Endovascular aneurysm repair (EVAR) has become the main treatment for abdominal aortic aneurysms (AAA) due to its advantages of minimal invasiveness, fewer perioperative complications, less blood loss, and shorter hospital stays. However, approximately 44% of EVAR procedures are performed outside of the device’s instructions for use (IFU). This is mainly due to the high proportion of AAAs with complex and challenging neck anatomy in clinical practice. During the 9th China Vascular Conference (CVC 2024) on September 12, Professor Sadik Bilgic from Ankara University School of Medicine in Turkey shared his experience in managing challenging neck AAAs.

Challenging Neck Anatomy Increases Treatment Difficulty
Challenging neck anatomy is defined as having a neck angle >60°, neck diameter ≥28 mm, trapezoidal neck shape, short neck length, or the presence of thrombus or calcification involving more than 50% of the neck circumference. AAA with complex neck anatomy increases the risk of poor EVAR outcomes, including long-term aneurysm rupture or death due to proximal Type I endoleaks, visceral artery occlusion, iliac branch occlusion, increased contrast agent dose and radiation exposure, renal insufficiency, and a higher risk of reintervention. However, compared to open surgery, the morbidity and mortality rates for high-risk patients undergoing EVAR remain lower.
For AAAs with complex neck anatomy, endovascular techniques include standard EVAR, Endoanchors for enhanced proximal fixation, chimney techniques, sac embolization, fenestration, and branched stent-grafts. Compared to other complex endovascular techniques, standard EVAR has a higher risk of endoleak and reintervention, with a greater likelihood of long-term rupture, but it offers lower 30-day mortality, shorter hospital stays, and less blood loss.
Compared to standard EVAR and fenestrated/branched EVAR, chimney EVAR has a higher rate of branch occlusion and a higher incidence of Type I endoleak and aneurysm sac enlargement during follow-up. However, it has shorter operative times, lower contrast agent use and radiation exposure, less blood loss, and a lower risk of early visceral branch thrombosis.
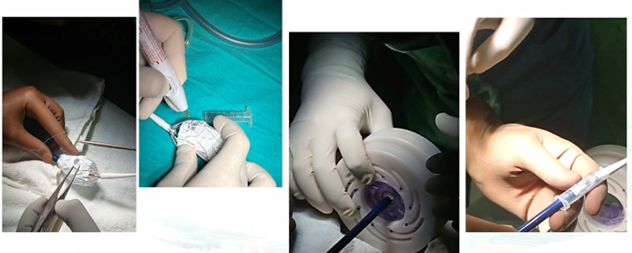
Pre-fenestrated EVAR requires precise preoperative measurements and on-table modifications based on the measurements. This technique currently lacks off-the-shelf stent options and requires modification of existing stents. Surgeon-modified stents have lower rates of endoleak and reintervention, a reduced risk of sac expansion and long-term rupture, a high patency rate for branches, and a high success rate for initial treatment attempts.
Single-Center Data
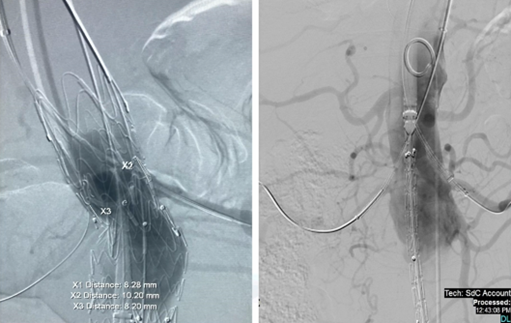
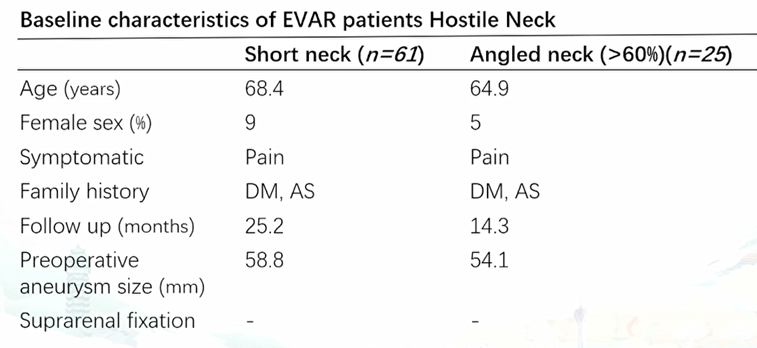
A retrospective analysis was conducted on 68 patients who underwent Ankura stent implantation, of which 61 had short necks and 25 had tortuous necks. In the short-neck group, 4.1% had renal impairment, 72% had hypertension, 14% had diabetes, 48% had coronary artery disease, and 21% had pulmonary disease. In the tortuous neck group, 3.8% had renal impairment, 69.8% had hypertension, 15.2% had diabetes, 54% had coronary artery disease, and 24% had pulmonary disease.
The reintervention rate for the short-neck group due to endoleak was 6.7%. The 30-day endoleak rate for the tortuous neck group was 13.8%, and the long-term mortality rate was 3.8%.
Summary
Overall, challenging neck AAA has a higher rate of reintervention, longer hospital stays, and higher morbidity and mortality following endovascular treatment. Currently, in high-volume centers with experienced practitioners, the use of various endovascular techniques to treat complex neck AAAs is still considered an acceptable alternative to open surgery.