During the 9th China Vascular Conference (CVC 2024) on September 12, Professor Wu Ridong from the Department of Vascular Surgery, The First Affiliated Hospital of Sun Yat-sen University, shared his experience in treating a rare case of an abdominal aortic aneurysm in a 4-year-old child.

Case Sharing
Patient Information (Female, 4 years old)
Chief Complaint: Abdominal aortic aneurysm detected for over one month.
Current Medical History: Over a month ago, the child was treated at a local hospital for fever and abdominal pain, presenting with flu-like symptoms. A CT scan revealed an “abdominal aortic aneurysm and left renal cortical thinning.” During hospitalization, the highest blood pressure recorded was 200 mm Hg. After intravenous antihypertensive treatment, the patient was switched to oral spironolactone, captopril, and nifedipine, maintaining blood pressure between 125-142/76-99 mm Hg.
Past Medical History: No history of Kawasaki disease, vasculitis, trauma, surgeries, or catheter placements.
Family History:
•Temperature: 36.6℃
•Pulse: 86 bpm
•Respiration: 20 breaths/min
•SpO₂: 100%
•Blood Pressure: 138-142/85-91 mm Hg (upper limbs), 125-129/83-89 mm Hg (lower limbs).
Abdominal Examination: A pulsatile mass was palpable 3 cm below the left costal margin, but no vascular murmurs were heard.
Laboratory Findings:
•Hypertension-related markers: Renin: 487.5 μIU/mL, Aldosterone: 1750 μIU/mL, Aldosterone/Renin ratio: 3.6 (supine).
•No other abnormalities were found.
•Whole exome sequencing and parental validation did not identify congenital aneurysm-related gene mutations.
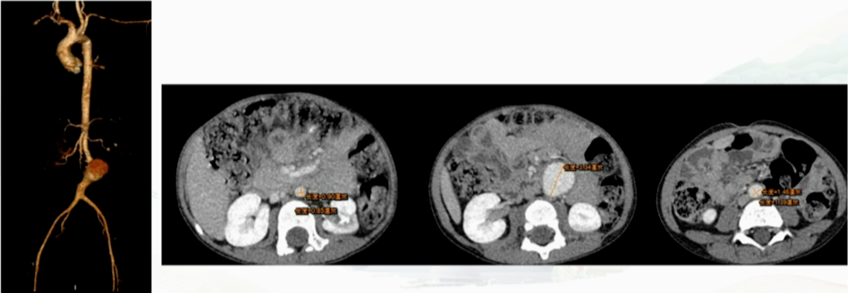
Imaging Examinations:
1.Abdominal CT: Left renal atrophy, left renal artery narrowing, abdominal aortic aneurysm (3.3 cm, eccentric, with calcified plaques).
2.Echocardiography: Mild left ventricular enlargement, suggestive of hypertensive heart disease. No abnormalities in other thoracoabdominal organs or blood vessels.
3.Cranial MRI: Normal.
4.Renography: Left renal atrophy with moderate decline in blood flow perfusion and function, while the right kidney had normal blood flow and function.
Surgical Plan:Following a multidisciplinary team (MDT) discussion involving vascular surgery, pediatric cardiology, pediatric ICU, pediatric surgery, transfusion medicine, anesthesiology, and the operating room staff, the treatment plan for the child’s abdominal aortic aneurysm was finalized. The child’s hypertension was closely linked to left renal artery stenosis. With blood pressure stabilized on medication, the surgical plan was to first address the abdominal aortic aneurysm through aneurysm resection and artificial graft replacement.

