During the 9th China Vascular Conference (CVC 2024), held on September 12, 2024, at the Chengdu Century City International Convention Center, the annual Top 10 Case Showcase of the Vascular Surgery Group of the Chinese Clinical Case Database was successfully held. Numerous surgical experts provided in-depth analysis and experience sharing on the selected top 10 cases. Dr. Pu Zuo from the Vascular Surgery Center of Fuwai Hospital, Chinese Academy of Medical Sciences, introduced their experience in using a concave branched stent system to treat an aortic arch aneurysm.

Research Background and Advances
Open surgery for aortic arch diseases poses significant challenges due to its complexity and risks. Even after excluding acute aortic syndromes, the in-hospital mortality and postoperative permanent neurological dysfunction rates for arch surgeries (including hybrid procedures) remain high at 11.1% and 5.6%, respectively. For elderly patients and those with multiple comorbidities, open surgery is often not feasible. Minimally invasive treatment for arch pathologies can improve prognosis and provide a safe and effective alternative for patients who cannot tolerate open surgery. Despite decades of development in endovascular therapy for aortic diseases, especially with significant progress in treating descending aorta and single-branch pathologies, endovascular treatment for aortic arch lesions remains a technical challenge that requires further innovation and breakthroughs.
Current commonly used aortic arch stents have the following limitations:
1.Primarily rely on custom designs, leading to prolonged waiting times, increased costs, and limited applicability.
2.Inability to achieve complete endovascular three-branch reconstruction.
3.Most stents require operation within an ischemic window in the aortic arch, which is technically demanding and increases the risk of cerebral infarction.
Therefore, developing more advanced aortic arch stents and endovascular techniques is crucial for improving outcomes and reducing surgical risks.
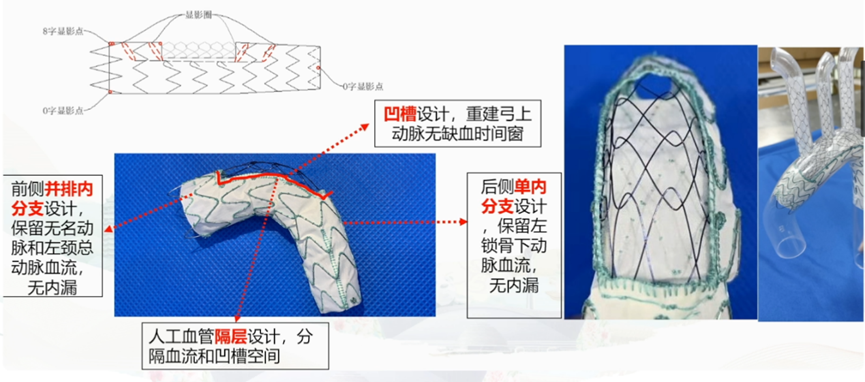
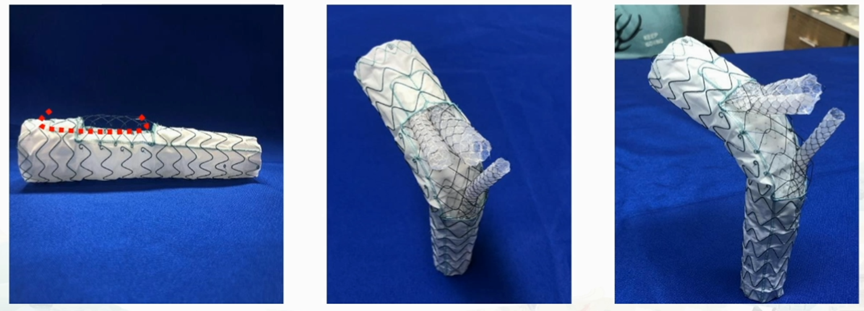
Since 2011, Professor Shuchang’s team has led the design and development of the C-S Integrated Aortic Arch Three-Branch Reconstruction System (Concave Supra-arch Branched Stent-Graft), which has been patented and successfully completed animal experiments. This innovative concave stent system design can effectively reconstruct the aortic arch branches endovascularly without interrupting cerebral blood flow and does not require patient-specific customization, offering broad clinical application potential. Key features of the stent system include:
1.Concave Design: Reconstructs supra-aortic arteries without an ischemic window.
2.Artificial Graft Partition Design: Separates blood flow and the concave space.
3.Parallel Inner Branches on the Anterior Side: Maintains blood flow to the innominate artery and left common carotid artery without endoleak.
4.Single Inner Branch on the Posterior Side: Maintains blood flow to the left subclavian artery without endoleak.
Case Sharing
Patient Information (Male, 51 years old)
Chief Complaint: Aortic arch aneurysm detected for over five years.
Past Medical History: Diagnosed with pulmonary tuberculosis 8 years ago.
Social History: Long-term history of smoking and alcohol consumption.
Diagnosis: Aortic arch aneurysm; hypertension; inactive pulmonary tuberculosis.
