Endovascular aneurysm repair (EVAR) has become the primary treatment for abdominal aortic aneurysms (AAA) due to its minimally invasive nature, reduced bleeding, and quick postoperative recovery. Despite the decreasing perioperative risk, follow-up issues still require close monitoring and occasional re-intervention. On May 18, 2024, at the 2nd Tianfu Vascular Conference (TFS 2024), Professor Zhao Jichun from West China Hospital, Sichuan University, shared insights from the “EVAR Cohort Study Data and Management of Complications in Endovascular Treatment of Complex Abdominal Aortic Aneurysms.”

EVAR Cohort Study at West China Hospital
West China Hospital’s vascular surgery department was a major contributor to the Engage Asia-Pacific cohort, leading early (2011-2016) enrollment and later (2017-2021) including more complex AAA anatomies. The EVAR cohort study, based on the Engage study model, included patients from 2011 to 2021.
Inclusion Criteria:
1. Infrarenal abdominal aortic aneurysms
2. AAAs with or without common iliac artery aneurysms
3. Meeting surgical intervention indications
Exclusion Criteria:
1. Pseudoaneurysms or penetrating ulcers
2. Intramural hematoma or aortic dissection
3. Infectious aneurysms
4. Thoracoabdominal aneurysms or AAAs involving renal or other visceral arteries
5. Patients using CERAB or Kissing techniques
6. Post-aneurysm surgery re-intervention
7. Lack of preoperative abdominal aortic CT or unavailable anatomical parameters
Intervention:
All patients underwent standardized surgical procedures by experienced vascular surgeons, minimizing intervention-related confounding factors.
Outcomes:
• Short-term Outcomes: Primary: 30-day mortality. Secondary: 30-day re-intervention, aneurysm rupture, cardiovascular events, acute kidney injury.
• Long-term Outcomes: Primary: 3-year re-intervention rate. Secondary: 3-year adverse aortic events, overall survival, aortic-related mortality.
Patient Baseline Data:
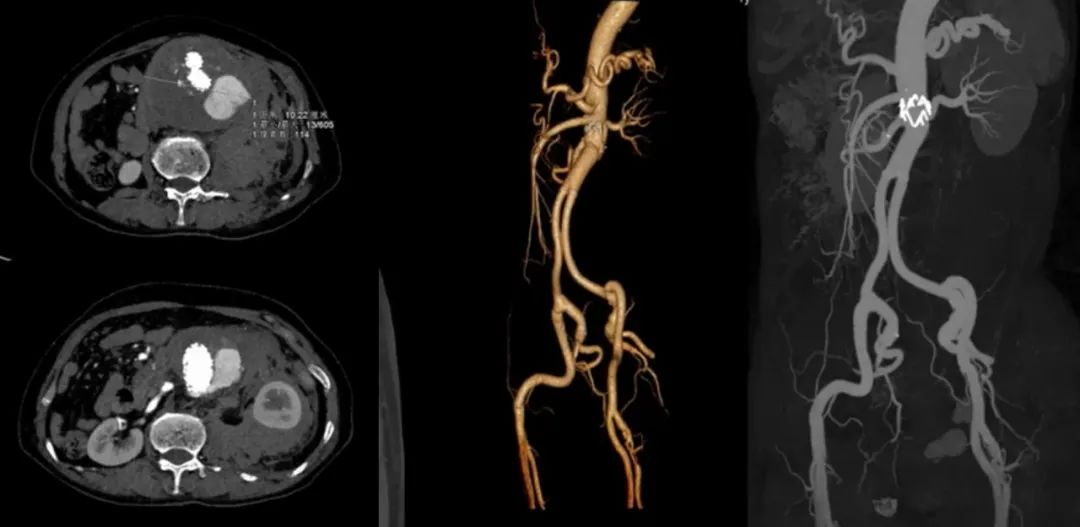
The study included 1095 patients, with an average age of 71.14±9.60 years, 83.01% male. Co-morbidities included hypertension (66.63%), diabetes (12.8%), lung disease (18.15%), coronary artery disease (17.42%), and chronic kidney disease (5.35%). Average aneurysm neck length was 27 mm, diameter 20 mm, with severe angulation in 26.66%, and mean aneurysm diameter 51.8 mm. The left common iliac artery averaged 15 mm in diameter, and the right 16 mm. The cohort exhibited more complex anatomies than the Engage cohort, mainly with twisted aneurysm necks.
Short-term Outcomes:
The 30-day mortality rate was 1.36% (15/1095), mainly due to post-rupture abdominal compartment syndrome (27%), cardiac events (27%), and lung infections (20%).
