Infected aortic aneurysms are one of the most challenging diseases faced by vascular surgeons. Although they have a low incidence, they are highly aggressive with a very high mortality rate. Infection can lead to the destruction of the aortic wall and the formation of aneurysms, and is often associated with immunocompromised conditions such as diabetes, HIV, end-stage renal failure (ESRF), and steroid use. On September 12, 2024, during the 9th China Vascular Conference (CVC 2024), Professor Benjamin DK Leong from Queen Elizabeth Hospital, Malaysia, shared his experience in endovascular repair of infected aortic aneurysms.

Current Status of Endovascular Treatment for Infected Aortic Aneurysms
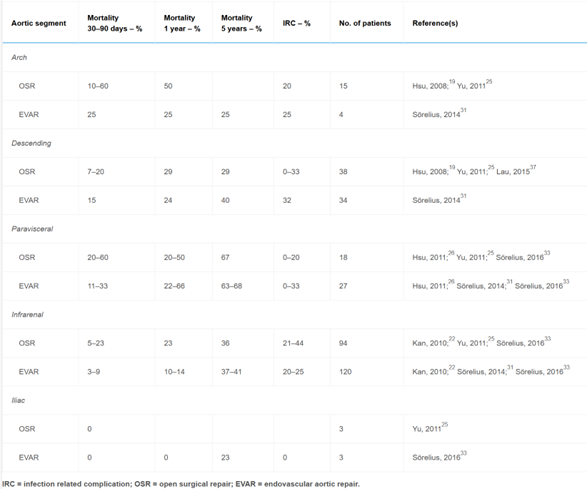
Currently, the gold standard treatment for infected aortic aneurysms remains open surgical repair, including in-situ and extra-anatomic bypass repairs. However, the postoperative mortality rate for open surgery is as high as 44%. For patients who are in poor general condition, have multiple comorbidities, or are unsuitable for open surgery, endovascular repair is also an option.
In 2011, Kripracha et al.[1] reported that for patients without fistula complications, endovascular repair of infected aortic aneurysms provided good short- and mid-term outcomes. However, for patients with fistula complications, the prognosis after endovascular repair was significantly poorer.
In 2018, Chinsakchai et al.[2] found that EVAR for infected abdominal aortic aneurysms (AAA) was feasible, with 38.3% of patients discontinuing antibiotics after an average of 13.4 months. A serum albumin level <3 mg/dL was identified as a factor associated with persistent infection.
In 2019, Sörelius et al.[3] published a systematic review on the management of infected AAAs. The results showed that compared to open surgery, EVAR had higher short-term survival, and similar long-term outcomes. This suggests that EVAR can be considered an acceptable alternative to open surgery. However, infection-related complications remain a significant threat following repair of infected AAAs and require further research. Factors associated with poor outcomes after EVAR include advanced age, rupture, suprarenal aneurysms, and non-Salmonella-positive cultures.
Single-Center Endovascular Repair Results
At our center, there were 42 cases of infected aortic aneurysms treated with endovascular repair, with 1 case (2.3%) converting to open surgery, 4 cases (10%) of aneurysm-related mortality, 5 cases (11.9%) of non-aneurysm-related mortality, and 4 cases (9.5%) requiring reintervention. Perioperative mortality was 4 cases, representing a perioperative mortality rate of 9.5%.
For all cases, if conditions permitted, intravenous antibiotics were administered for 2 weeks prior to intervention. In addition, if there was insufficient anchoring zone, adjunct techniques such as chimney grafts, custom fenestration, surgeon-modified grafts, or hybrid procedures were considered. For fragile tissues, gentle balloon expansion or non-balloon techniques were preferred. Postoperatively, lifelong antibiotic treatment was recommended (minimum 6-12 months).
