During the 9th China Vascular Conference (CVC 2024), held on September 12, 2024, at the Chengdu Century City International Convention Center, the annual Top 10 Case Showcase of the Vascular Surgery Group of the Chinese Clinical Case Database was successfully held. Numerous surgical experts provided in-depth analysis and experience sharing on the selected top 10 cases. Professor Kang Fei from the Vascular Surgery Department of the First Affiliated Hospital of Fujian Medical University shared his experience in using a physician-modified endograft for treating a case of juxtarenal abdominal aortic aneurysm.

Case Sharing
Patient Information (Male, Middle-aged)
Chief Complaint: Abdominal pulsatile mass found for six months.
Past Medical History: History of hypertension for more than 10 years, with a maximum blood pressure of 160/100 mm Hg, regularly controlled with antihypertensive medication, currently at 120/80 mm Hg. Four years ago, the patient underwent coronary artery stent implantation due to myocardial infarction and has been on long-term use of clopidogrel and rosuvastatin.
Physical Examination: Soft and non-tender abdomen without rebound tenderness. A pulsatile mass approximately the size of a fist was palpated around the umbilical region, with a pulsation rate consistent with the heartbeat. Bowel sounds were 3 times per minute, and peripheral pulses in all four limbs were good.
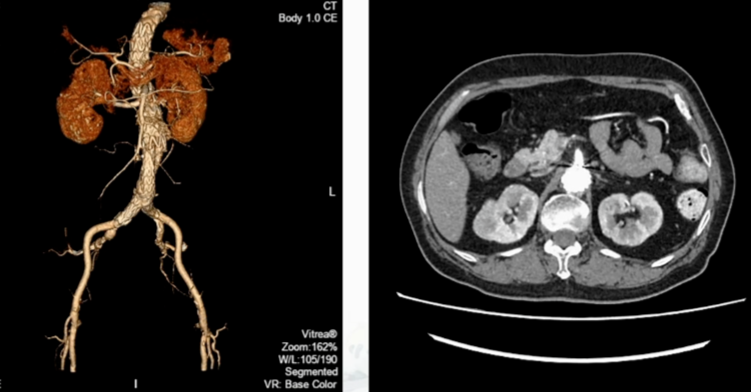
Additional Tests: Echocardiogram showed left ventricular hypertrophy and thickening of the interventricular septum, grade II left ventricular diastolic dysfunction, and normal LVEF. CTA revealed a thoracic aortic aneurysm and an abdominal aortic aneurysm.
Preoperative Diagnosis: Abdominal aortic aneurysm, thoracic aortic aneurysm, hypertension, coronary artery disease post-coronary stenting.
Preoperative Assessment:
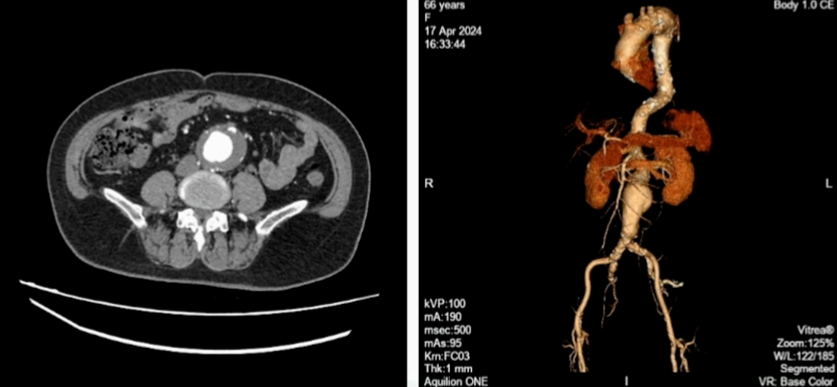
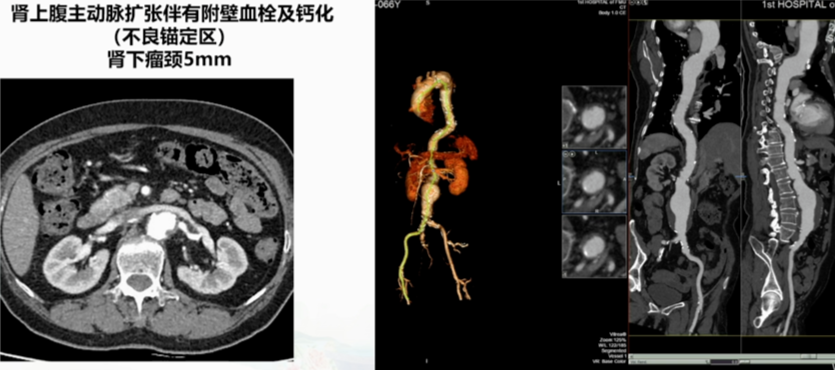
• Juxtarenal Abdominal Aneurysm: Maximum diameter of 6.3 cm. The thoracic aortic aneurysm had a maximum diameter of 4.8 cm, with tortuous necks and mural thrombus. Bilateral accessory renal arteries were noted.