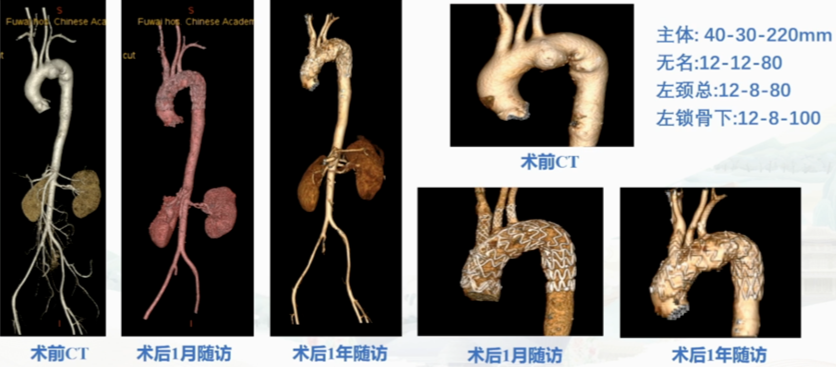
Preoperative CTA: Aortic arch aneurysm, maximum diameter 5.12 cm.

Key Surgical Steps
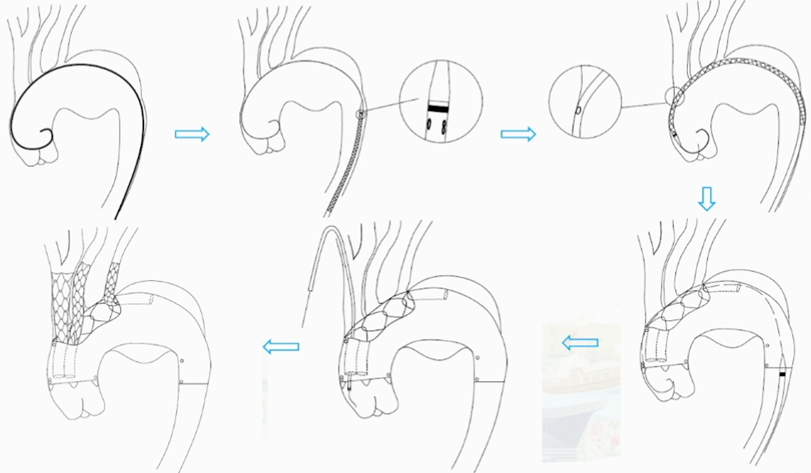
1.Establish vascular access.
2.Guidewire navigation through the aortic lesion to facilitate subsequent stent delivery.
3.Deploy the CS main body stent along the guidewire.
4.Deploy three internal branched stents sequentially within the concave slots of the main stent.
5.Stent Positioning and Deployment.
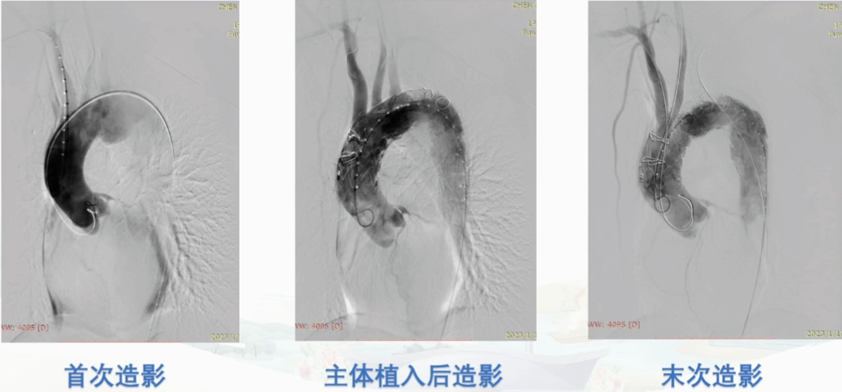
Postoperative Follow-Up
The patient had good follow-up results 1.5 years postoperatively, with imaging showing no stent migration or endoleak, and the aneurysmal sac had shrunk.
Preoperative Evaluation Criteria
1.Indications
•Involvement of the aortic arch (aortic arch aneurysm, aortic dissection, aortic ulcer, and aortic intramural hematoma).
•Proximal anchoring zone length ≥15 mm.
•Good supra-aortic and femoral artery access.
•Proximal anchoring zone diameter range: 25-45 mm.
2.Contraindications
•Severe calcification or mural thrombus in the anchoring zone, potentially hindering stent wall apposition.
•Severe stenosis, calcification, or tortuosity in the access vessels, affecting delivery system entry.
•Systemic or local infection increasing the risk of graft infection.
•Contrast allergy or renal impairment prohibiting the use of contrast agents.
•Connective tissue disorders, such as Marfan syndrome.
•Severe organ dysfunction that may prevent tolerance of surgery.
•Other contraindications as determined by the surgeon.
Perioperative Management Points
1.Surgical Access:
•Right brachial artery incision—Innominate artery branch access.
•Left brachial artery incision—Left subclavian artery branch access.
•Left carotid artery incision—Left common carotid artery branch access.
•Unilateral femoral artery incision—Main body stent access.
2.Anesthesia Access:
•Contralateral femoral artery or dorsalis pedis artery for pressure monitoring.
•Right jugular vein or subclavian vein for CVC.
3.Positioning: Cross-shaped positioning with exposure of the left neck.
4.Postoperative Anticoagulation: Low-molecular-weight heparin for 3 days; dual antiplatelet therapy for 1 year.
5.Follow-Up Schedule: Clinical follow-up before discharge and at 1, 6, and 12 months postoperatively.
Follow-Up Assessments:
•Imaging (CTA/MRI at discharge, 6 months, and 1 year).
•Adverse events (all-cause mortality, myocardial infarction, cerebral infarction, paraplegia).
•Concurrent medication use.