Long-term Survival Outcomes:
The average follow-up was 49.1±32.0 months, with a median survival follow-up of 45.8 months. The 1-year aortic event-free survival rate was 99.1%, 3-year was 98.3%, and 5-year was 95.8%. Major causes of death included tumors (15.3%), myocardial infarction (9.0%), stroke (9.0%), and lung infections (8.6%). Aortic-related deaths were due to unknown aneurysm rupture (n=17), stent fracture (n=1), stent infection (n=2), type Ib endoleak (n=4), and proximal aortic dissection (n=1).
Long-term Complications:
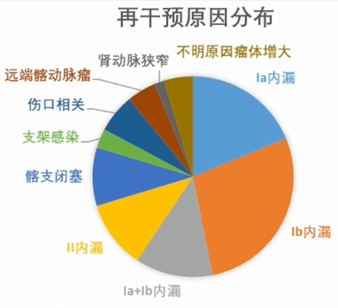
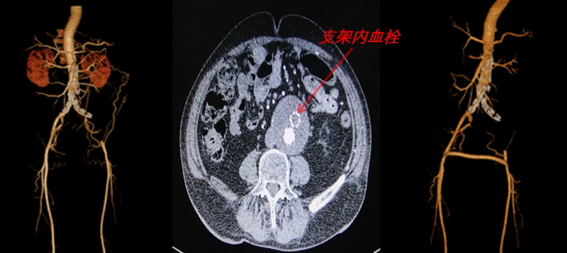
Re-interventions were most commonly for type Ib endoleak (28.4%), followed by type Ia endoleak (16.4%). Over 60% of type I endoleak-related re-interventions were successful. Stent infection, though rare, posed complex challenges. Distal iliac artery aneurysms, internal iliac artery aneurysms, renal artery stenosis, and wound-related factors also required attention.
Managing EVAR Complications
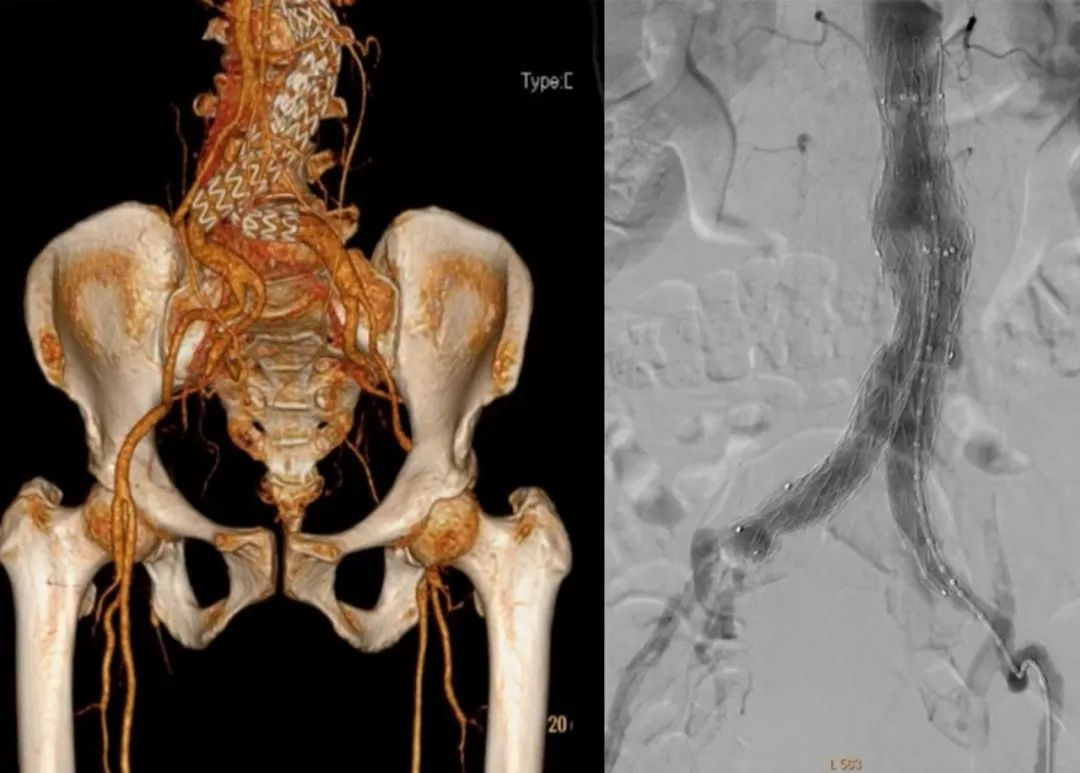
Complex AAAs, including those with severe angulation, short necks, large aneurysms, mural thrombus, iliac artery aneurysms, ruptures, and tortuous, narrow, or occluded access arteries, pose significant challenges and increase postoperative complication rates. Common EVAR complications include endoleak, iliac limb occlusion, stent migration, stent kinking, stent infection, and aneurysm rupture.
