During the 9th China Vascular Conference (CVC 2024), held on September 12, 2024, at the Chengdu Century City International Convention Center, the annual Top 10 Case Showcase of the Vascular Surgery Group of the Chinese Clinical Case Database was successfully held. Numerous surgical experts provided in-depth analysis and experience sharing on the selected top 10 cases. Professor Shi Xiaoxi from the First Affiliated Hospital of China Medical University shared a case of an infected ruptured abdominal aortic aneurysm complicated by necrotizing fasciitis of the right lower limb.

Case Sharing
Patient Information (Male, 66 years old)
Chief Complaint: Fever with low back pain for 1 month, right lower limb swelling for 2 days.
Current Medical History: The patient experienced intermittent fever for 1 year, with worsening fever over the past month, reaching a maximum of 38°C. This was accompanied by low back pain, which the patient attributed to “lumbar disc herniation” and did not seek treatment for. Two days prior, the patient developed spontaneous swelling of the right lower limb with skin cyanosis and visible tension blisters, without other associated symptoms.
Past Medical History: The patient had a history of diabetes, which was well controlled. He denied any history of surgeries or contact with livestock. Brucellosis testing at a local hospital was negative.
Additional Tests:
1.CTA: Pseudoaneurysm rupture of the abdominal aorta with a right psoas muscle abscess and compression and stenosis of the right iliac artery.
2.Lower Limb Duplex Ultrasound: Significantly reduced arterial blood flow in the right lower limb and deep vein thrombosis (DVT) in the right lower limb.
3.Laboratory Tests: Prior to admission, white blood cell count, C-reactive protein, procalcitonin, and other inflammatory markers were significantly elevated.

Diagnosis and Treatment
1.Emergency Management: Right lower limb venous thrombosis and arterial DVT were detected. To prevent fatal pulmonary embolism, an inferior vena cava filter was placed on the 5th day after admission.
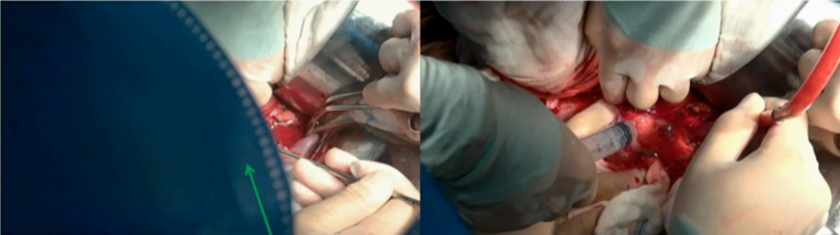
2.Surgical Management on Day 6: Under general anesthesia, abdominal aortic aneurysm resection with Y-shaped graft replacement, local debridement, antibiotic irrigation, and omental plasty were performed. A large amount of ascitic fluid was observed intraoperatively, and samples were sent for bacterial culture and Levinthal test.
3.Simultaneous Burn Surgery: Right lower limb wound debridement and wound repair were performed by the burn unit. The patient was transferred to the ICU for one day and then returned to the vascular surgery ward for further treatment. On the 3rd postoperative day, pus culture results indicated Candida tropicalis, Gram-positive cocci, Gram-negative bacilli, and Acinetobacter baumannii. Sensitive antibiotics were adjusted accordingly.
4.Worsening of Lower Limb Necrosis (Necrotizing Fasciitis): Local incisions were made, and daily dressing changes were performed in conjunction with the burn unit. The posterior thigh muscles, knee, lower calf, and ankle skin gradually showed normal wrinkling, and sensory and motor functions were gradually restored. The patient’s temperature stabilized.
5.Transfer for Skin Grafting Surgery: The patient was transferred to an external hospital specializing in burn surgery for skin grafting, and the right lower limb healed well. The patient continued rehabilitation exercises post-discharge and has since fully recovered.
Vascular Surgery Procedure
Procedure 1: Mesenteric blockade with lidocaine, ligation of the inferior mesenteric vein, and dissection and ligation of the lymphatic vessels.