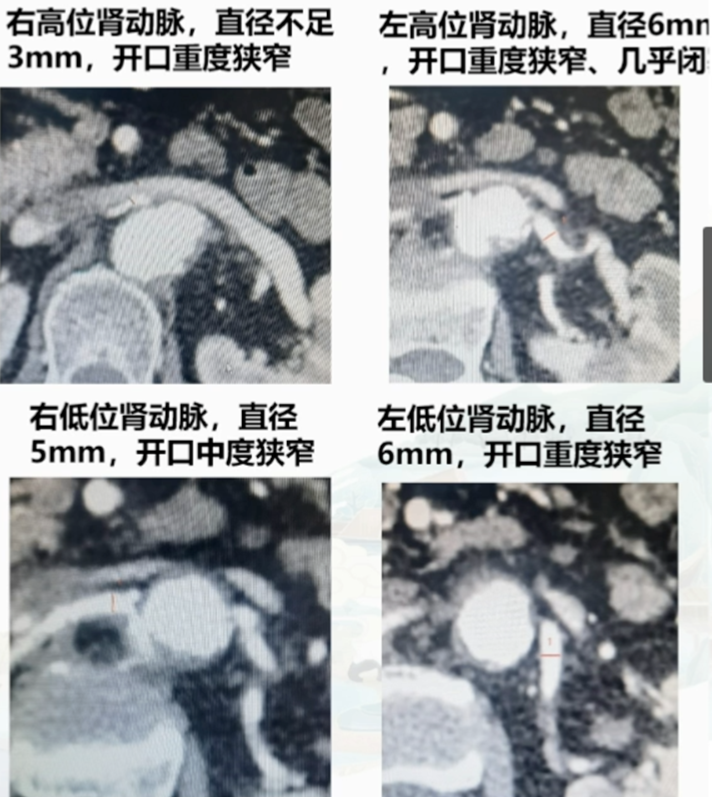
Bilateral Renal Artery Stenosis:
• Right High-position Renal Artery: Diameter less than 3 mm, with severe ostial stenosis.
• Right Low-position Renal Artery: Diameter 5 mm, with moderate ostial stenosis.
• Left High-position Renal Artery: Diameter 6 mm, with severe ostial stenosis, almost occluded.
• Left Low-position Renal Artery: Diameter 6 mm, with severe ostial stenosis.
•Dilated Suprarenal Abdominal Aorta: Presence of mural thrombus and calcification (poor anchoring zone), with a 5 mm infrarenal neck.
Preoperative Planning:
• The accessory right renal artery was too small, so it was planned to be sacrificed without preoperative fenestration. Both left renal arteries required fenestration and reconstruction due to their narrow lumens and near occlusion. The plan involved 3D printing assistance for five fenestrations and reconstruction of the visceral branches.
Preoperative Preparation:
1. Preoperative full aortic CTA to evaluate the surgical approach and arch condition.
2. Measurement of the abdominal aorta, visceral artery diameters, main trunk lengths, and clock-face positions of the branch ostia. Fenestration positions were roughly sketched.
3. 3D printing of the model and low-temperature plasma sterilization.
4. Surgical instruments included the main body stent, iliac branch stents, branch stents, balloons, sterile markers, sterile rulers, spring coils, etc.