Microbiological culture results revealed:
•Burkholderia pseudomallei: 26.7%
•Salmonella species: 23.3%
•Klebsiella pneumoniae: 10.0%
•Staphylococcus aureus: 6.7%
•Escherichia coli: 3.3%
•Negative culture results: 30.0%
Affected anatomical sites included:
•Abdominal aorta: 50.0%
•Iliac artery: 23.3%
•Aorta-iliac artery: 3.3%
•Thoracoabdominal aorta: 6.7%
•Thoracic aorta: 10.0%
•IVC/CIV fistula: 6.7%
Case Analysis
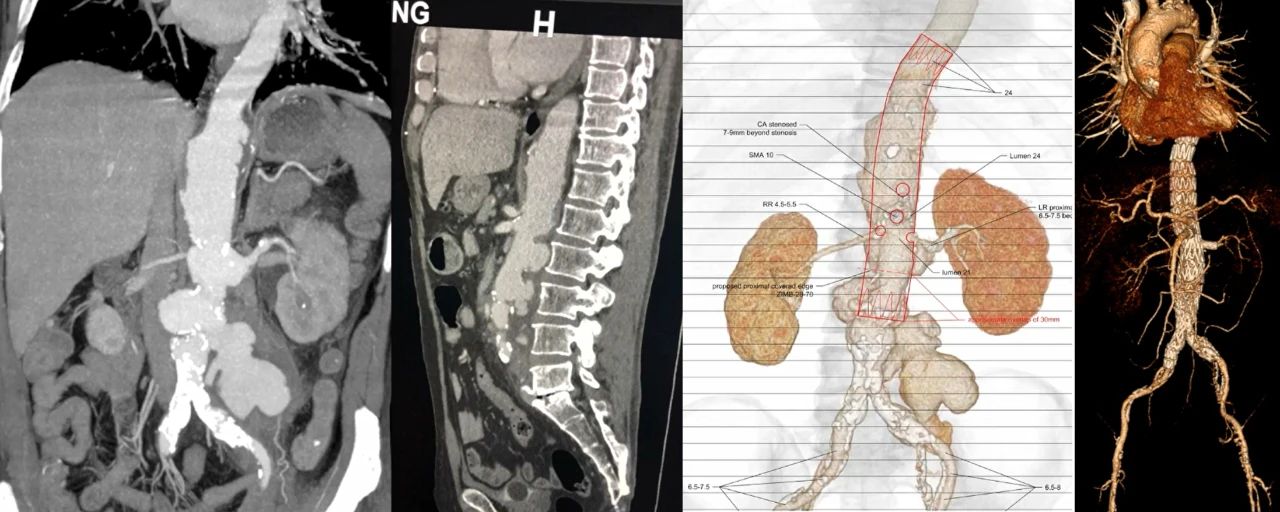
Case 1: A 58-year-old male with a Burkholderia pseudomallei-infected aortic aneurysm complicated by aneurysmal rupture. He underwent an off-pump fenestrated endovascular repair. The patient survived and had no endoleak at the 4-year follow-up.
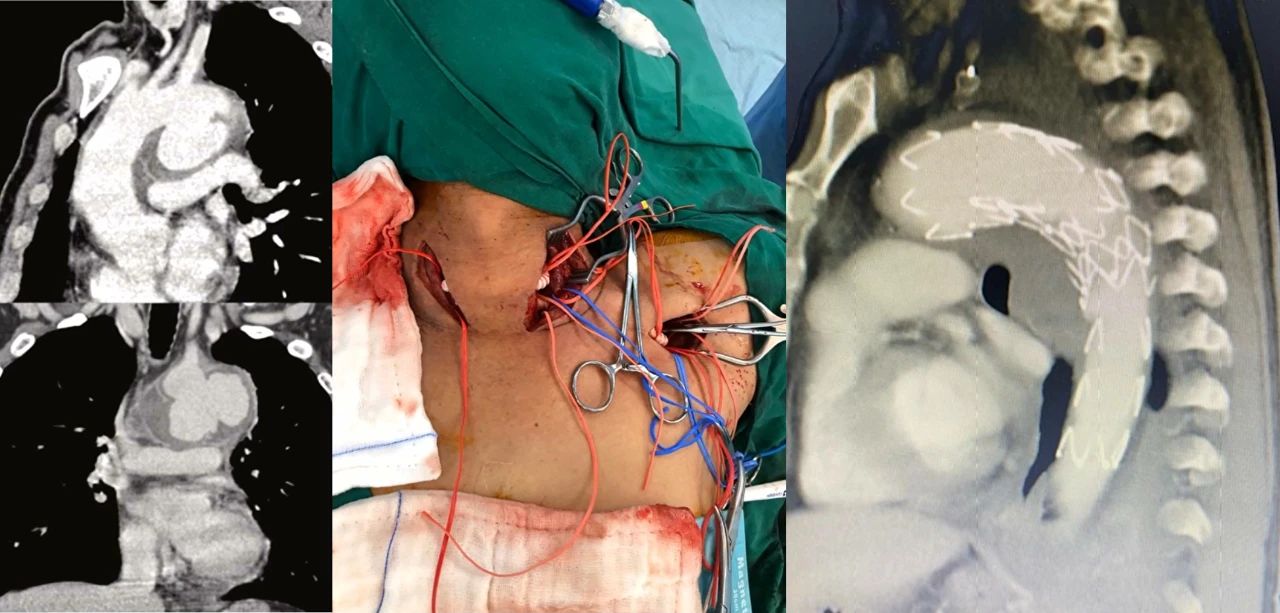
Case 2: A 55-year-old male was admitted with hoarseness and fever. CT imaging revealed an infected aneurysm of the aortic arch. The surgical strategy involved debranching of the aorta combined with TEVAR, neck-to-neck bypass, LCCA-left axillary artery bypass, and LSA embolization. At the 4-year follow-up, the patient was still alive.
Conclusion
Infected aortic aneurysms are a severe type of vascular disease. Endovascular repair for infected aortic aneurysms can achieve good early and mid-term outcomes. Proper preoperative antimicrobial therapy, meticulous endovascular techniques, and well-planned access routes are essential for achieving favorable prognosis.


