In recent years, cyanoacrylate closure (CAC) has become a commonly used method for treating saphenous vein trunks. However, CAC still carries the risk of recanalization post-procedure. How should these cases be managed? On September 12, 2024, during the 9th China Vascular Conference (CVC 2024), Takaya Murayama from the Kannai Medical Clinic in Japan shared their center’s strategies for dealing with CAC recanalization.

Treatment Methods
Over the past year, Takaya Murayama’s center treated 25 cases of CAC recanalization (recanalization rate: 7.6%). Among these, 22 cases were treated using sclerotherapy, but 4 cases showed poor results and switched to laser or RF MDPA. Three cases with extensive recanalization were treated directly using laser or RF MDPA.
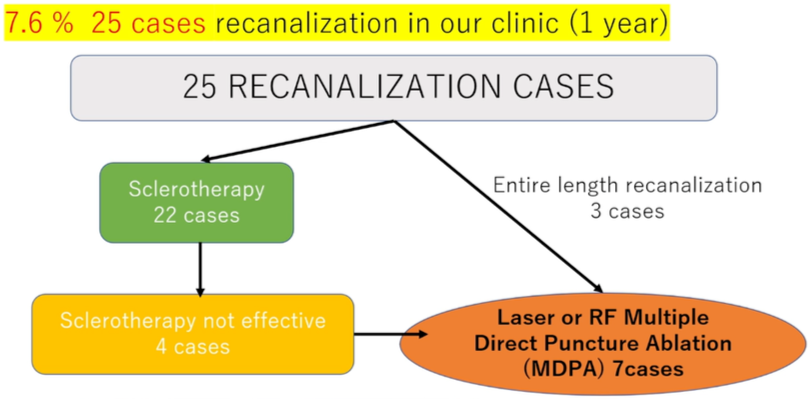
Methods for Treating 25 Cases of CAC Recanalization
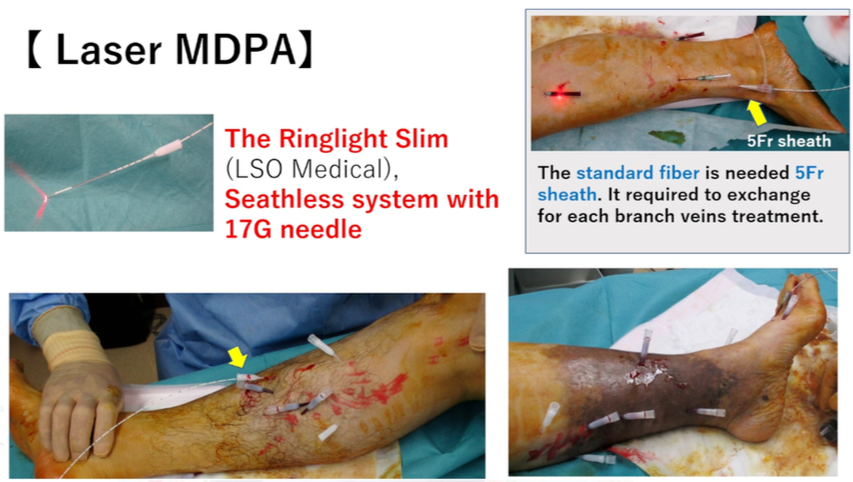
Laser MDPA
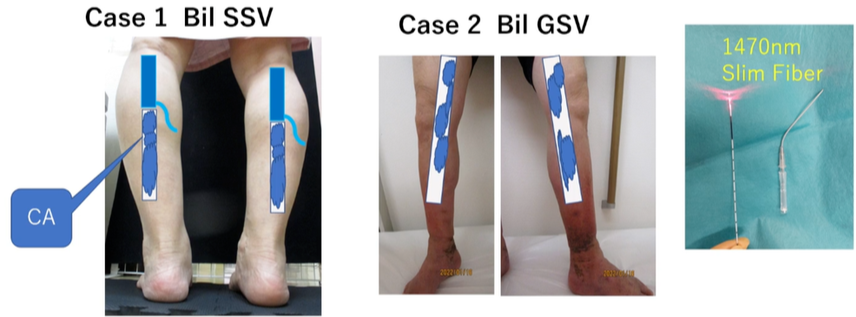
The image below shows the laser MDPA process. A 17G indwelling needle was used for puncture, with a Ringlight Slim laser fiber and a 5Fr sheath. During the procedure, different branch veins were punctured directly.
