During the 9th China Vascular Conference (CVC 2024), held on September 12, 2024, at the Chengdu Century City International Convention Center, the annual Top 10 Case Showcase of the Vascular Surgery Group of the Chinese Clinical Case Database was successfully held. Numerous surgical experts provided in-depth analysis and experience sharing on the selected top 10 cases. Professor Liu Yu from the Cardiac and Great Vessels Surgery Department at West China Hospital of Sichuan University shared a case of Type A aortic dissection with malperfusion.

Case Sharing
Patient Information (Male, 51 years old)
Chief Complaint: Chest pain for 7 hours.
Past Medical History: Diagnosed with hypertension for one year, with a maximum blood pressure of 180/? mmHg, irregular medication use.
Physical Examination:
• Temperature: 36.6℃
• Pulse: 101 bpm
• Respiration: 18 breaths/min
• SpO₂: 97%
• Blood Pressure:
• Left upper limb: 155/59 mmHg
• Right upper limb: 143/66 mmHg
• Left lower limb: 97/38 mmHg
• Right lower limb: blood pressure unobtainable.
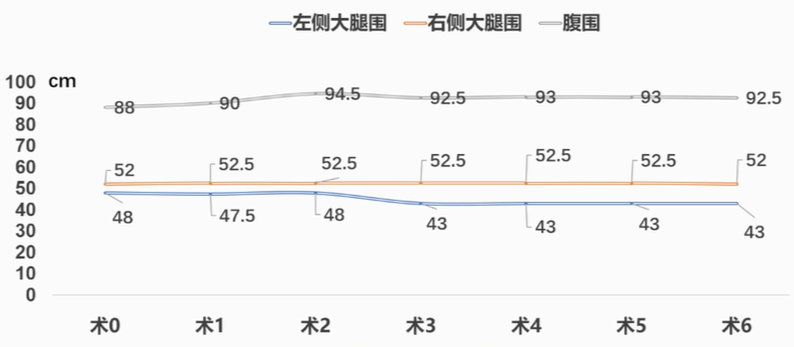
General Condition: Conscious, slightly distended abdomen without tenderness or rebound pain, reduced skin temperature in both lower limbs, weakened dorsalis pedis pulse in the left lower limb, and absent dorsalis pedis pulse in the right lower limb. Bilateral upper limb muscle strength was grade 5, while lower limb muscle strength was grade 2.
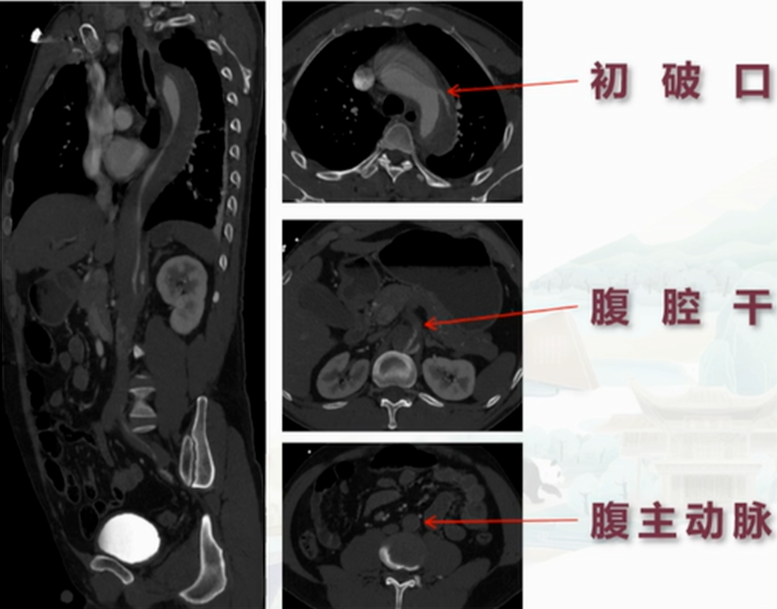
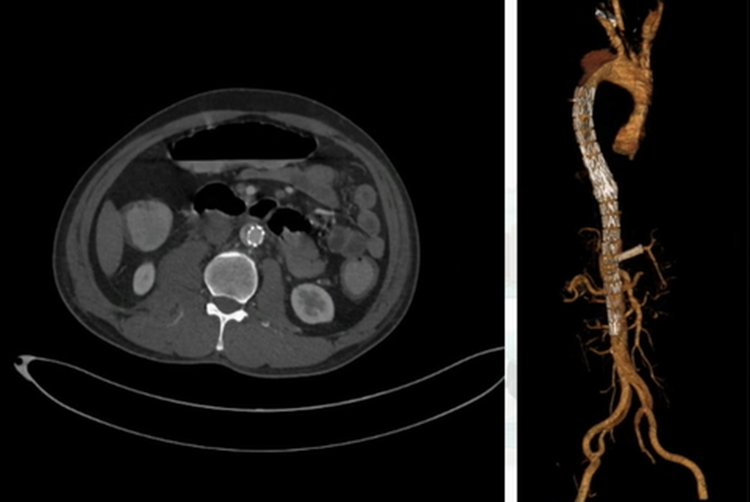
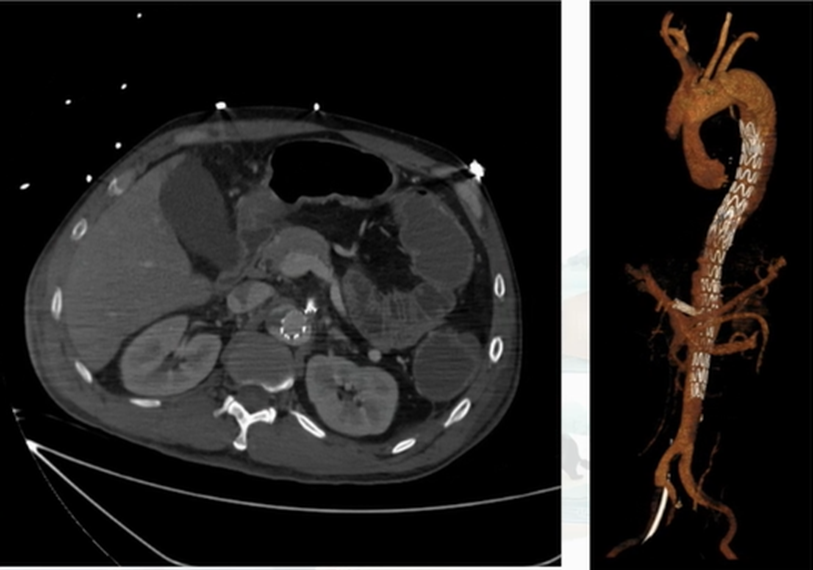
Dissecting Aneurysm CT Angiography: Aortic dissection originating from the ascending aorta, involving all three arch branches, and extending downwards to the bilateral common iliac arteries. The true lumen was small, while the false lumen was large. The right common iliac artery and internal iliac artery were poorly visualized. The celiac trunk and superior mesenteric artery originated from a mixed lumen, with multiple thrombi in the false lumen.
Blood Gas Analysis:
• pH: 7.156
• Lactic acid: 12.40 mmol/L
• BE: -17.1 mmol/L
• Bicarbonate: 10.4 mmol/L.
