
With the aging population, the incidence of aortic diseases is rising annually. High-risk elderly patients with aortic diseases are likely to increase in the future. Data from the National Hospital Quality Monitoring System (HQMS) indicates a yearly increase in aortic surgeries, including both open surgeries and minimally invasive endovascular procedures. On May 18, 2024, at the 2nd Tianfu Vascular Conference (TFS 2024), Professor Shu Chang from Fuwai Hospital, Chinese Academy of Medical Sciences, shared advancements in minimally invasive treatment for aortic diseases.

Treatment Strategies for Ascending Aortic Diseases
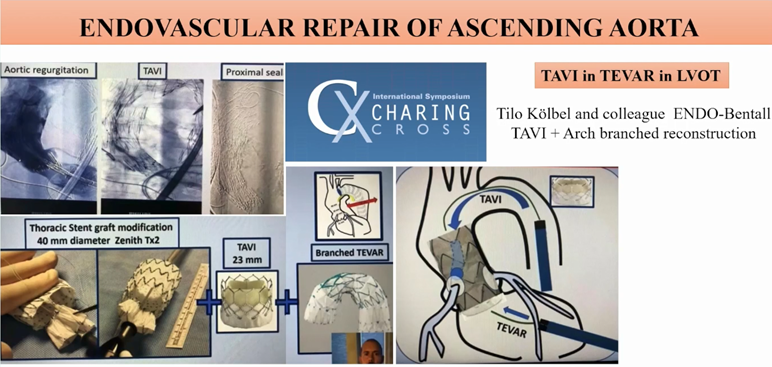
In the early days, endovascular surgery for ascending aortic diseases was considered off-limits, with open surgeries such as ascending aorta replacement, Bentall surgery, and David surgery being the main options. However, with the progress of minimally invasive techniques and the development of devices, endovascular repair has expanded to treat ascending aortic diseases.
As early as 2001, Academician Wang Zhonggao successfully performed the first ascending aorta stent implantation, treating acute total aortic dissection. In 2015, Professor Shu Chang completed the first domestic ascending aorta and descending aorta stent implantation in Indonesia. In 2017, Professors Rylski and White proposed the Endo-Bentall/Endo-Wheat technique for complete endovascular repair of the aortic root and ascending aorta in one stage. In 2020, Professor Gaia performed the world’s first Endo-Bentall surgery for a patient post-aortic valve replacement. In 2023, Professor Kölbel demonstrated the Endo-Bentall TAVI and aortic arch branch reconstruction at the CX conference.
Treatment Strategies for Aortic Arch Diseases
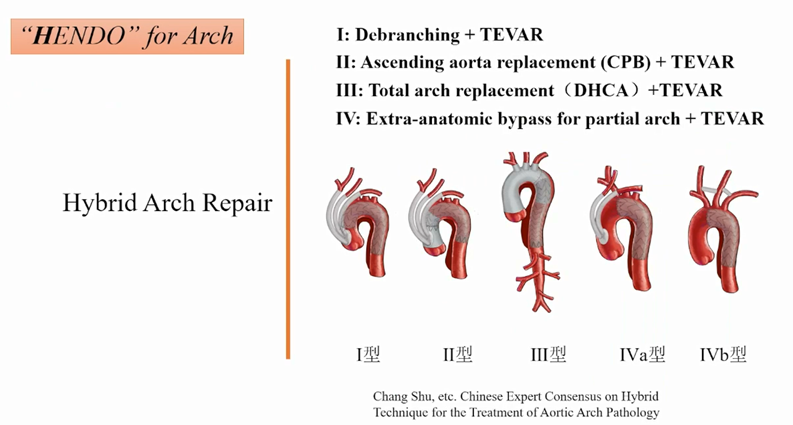
Treating aortic arch diseases requires individualized strategies considering etiology, pathology, and anatomical structure. Based on this, Professor Shu proposed the “HENDO” treatment system, including Hybrid Arch Repair, Endovascular Repair, and Open Arch Repair.