Procedure 2: Dissection of the left renal vein, clamping of the aneurysmal neck, and dissection and clamping of the bilateral external iliac arteries.
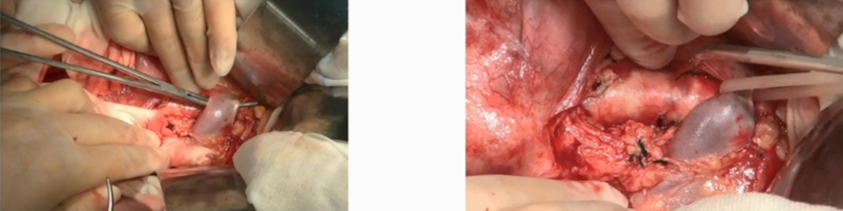
Procedure 3: Incision into the aneurysmal sac revealed a large amount of pus, which was collected for culture.
Procedure 4: Exploration of the aneurysmal cavity showed severe wall calcification. The orifices of the bilateral common iliac arteries were ligated.
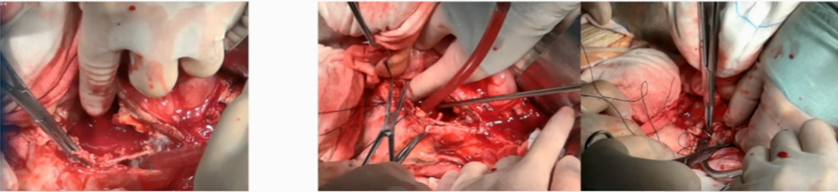
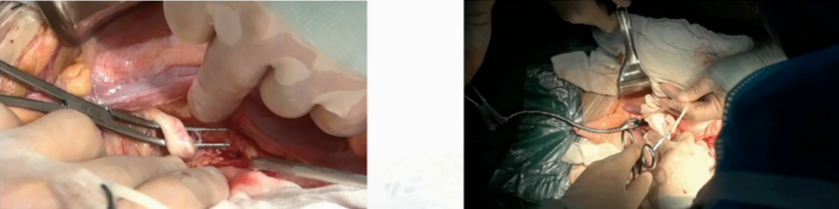
Procedure 5: Irrigation with hydrogen peroxide, followed by irrigation with vancomycin, metronidazole, and rifampicin.

Procedure 6: The proximal anastomosis of the rifampicin-soaked artificial graft was completed. Multiple antibiotics were applied locally at the proximal anastomotic site using hemostatic cotton and biological glue.
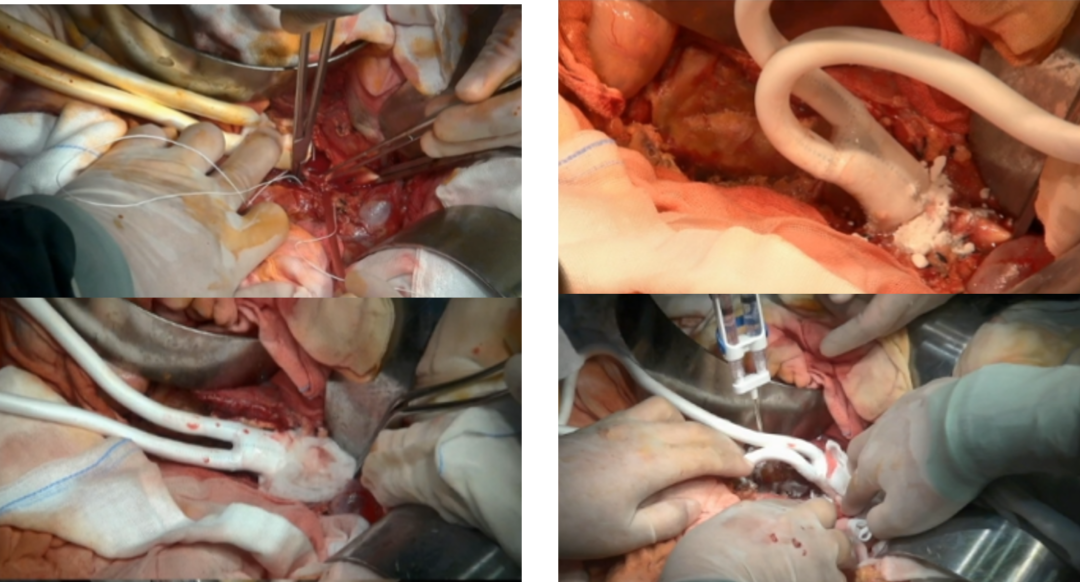
Procedure 7: Distal anastomoses on both sides were completed, and antibiotics were applied again at the distal anastomotic sites.

Procedure 8: Omental plasty (wrap-around omentoplasty of the artificial graft).

Summary
This case of an infected abdominal aortic aneurysm had an insidious onset and atypical clinical symptoms.
During treatment, the patient presented the following characteristics:
1.Multi-Pathogen Infection: Multiple pathogens were detected through multi-site sampling, with four different pathogenic bacteria confirmed.
2.Multiple Complications: The patient developed multiple complications during the course of the disease.
3.Multimodal Treatment Approach: Management involved a multidisciplinary approach, including vascular surgery, burn surgery, and infection management.
4.Use of Multiple Therapeutic Agents: Various drug regimens were administered through multiple routes, including abdominal, lower limb, and intravenous administration.
With comprehensive treatment, the patient was successfully cured and has fully recovered.


