Aortic coarctation is a relatively common congenital cardiovascular malformation. With the continuous advancement of interventional techniques and the development of new stents, endovascular treatment for aortic coarctation has emerged as a minimally invasive surgical option and has gained widespread clinical application and development in recent years. During the 9th China Vascular Conference (CVC 2024) held in Chengdu from September 12-14, Professor Cherpak Bogdan from the National Amosov Institute of Cardiovascular Surgery shared his team’s research on endovascular treatment for aortic coarctation and its outcomes.

Research Methods
This study included 194 patients with aortic coarctation from 2008 to 2021 to explore the clinical characteristics and treatment response across different age groups. Patient ages ranged from 3 days to 60 years, and they were divided into four groups:
1.Group 1: Infants under 1 year of age (n = 5, average age 3.5 ± 1.6 months).
2.Group 2: Children and adolescents aged 5-18 years (n = 72, average age 13.0 ± 3.8 years).
3.Group 3: Young adults aged 19-25 years (n = 33, average age 22.1 ± 1.9 years, including 4 pregnant women).
4.Group 4: Adults over 25 years of age (n = 84, average age 36.3 ± 0.9 years, including 6 pregnant women).
The morphology of the aortic coarctation was mainly of the interrupted type (67.0%), followed by restenosis (10.3%), aortic arch hypoplasia (9.3%), and aortic coarctation combined with aortic tortuosity (6.2%). The stent designs used included three types: open-loop, closed-loop, and hybrid. Covered stents or bare stents were selected based on the specific morphological characteristics of the coarctation.
Research Results
1.Surgical Outcomes: The success rate of endovascular treatment for aortic coarctation reached 98.9% (n = 189). All patients were discharged in satisfactory condition 3-7 days postoperatively (average 3.4 ± 1.8 days). The procedure significantly reduced the systolic pressure gradient, with an average decrease of 83.9% (from 52.0 mmHg to 8.4 mmHg). Although minor complications occurred, including 2.1% stent migration requiring repositioning and 1.6% access artery loss of pulsation requiring surgical intervention, there were no in-hospital deaths.
2.Long-Term Outcomes: A total of 95.9% of patients (186) were followed long-term. During this period, only 1 patient died due to heart failure, atrial fibrillation, and mitral regurgitation. The overall complication rate was 10.1%, with complications including stent fracture (3.8%), aneurysmal wall dilatation (2.1%), stent migration requiring reintervention (2.1%), and access artery occlusion requiring repair and closure (1.6%). The rarest complication was aorticitis at the stent implantation site, accompanied by pseudoaneurysm and mediastinitis (0.5%).
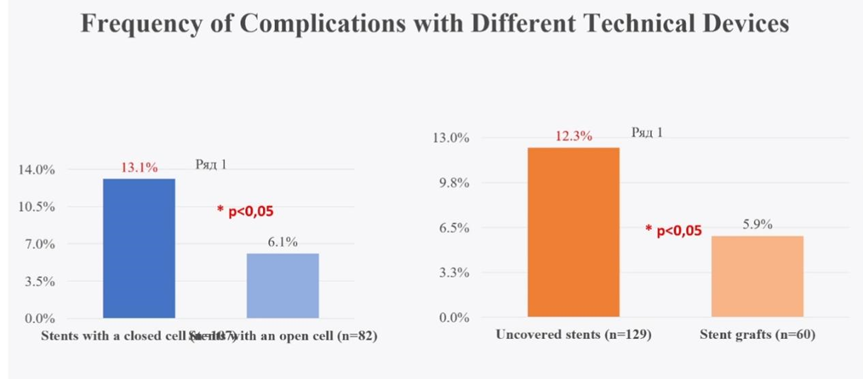
3.Complication Analysis:
•Open-loop stents: 6.1% complication rate.
•Closed-loop stents: 13.1% complication rate.
•Covered stents: 5.9% complication rate.
•Bare stents: 12.3% complication rate.