Surgical Procedure
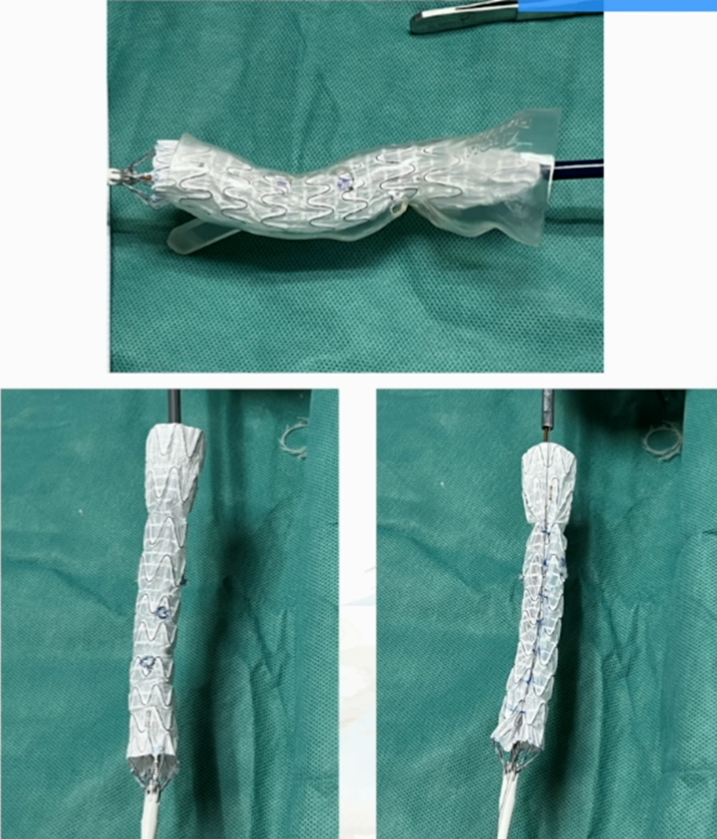
Procedure 1: Preoperative Fenestration Process
1. Fenestration of the visceral area using the 3D-printed model, and fixation of spring coils at the fenestration site.
2. Stitching internal or external branches according to lesion type.
3. Diameter reduction: Flatten the proximal part of the delivery system.
4. Use a syringe needle to puncture the front end of the delivery system, guide the V-18 wire through.
5. Fixation at the front end of the covered stent using 3-0 prolene sutures.
6. Reassembly: Optional use of infusion set to aid stent restraint.
7. Patient Position: Supine.
8.Access Selection: Left axillary artery incision, bilateral common femoral artery puncture, and pre-placement of two suture devices.
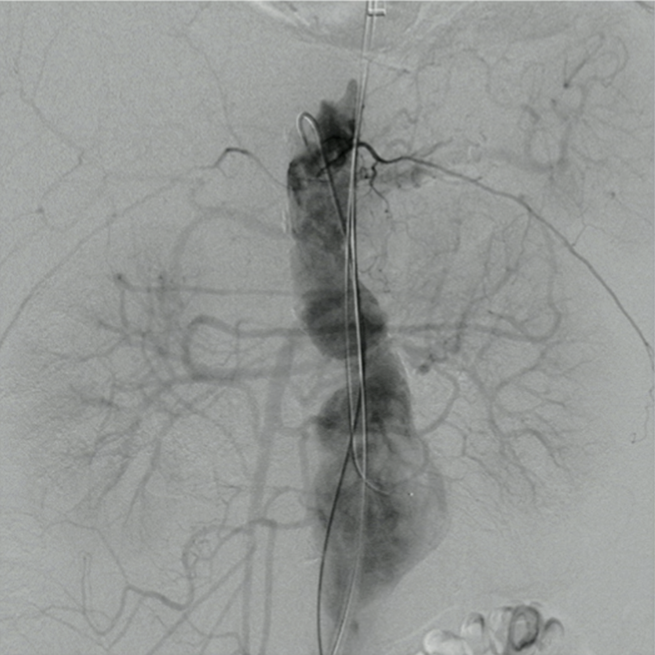
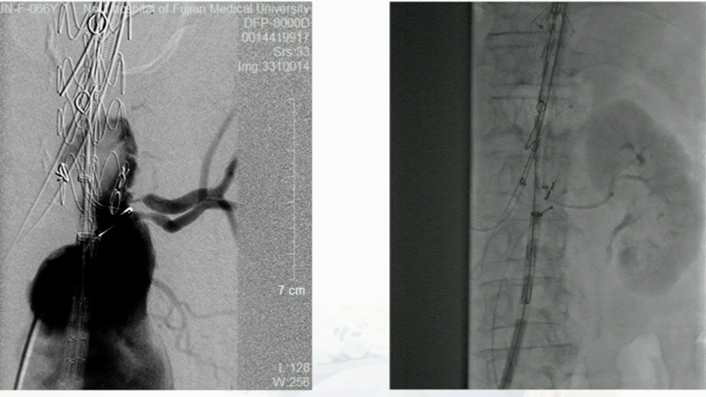
Procedure 2: Intraoperative Aortography
Confirmed the consistency of the lesion with the preoperative assessment.