Endoleak Management:
The 2018 SVS guidelines recommend treating type I endoleaks, closely monitoring type II endoleaks, and treating type III endoleaks. For type I and II endoleaks causing aneurysm expansion unresponsive to endovascular treatment, surgical intervention is advised (1B). The 2019 ESVS AAA guidelines recommend prompt intervention for type I endoleaks post-EVAR (1B).
For stable or reducing type Ia endoleaks without aneurysm expansion, continued clinical observation is advised. If proximal type Ia endoleaks cause aneurysm expansion, balloon angioplasty and additional cuff stents or coil embolization can be effective. For type Ib endoleaks, extending the iliac limb with additional stents is recommended. For type II endoleaks with aneurysm expansion, coil embolization is advised.
Case Studies:
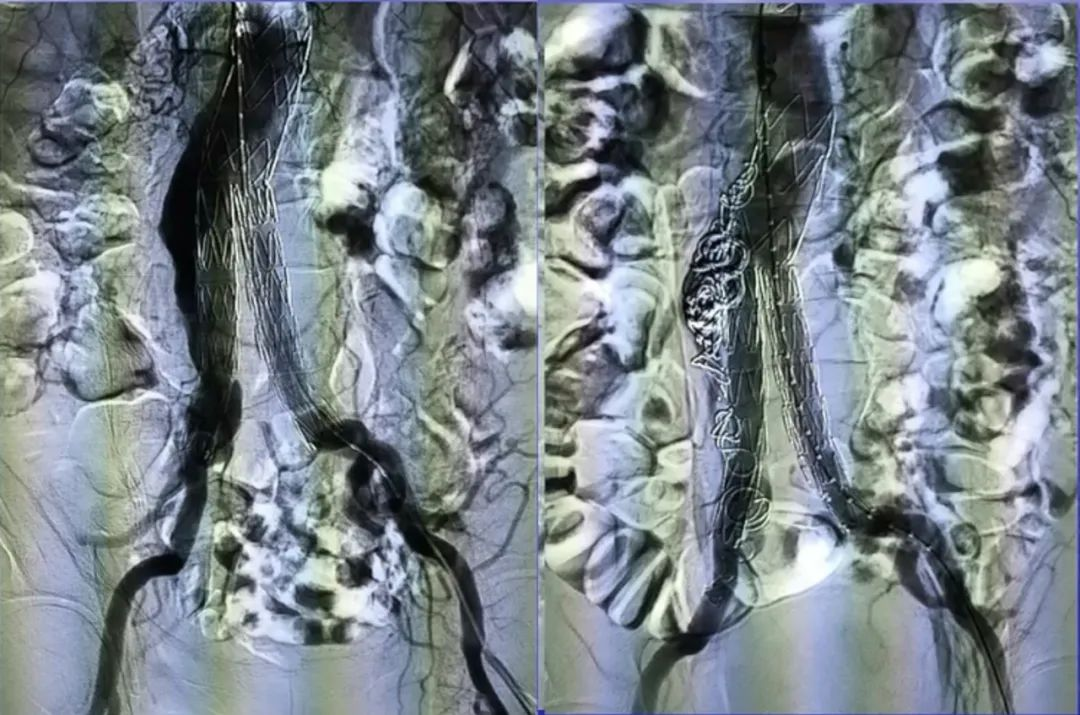
Case 1: 78-year-old male with type Ia endoleak and right internal iliac artery communication 3+ years post-EVAR. Coil embolization of the aneurysm sac and right internal iliac artery showed significant improvement on follow-up angiography.