Different age groups exhibited varying reintervention rates:
•Adults over 25 years: 45% reintervention rate.
•Children and adolescents aged 5-18: 37.2% reintervention rate.
•Young adults aged 19-25: 17.6% reintervention rate.
Additionally, 26.3% of patients were able to reduce their use of antihypertensive medications (from 3 to 2 drugs), demonstrating positive treatment outcomes.
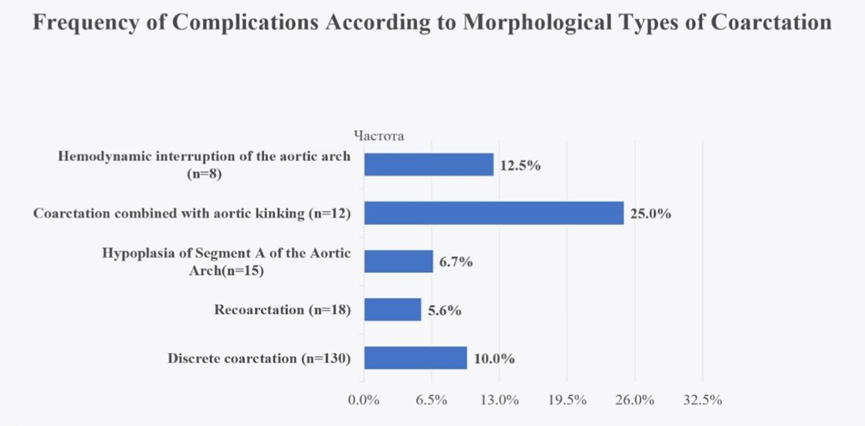
4.Complications by Morphology: The complication rate was lowest for patients with restenosis (5.6%) and aortic arch segmental hypoplasia (6.7%), while patients with aortic coarctation combined with aortic tortuosity had the highest complication rate (25.0%).
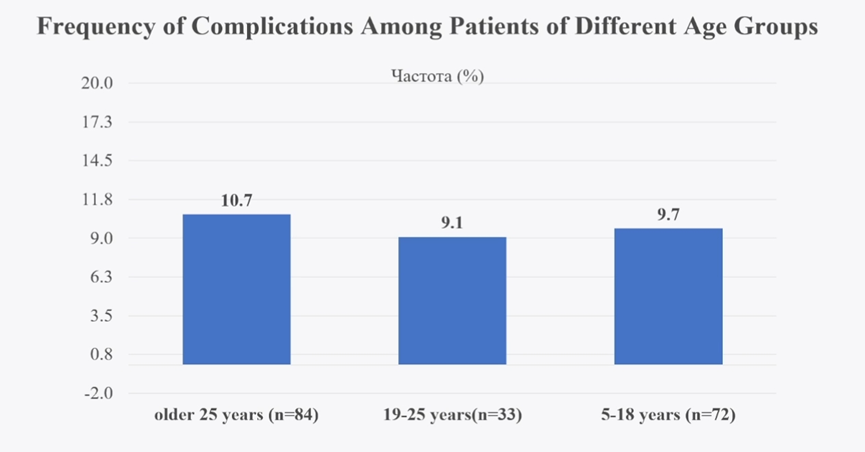
5.Optimal Treatment Timing by Age: Complications increased with age, suggesting that aortic coarctation should ideally be treated promptly after diagnosis. The highest complication rate occurred in patients over 25 years old, potentially reflecting more comorbidities or more complex coarctation morphology in this group. The optimal age for endovascular repair is 19-25 years, as this age group had the lowest reintervention rate (17.6%, P < 0.05) and complication rate (9.1%).
Despite the fact that most patients (73%) did not require reintervention, the reintervention rate was highest in patients over 25 years old (45%, P < 0.05).