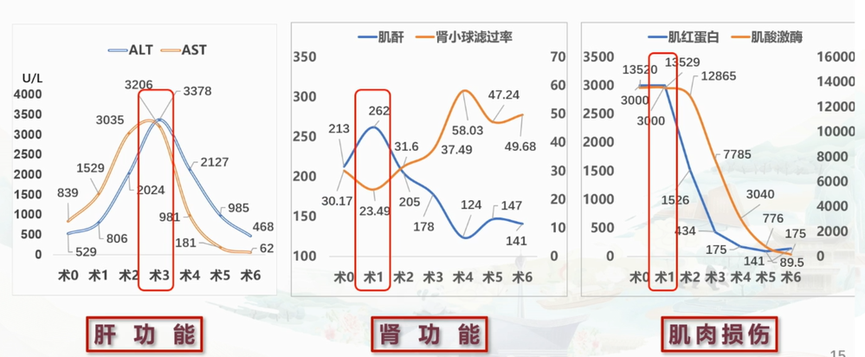
Biochemistry:
• Creatine kinase: 13,520 U/L
• Myoglobin: >3000 ng/ml
• ALT: 529 U/L
• AST: 839 U/L
• Creatinine: 213 umol/L
• Estimated glomerular filtration rate: 30.17 ml/min/1.73m².
Diagnosis:
1. Acute Type A aortic dissection with malperfusion.
2. Grade 3 hypertension, very high risk.
3. Acute liver function impairment.
4. Acute kidney function impairment.
5. Metabolic acidosis.
Treatment:
1. Control of Blood Pressure, Heart Rate, and Pain: Urapidil combined with esmolol to maintain left upper limb systolic blood pressure below 120 mmHg, heart rate at 60-80 bpm. Morphine hydrochloride for rapid pain relief.
2. Correction of Acid-Base Imbalance and Liver Protection: Sodium bicarbonate to correct acidosis; Ganning and polyene phosphatidylcholine for liver protection.
3. Improving Blood Flow: Alprostadil and papaverine to improve distal blood flow.
4. Emergency Interventional Surgery: Stage 1 intervention to rapidly restore abdominal organ and lower limb perfusion.
Stage 1 Interventional Surgery
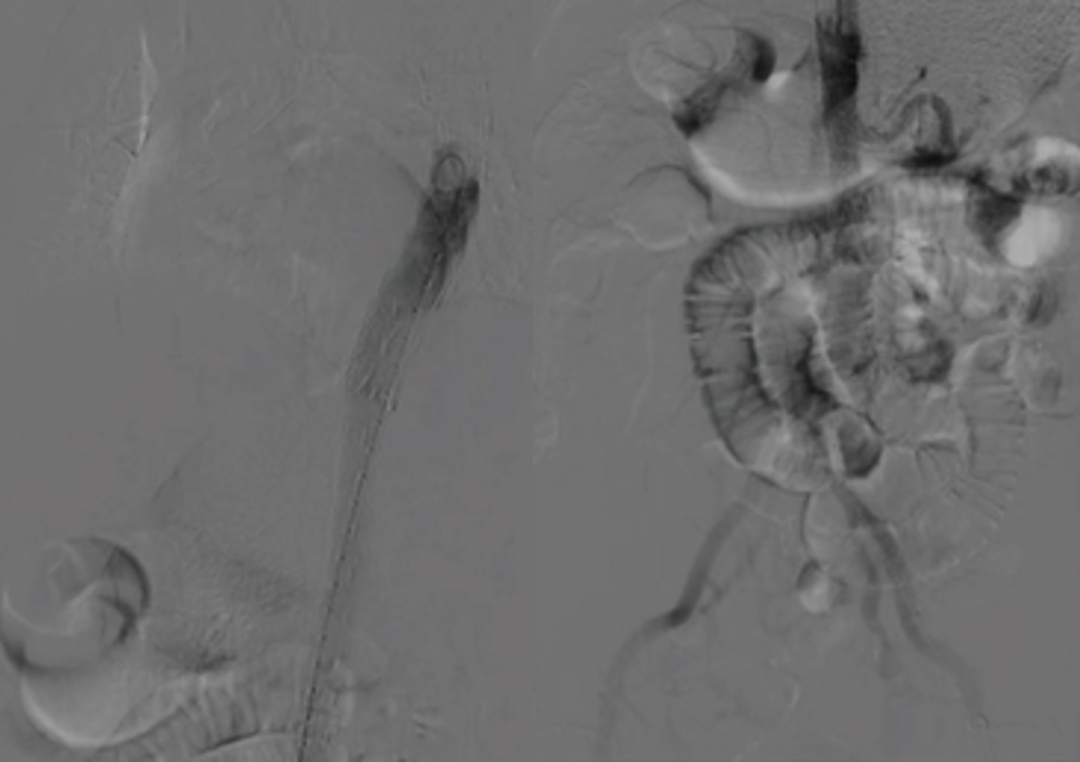
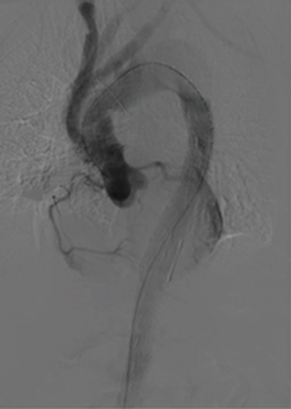
Procedure 1: Aortography showed a narrow true lumen in the thoracoabdominal aorta and delayed celiac trunk visualization.