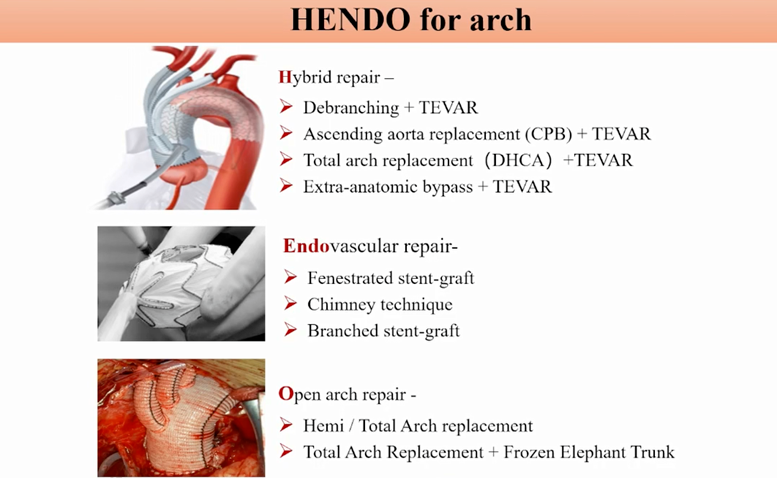
Open surgical techniques include partial arch replacement, total arch replacement, and total arch replacement with frozen elephant trunk stenting, often requiring deep hypothermic circulatory arrest (DHCA), which carries high surgical risks.
Hybrid surgical techniques combine open surgery with minimally invasive endovascular repair, divided into four types:
1. Hybrid I: Ascending aorta-head branch artery bypass with total arch covered stent endovascular repair.
2. Hybrid II: Ascending aorta replacement (with or without aortic root repair, CPB) with head branch artery debranching, combined with total arch covered stent endovascular repair.
3. Hybrid III: Ascending aorta (with or without aortic root repair) and aortic arch replacement, with or without hard or soft elephant trunk stenting, combined with catheter technology to assess or repair distal aorta and further disease.
4. Hybrid IV: Non-extracorporeal circulation, open chest ascending aorta-one or two arch branch artery bypass (IVa), or neck bypass (IVb), combined with partial aortic arch covered stent endovascular repair.
Rapid Development of Endovascular Techniques and Devices
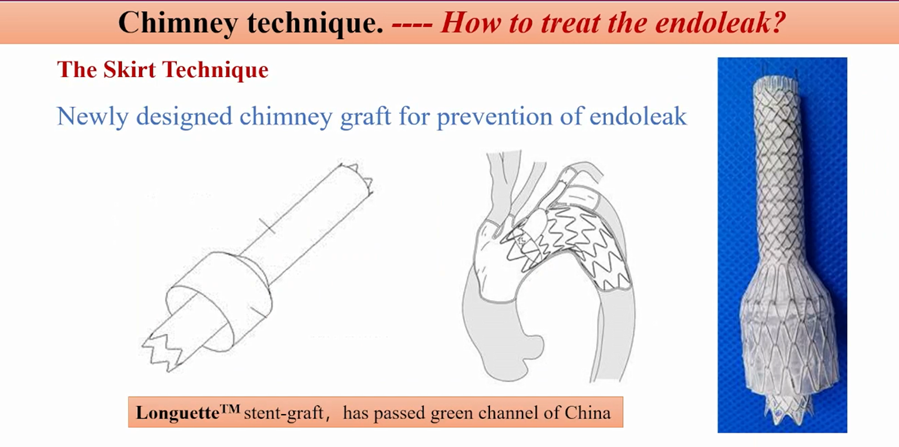
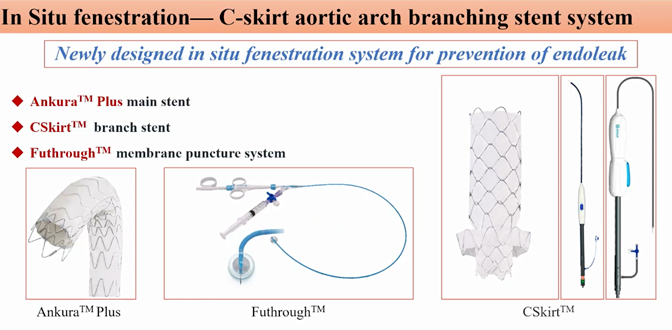
Endovascular techniques include parallel stenting (chimney technique), fenestration techniques, and branched stent grafts. New devices include Longuette™ stents, CSkirt aortic arch branch stent system, and Ankura™ stents.
• Parallel Stenting (Chimney Technique, ch-TEVAR): Techniques include single, double, or triple chimney stenting. Flexible large stents should be used to avoid small stents squeezing out gaps. Proper overlapping of parallel stents reduces endoleak. This technique is suitable for complex anatomies and can be used as a remedial measure if the arch branches are accidentally covered. ch-TEVAR may have limitations leading to Gutter endoleaks, with an incidence of Type Ia endoleak around 1.2%-20%. The Longuette™ stent, developed under Professor Shu’s guidance, effectively prevents endoleaks. Multicenter clinical trials indicate an immediate technical success rate of 100% and a 97.88% rate of avoiding secondary intervention, with Type I/III endoleak occurrence of only 1.4% during follow-up.
