondary procedures. Although the 5-year results are satisfactory, larger-scale follow-up studies are needed.
Summary
There are various treatment options for short-neck or juxtarenal AAAs, including fenestrated devices, branched devices, parallel stents (chimney), and Endoanchor. Choosing the right tool depends on availability, preference, and evidence. Selecting the appropriate strategy is crucial for specific clinical scenarios.