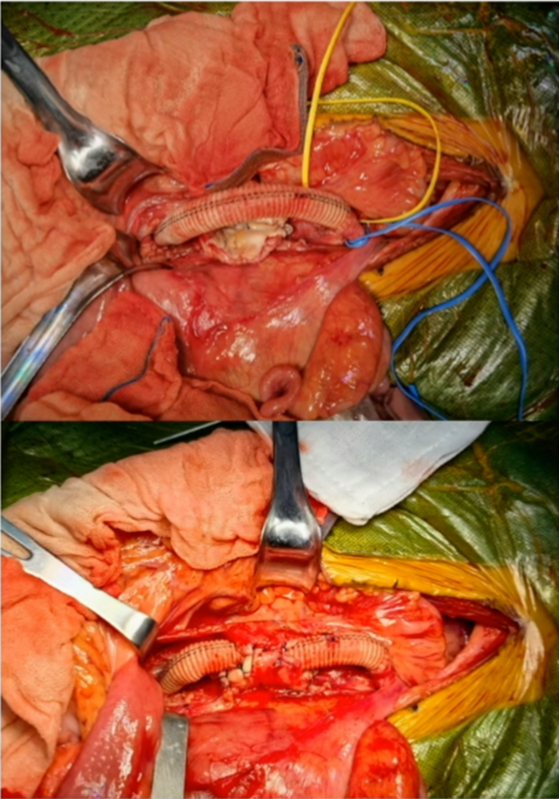
Surgical Procedure
Step 1: A midline abdominal incision was made to expose the aortic aneurysm.
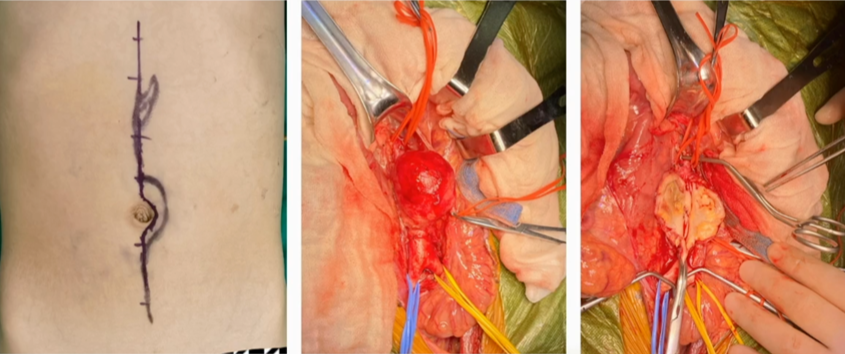
Step 2: Resection of the abdominal aortic aneurysm and replacement with an artificial graft.
Key Points:
•The normal diameter of the child’s aorta was 8 mm. To prevent future stenosis due to growth, a larger artificial graft (12 mm) was selected for anastomosis, with the proximal end modified to a wedge shape to match the native artery.
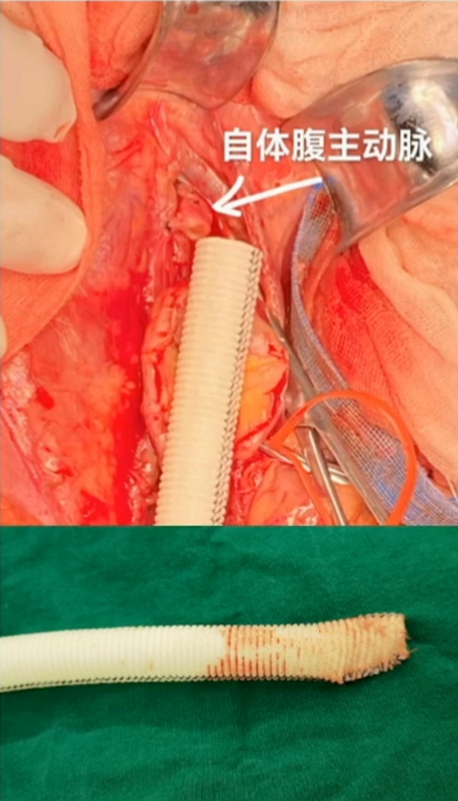
•To allow for future growth, the artificial graft was deliberately curved into a C-shape and secured in place.
Postoperative Follow-Up
Postoperative CTA showed that the artificial graft and anastomosis were patent. The patient has been followed up for 8 months, with good outcomes.

Treatment and Prognosis of Abdominal Aortic Aneurysms in Young Children
Abdominal aortic aneurysms in young children are rare, typically presenting at a very young age with poor tolerance, high surgical trauma, and suboptimal surgical outcomes. According to the literature, the earliest reported case dates back to 1918, and in 1956, Cooley and Taylor reported the first successful surgical case using aneurysm resection and transplantation of a cryopreserved adult iliac artery. From 1975 to 2019, only 70 surgical cases of pediatric abdominal aortic aneurysms were reported worldwide, most as individual case reports. Since 2008, only three studies have reported more than three cases. The largest series was a 2016 JVS article, which retrospectively analyzed 11 cases treated at the University of Michigan Children’s Hospital from 2002 to 2014, with ages ranging from 2 to 6 years.
Summary of Cases:
•Thoracic aortic aneurysm above the celiac trunk: 2 cases.
•Suprarenal abdominal aortic aneurysm: 2 cases.
•Perirenal abdominal aortic aneurysm: 2 cases.
•Infrarenal abdominal aortic aneurysm: 5 cases, maximum diameter 4.1 cm.
•Surgical approaches included aneurysm resection, thoracoabdominal bypass, open aortic closure + aortic reconstruction, closed aortic closure + double renal reimplantation + aortomesenteric bypass, aneurysm resection + infrarenal aortic reconstruction, and aortoiliac bypass.
Etiological Analysis:
•Idiopathic or congenital dysplasia: 7 cases.
•Tuberous sclerosis: 1 case.
•Trauma: 2 cases.
•Umbilical artery catheterization with infection: 2 cases.
Treatment Outcomes:
•Perioperative mortality: 1 case (preoperative heart and renal failure).
•Graft occlusion: 2 cases (1 month and 3 years postoperatively).
•The remaining cases had no aortic reconstruction-related complications.
•Follow-up of 10 cases, average follow-up of 4.9 years, indicating that pediatric abdominal aortic aneurysm treatment remains a complex and challenging field.
Single-Center Experience at The First Affiliated Hospital of Sun Yat-sen University
From August 2007 to April 2024, the hospital accumulated experience with 5 pediatric abdominal aortic aneurysm cases, with the first successful surgery completed on August 20, 2007.