RF MDPA
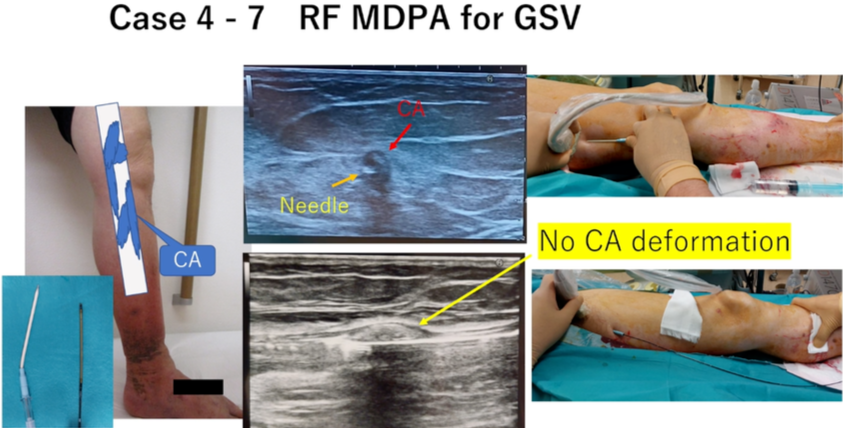
The image below shows the operation process for RF MDPA. During the procedure, the vein wall was ablated segment by segment at 7 cm intervals. The duration was adjusted based on the aneurysm size and depth from the skin.
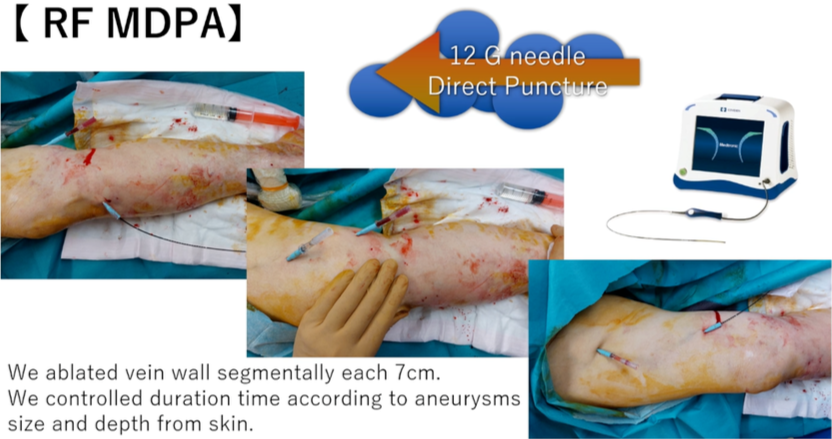
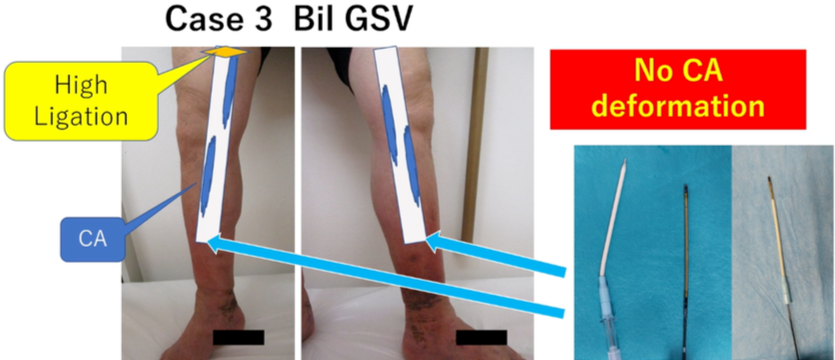
RF Sheathless System
Under ultrasound guidance, a 12G Angiocath indwelling needle sheathless system was used for percutaneous puncture, and the catheter was directly inserted into the vessel.