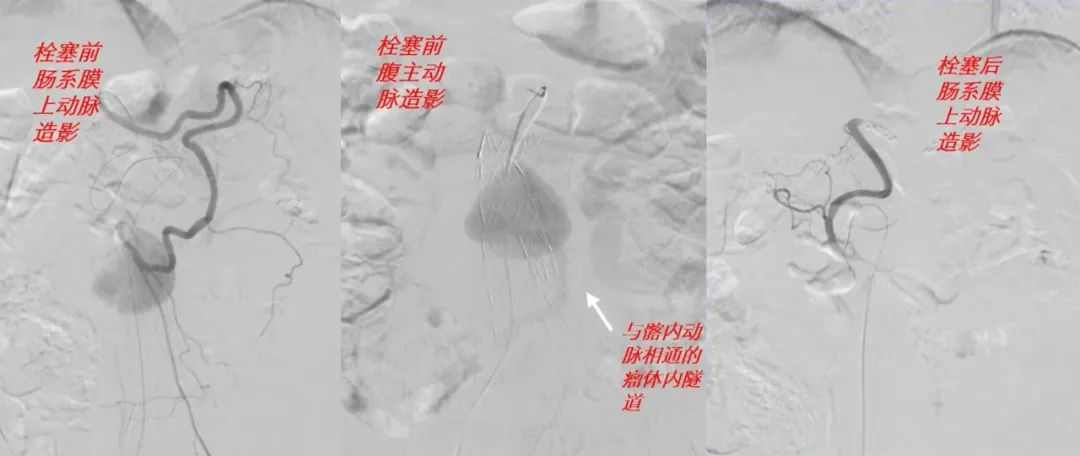
Case 2: 77-year-old male with type II endoleak involving the inferior mesenteric artery and communication with previously embolized right internal iliac artery 66 months post-EVAR. Coil embolization of the Riolan’s arch artery through the superior mesenteric artery resolved the endoleak.
Case 3: 62-year-old female with type Ia endoleak and rupture post-EVAR. Open surgery with aneurysm resection, stent removal, and graft replacement was performed.
Case 4: 70-year-old male with left iliac limb occlusion 1 year post-EVAR. Bilateral femoral-femoral bypass was performed.
Case 5: 70-year-old female with left femoral artery embolism 13 months post-EVAR. Femoral artery thrombectomy and thrombolysis were successfully performed.
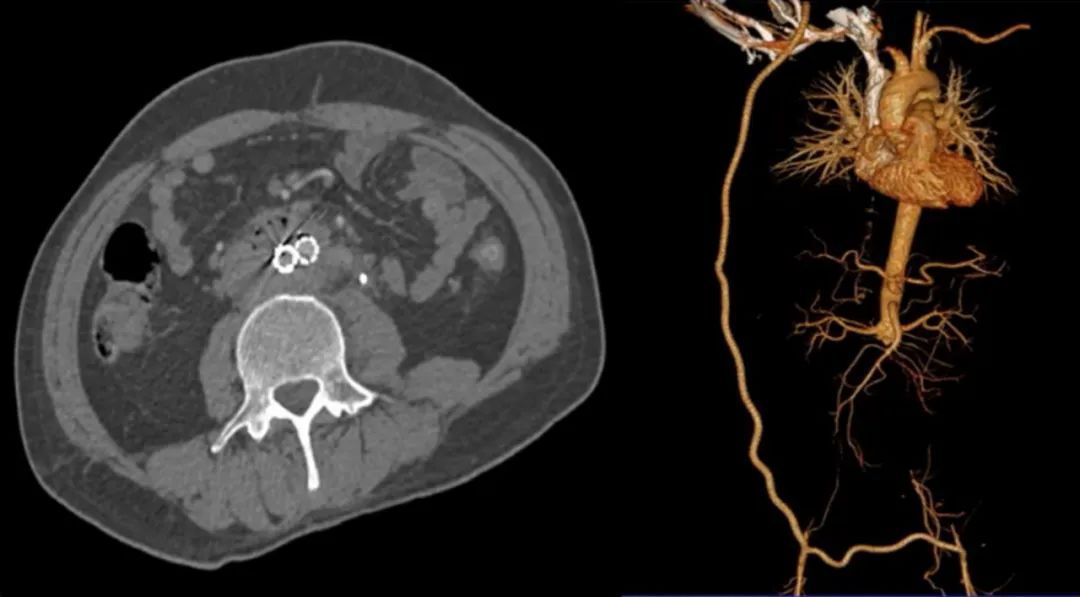
Case 6: 51-year-old male with stent infection, abdominal pain, fever, and gastrointestinal bleeding 1 year post-EVAR. Removal of the infected stent, infrarenal aortic ligation, and right subclavian to bilateral femoral artery bypass was performed. The patient was discharged after 13 days with oral antibiotic therapy.
Conclusion
Thorough preoperative evaluation of EVAR indications, aneurysm neck, aneurysm morphology, iliac artery anchoring zone anatomy, and access arteries is crucial for successful complex AAA endovascular repair. Close postoperative monitoring of aneurysm diameter and endoleak changes is necessary for timely complication management. Open surgery is warranted for rupture risk and graft infection to ensure long-term EVAR efficacy.
Contact Us
For more in-depth analysis on the treatment of complex abdominal aortic aneurysms and insights from the Tianfu Vascular Conference, stay tuned for our upcoming articles. If you have any questions or interests, please leave a comment or contact us via email at endovascluar@simtomax.cn. Thank you for your attention. Let’s work together for health!