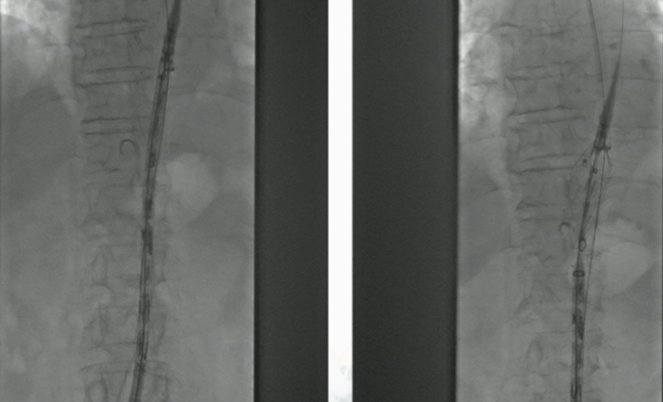
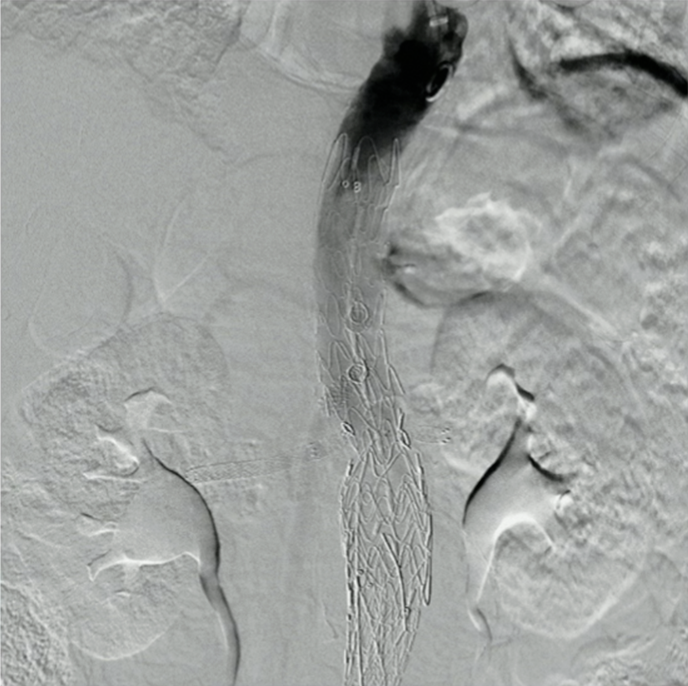
Procedure 3: Placement and deployment of the pre-fenestrated main body stent via the right femoral artery.
Procedure 4: After releasing the celiac artery (CA) fenestration, the guidewire was pre-positioned in the CA, and the stent was further released to the superior mesenteric artery (SMA) fenestration, similarly pre-positioning the guidewire.

Procedure 5: Continued deployment of the proximal covered portion, super-selecting the right renal artery.

Procedure 6: Difficulty was encountered in super-selecting the left renal artery due to the severe ostial stenosis and near occlusion. Eventually, the fenestration for the low-position left renal artery was abandoned, and super-selection was achieved for the high-position left renal artery.
Procedure 7: Long sheath placement in the left renal artery for fixation.
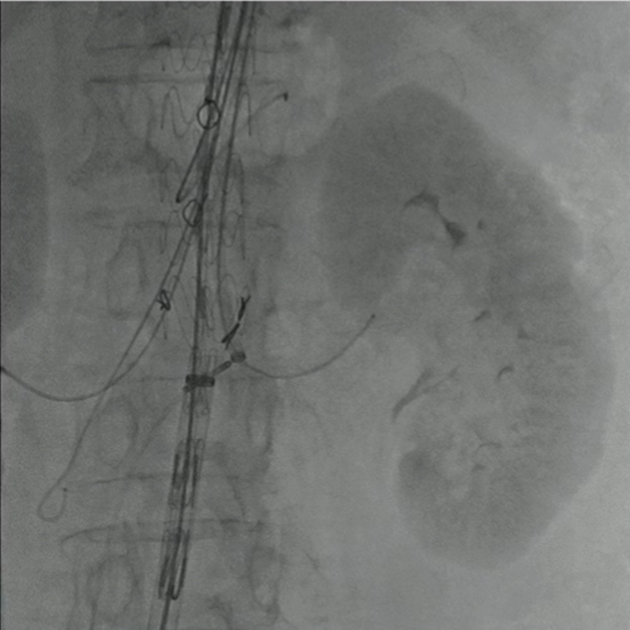
Procedure 8: PTA combined with stent placement in the right renal artery. A dissection occurred in the process, affecting distal flow, and a rescue stent (5×60 mm) was implanted.