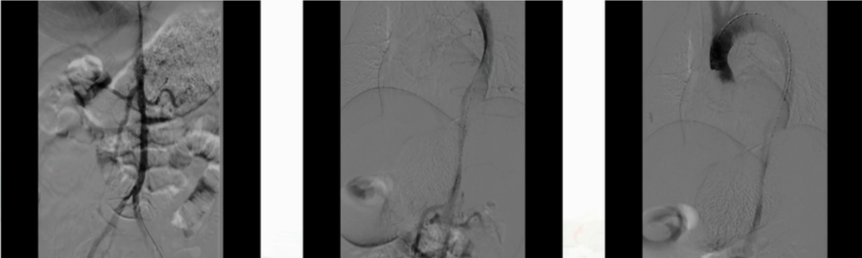
Procedure 2: A S&G TAA2824B120 covered stent was placed in the descending aorta, and a Valiant DM-TB-2620180 bare stent was used to extend across the visceral branches.
Procedure 3: Super-selection of the celiac trunk was performed, with Cordis C08040 bare stent placement and balloon dilation.

Procedure 4: Aortography confirmed expansion of the true lumen in the thoracoabdominal aorta and good celiac trunk perfusion.
Postoperative Treatment
Continued blood pressure and heart rate control with sedation and analgesia: Urapidil combined with nicardipine and esmolol to maintain systolic pressure of the left upper limb below 120 mmHg and heart rate at 60-80 bpm; propofol combined with hydromorphone for sedation and analgesia.
Continued liver protection and improved blood supply: Ganning and polyene phosphatidylcholine for liver protection; alprostadil and papaverine to improve distal blood flow.
Bedside CRRT treatment for myoglobinuria and acute kidney injury.
Complication: Five hours postoperatively, the patient passed 250 g of bloody stool, and nasogastric drainage showed light bloody fluid. Enhanced CT of the dissecting aneurysm showed that the true lumen of the thoracoabdominal aorta was expanded, and the proximal celiac trunk was well perfused. Intestinal wall edema and scattered gas-fluid levels were noted, with peritoneal thickening and swelling.
Treatment: Proton pump inhibitors were added for gastric protection.
ICU Monitoring

Postoperative Day 6: Enhanced CT showed no significant changes in the thoracoabdominal aorta or its branches. The intestinal wall was still edematous, and scattered gas-fluid levels were observed, but no signs of necrosis or perforation were found.
Stage 2 Hybrid Surgery
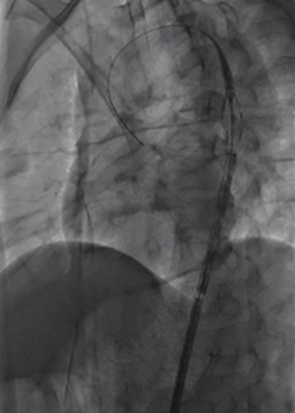
Procedure 1: Median sternotomy with ascending aorta replacement and arch branch resection.