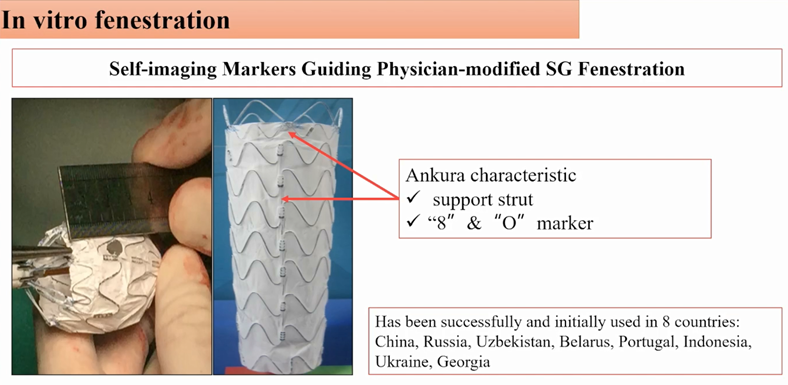
• Fenestration Techniques: Include ex situ pre-fenestration and in situ fenestration, chosen based on branch vessel angles, sometimes combining both techniques. This maintains the original anatomical structure of arch branch vessels, adapts to aortic arch morphology, has low endoleak incidence, and shortens surgery time. Professor Shu’s team innovatively proposed using the stent’s radiopaque markers for fenestration and branch artery positioning—the stent self-imaging positioning method with the Ankura aortic stent. This technique is quick, requiring only 5 minutes for fenestration and a single femoral artery puncture to reconstruct the three arch branches. Intraoperative single branch reconstruction takes 30 minutes, double branch 1 hour, and triple branch 1.5 hours. Ankura products have been successfully used in over 10 countries.
• Branched Stents: Match vascular anatomy, avoiding gutter endoleaks or stent migration, effectively addressing aortic arch diseases. The Castor® branched stent, the first domestic integrated aortic arch branched stent, completes LSA reconstruction in one stage during TEVAR. Combined with parallel stenting, Castor® can also reconstruct the LCCA and LSA. Additionally, the WeFlow series aortic arch branched stent developed by Professor Wei’s team enables complete endovascular reconstruction of single, double, and triple arch branches, showing promising initial clinical results.
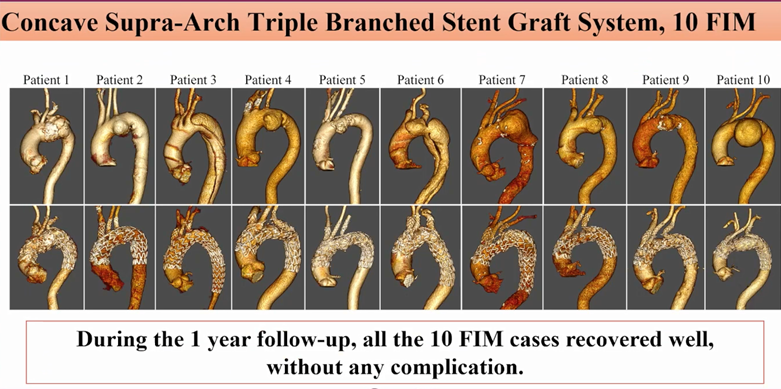
Professor Shu’s new aortic stent FIM study has completed 10 surgeries, with short operation times, minimal intraoperative bleeding, satisfactory immediate effects, and follow-up results (1-2 years), with no severe complications.