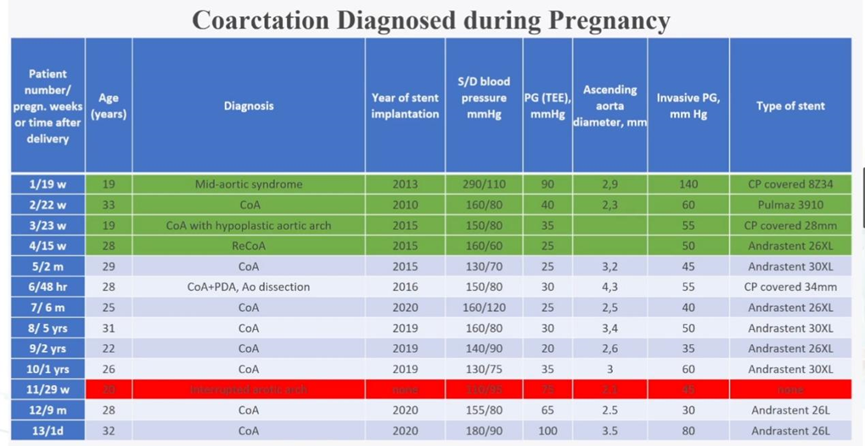
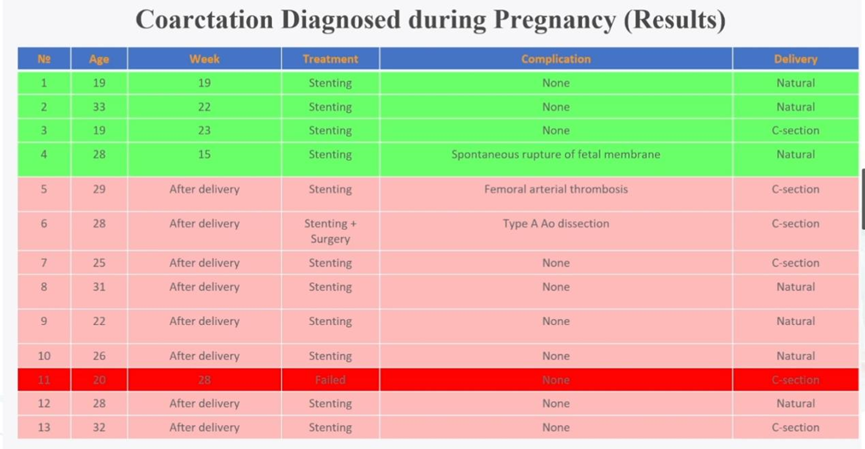
Recommendations for Treating Aortic Coarctation Diagnosed During Pregnancy
Severe primary and recurrent aortic coarctation should be treated before pregnancy. However, endovascular treatment remains a relatively safe and effective option for high-risk pregnant women to prevent life-threatening events.
Conclusion
1.Safety and Efficacy: Stent implantation for aortic coarctation is a safe and effective treatment for patients over 5 years of age, with a procedural success rate of 98.9% and a low complication rate (10%).
2.Favorable Anatomical Conditions: The most favorable anatomical conditions and lowest complication rates were observed in patients with restenosis (5.6%) and aortic arch segmental hypoplasia (6.7%), in contrast to aortic tortuosity (25.0%) and aortic arch flow interruption (12.5%).
3.Optimal Age for Endovascular Repair: Although aortic coarctation should be treated as soon as possible after diagnosis, the optimal age for endovascular repair is 19-25 years, as this group showed the lowest reintervention rate (17.6%, P < 0.05) and complication rate (9.1%).
4.Stent Selection: Open-loop stents are safer than closed-loop stents (complication rates of 6.1% and 13.1%, respectively, P < 0.05). Covered stents are safer than bare stents (complication rates of 5.9% and 12.3%, respectively, P < 0.05). However, due to the need for lifelong anti-inflammatory treatment, covered stents should only be used in severe cases of aortic coarctation, aortic arch segmental hypoplasia, fibromuscular dysplasia, and aortic flow interruption.
5.Pregnancy Considerations: Severe primary and recurrent aortic coarctation should be treated before pregnancy, but endovascular treatment remains a safe and effective option for high-risk pregnant women.