Three patients have been followed for over 15 years. Specific details are as follows:
•Case 1: Detected in 2008 with a maximum diameter of 8.9 cm, underwent Y-shaped graft replacement. In 2019, the graft remained patent.

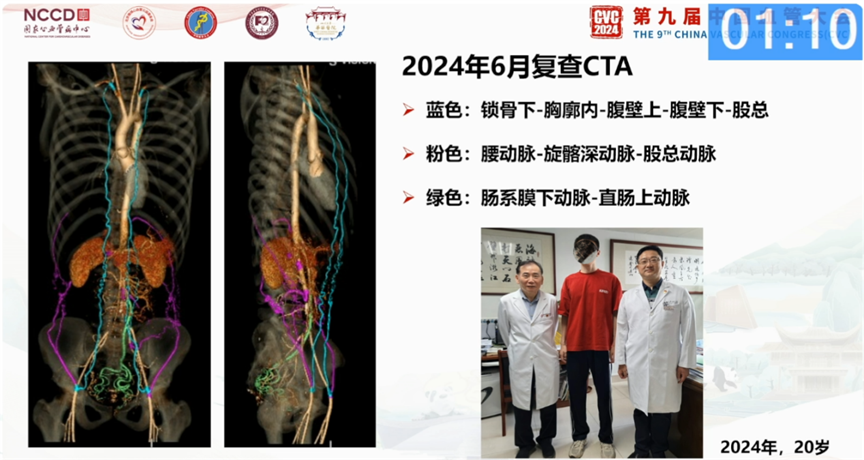
•Case 2: Detected in 2007 with a maximum diameter of 4.48 cm, underwent Y-shaped graft replacement. At 20 years old (June 2024), the graft was occluded, but collateral circulation was well-established.

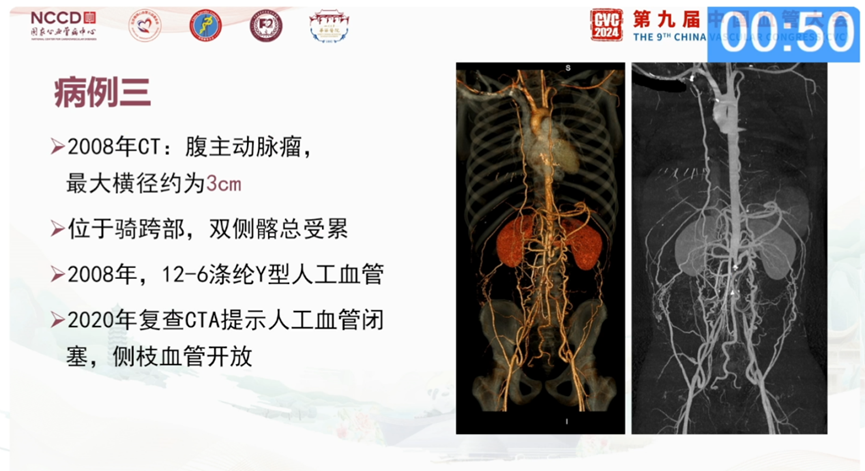
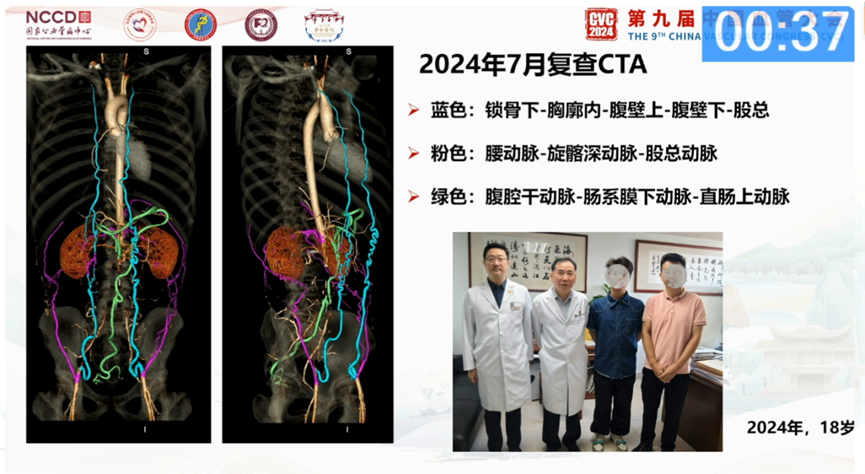
•Case 3: Detected in 2008 with a 3 cm aneurysm affecting both common iliac arteries. Underwent Y-shaped graft replacement. In 2020, CTA showed graft occlusion but open collateral vessels.
Conclusion
Pediatric abdominal aortic aneurysms are rare, and treatment primarily depends on open surgery. Selecting slightly larger diameter and longer grafts is recommended to accommodate future growth. Although long-term follow-up may reveal graft occlusion, no lower limb ischemia has been observed, likely due to effective collateral circulation. Whether to replace the graft in adulthood remains controversial and should be decided based on individual circumstances and clinical presentation.