Treatment Strategies for Descending Aortic Diseases
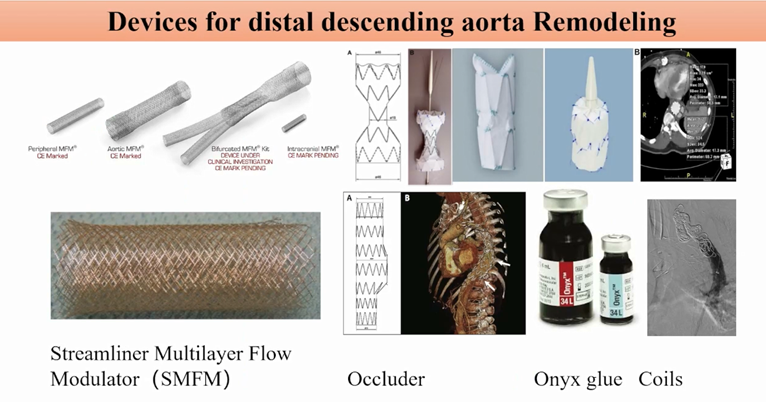
Treatment of descending aortic diseases focuses on distal aorta remodeling. TEVAR faces challenges such as residual distal entry tears causing aneurysmal expansion, unresolved distal true lumen narrowing, and new distal dissection entry tears (SINE). Clinicians have tried using multilayer bare stents, plugs, adhesives, and coils to address these challenges.
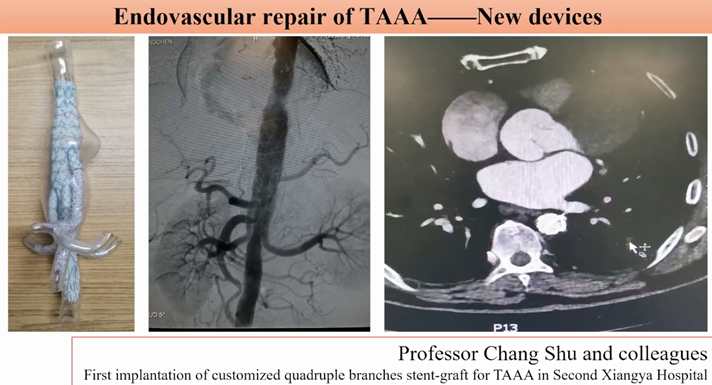
For complete endovascular repair of thoracoabdominal aortic aneurysms, new products are under development and clinical trials. Professor Wei’s team has completed FIM research for the G-Branch™ thoracoabdominal aortic covered stent system, demonstrating its clinical feasibility. Multicenter clinical trials show promising results. Professor Shu’s team designed a customized four-branch thoracoabdominal stent, successfully applied in Xiangya Second Hospital’s first clinical case, with 2-year follow-up showing good efficacy.
Treatment Strategies for Abdominal Aortic Diseases
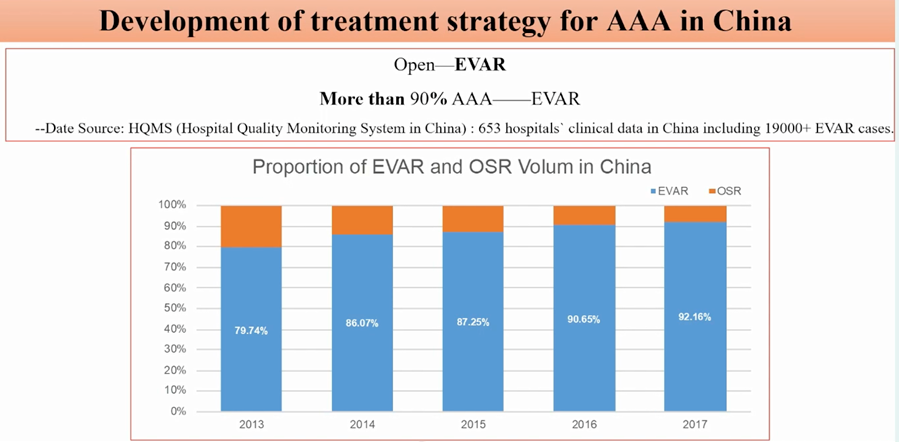
HQMS data indicates that by 2016, over 90% of AAA patients in China received endovascular treatment, including those with complex anatomical AAA (cAAA). Techniques like extreme renal release, ex situ fenestration, CUFF stent use, chimney technique, and new stent development are efforts to tackle cAAA. However, endovascular surgery cannot address all cAAA cases, and open surgery remains a fundamental treatment.
Conclusion
Treatment of aortic diseases is transitioning from open surgery to hybrid and endovascular repair. Minimally invasive approaches are the future trend. Open surgery remains the foundation for treating aortic diseases, with meticulous and precise direct vision surgery being the gold standard for complex lesions. The diverse anatomy and pathology of aortic diseases require tailored treatment plans. Cautious branch reconstruction is advised, performed only when necessary. Many new non-customized single, double, and triple branched stent systems are under development, and further safety and efficacy data are anticipated.