Case Sharing
Case 1 and Case 2: Treated with laser MDPA, with CA deformation observed during ablation.
Issues with Laser Ablation
Based on these cases, the following potential issues with laser MDPA were identified:
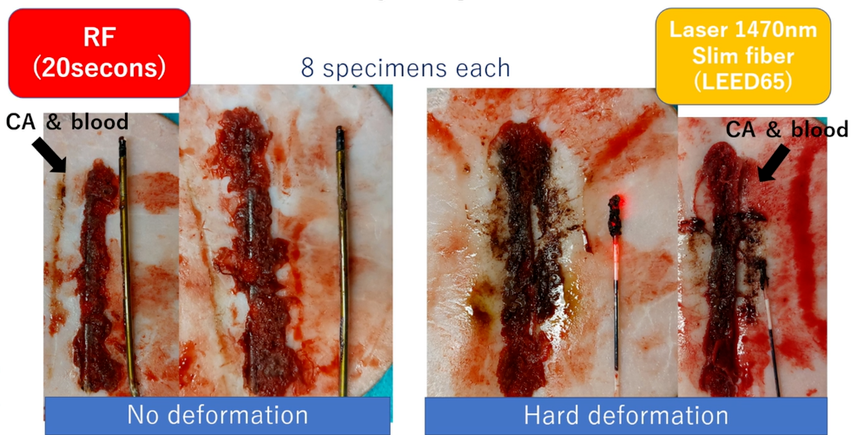
1.CA Deformation During Ablation
CA deformation occurred during laser ablation, so ablation was only performed in areas without CA deformation.
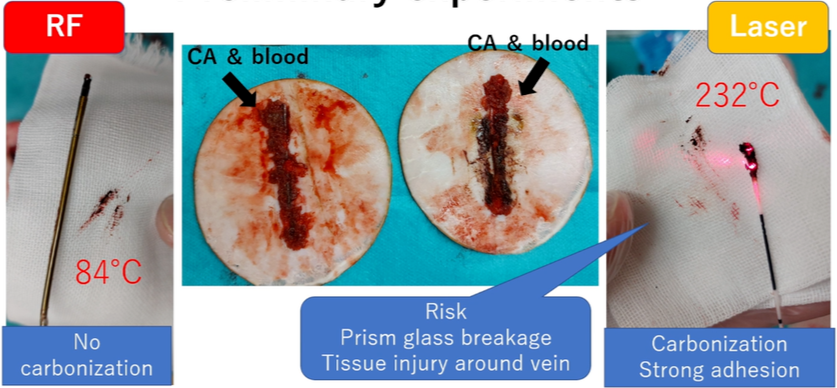
2.Fibrous Prism Glass Breakage
In a study of 5,000 cases, 0.3%-1% of patients experienced fibrous prism glass breakage due to carbonization and adhesion around the prism glass.
Initial Experiment
When comparing laser and RF treatments, it was clearly observed that laser ablation resulted in visible carbonized hard material, while RF treatment caused no deformation or carbonization. The intraoperative temperature of RF was only 84°C, compared to 232°C during laser ablation, which led to carbonization and severe adhesion, increasing the risk of prism breakage and damage to surrounding venous tissue.
RF vs. Laser Comparison
Case Sharing
Cases 3-7: All were treated with RF MDPA for great saphenous vein (GSV) ablation, with no CA deformation observed.
Conclusion
Based on the current experience, laser MDPA may not be suitable for CAC recanalization cases due to the risk of CA deformation. In contrast, RF MDPA appears to be a safe and effective strategy for treating CAC recanalization. Of course, further studies and more cases are needed to confirm this conclusion.