Procedure 9: SMA was expanded and a balloon-expandable stent was implanted.
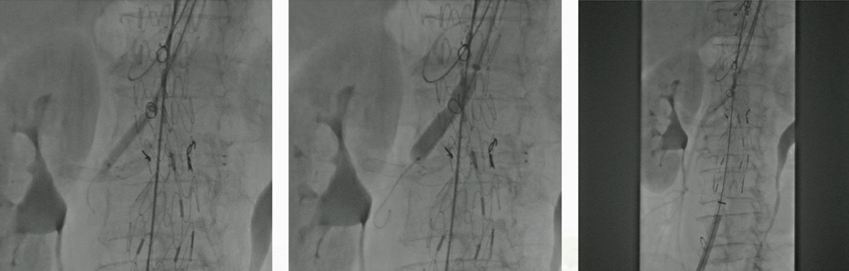
Procedure 10: CA was expanded and a self-expanding stent was implanted.
Procedure 11: EVAR with bare stent deployment below the renal arteries.
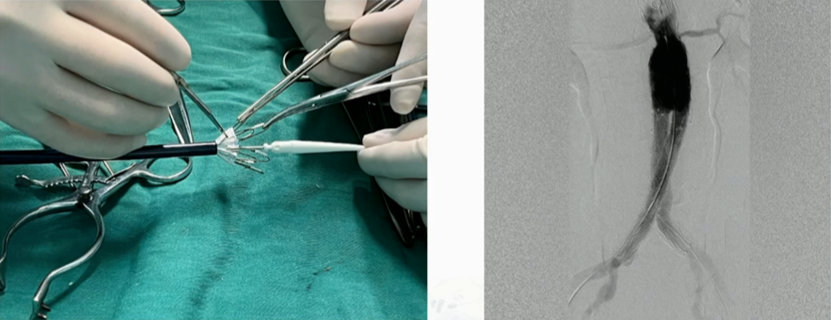
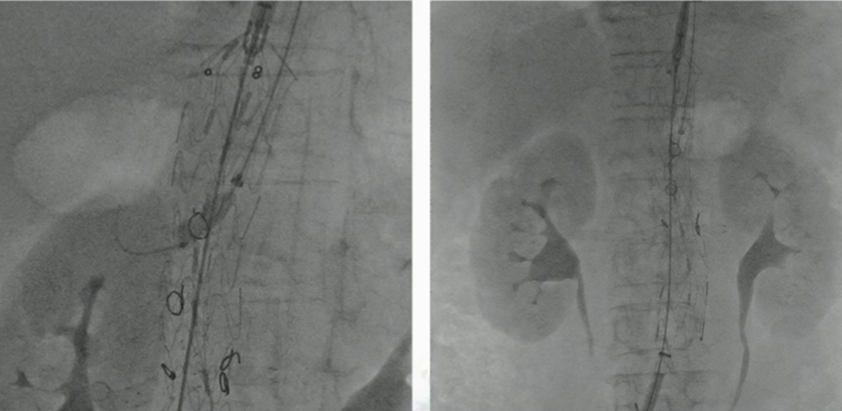
Outcome: Postoperative angiography showed satisfactory reconstruction of the four visceral branches without endoleak.
Postoperative Management
1. Spinal Cord Ischemia Prevention: Maintain optimal blood pressure, generally at 130-140 mm Hg.
2. Contrast-Induced Nephropathy Prevention: Hydration.
3. Medication: Antiplatelet, anticoagulation, statins, antihypertensive drugs, etc.
Postoperative Follow-Up
Postoperative CTA showed a patent abdominal aortic stent with satisfactory reconstruction of the visceral branches.