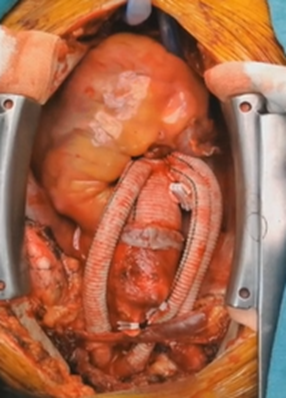
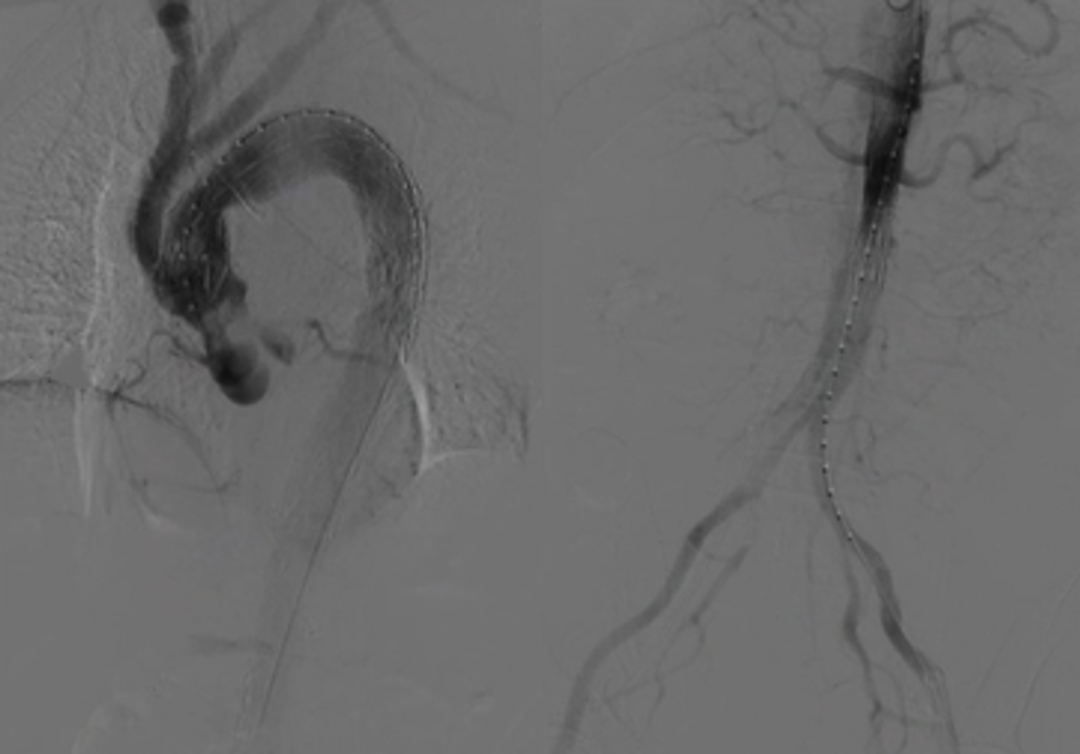
Procedure 2: Aortic arch angiography followed by deployment of a S&G TAA3030B200 covered stent.
Procedure 3: Repeat angiography confirmed effective expansion of the true lumen in the thoracoabdominal aorta, with good visceral and iliac artery perfusion.
Outcome: Total hospital stay was 16 days, including 14 days in ICU. Upon discharge, the patient was able to tolerate liquid food, with grade 3 lower limb muscle strength. The patient was transferred to a secondary hospital for further rehabilitation.
Follow-Up: One month postoperatively, follow-up CT angiography showed patent grafts and stents without dislocation or endoleak. The abdominal branches and iliac artery were well-perfused, and the intestinal wall showed no abnormalities.


