Venous thromboembolism (VTE) is the third most common cardiovascular and cerebrovascular disease after acute myocardial infarction and stroke, and the average annual prevalence of VTE is on the rise due to factors such as population aging.VTE includes deep venous thrombosis (DVT) and pulmonary embolism (PE), which are different stages of the same disease. VTE includes deep venous thrombosis (DVT) and pulmonary embolism (PE), which are different stages of the same disease. the main adverse events of DVT include limb swelling and pain, necrosis, PE, and post-thrombotic syndrome (PTS), which seriously affects the survival and quality of life of patients. In recent years, with the increasing awareness of DVT and PTS, the treatment concept of DVT has changed. Among them, endoluminal treatment, with the advantages ofminimallyinvasive, early symptomatic improvement, protection of valve function, and prevention of PTS, has gradually replaced the traditional open surgery, and has become the preferred method of surgical treatment for DVT.
This article develops the Expert Consensus on Endoluminal Treatment of Acute Lower Extremity Deep Vein Thrombosis based on recent clinical trial results, clinical guidelines, and clinical experience to provide guidance on endoluminal treatment of lower extremity deep vein thrombosis.

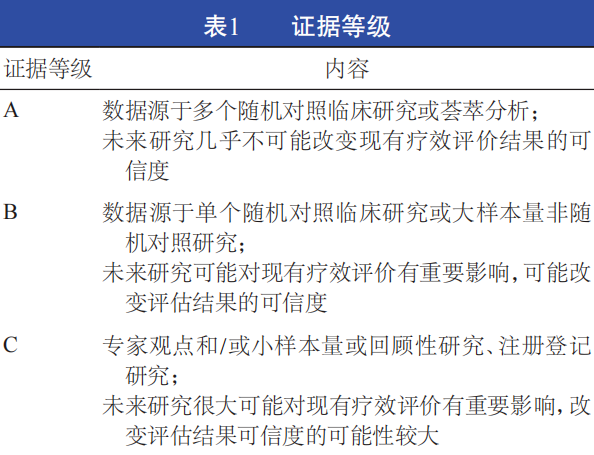
With the rapid development of endoluminal technology, continuous innovation of interventional devices and in-depth understanding of DVT regression, the traditional concept of diagnosis and treatment of DVT can no longer adapt to the current development trend. The Peripheral Vascular Disease Committee of the Chinese Microcirculation Society initiated and organized the expert group of the Lower Extremity Venous Endoluminal Treatment Committee to formulate the key issues and consensus outline, and the expert group organized the national experts in the field to conduct public discussion and modification for 3 times to finalize the “Expert Consensus on Endoluminal Treatment of Acute Lower Extremity Deep Vein Thrombosis”. The level of evidence and strength of recommendation of this consensus refer to the GRADE classification method, and the details are shown in Tables 1 and 2.

The main etiology of DVT is hypercoagulable state of blood, stagnation of blood flow and damage of vein wall.The risk factors of DVT include primary and secondary factors.The primary factors include antithrombin, protein C, protein S deficiency and anticoagulant antibody syndrome, etc.The secondary factors include trauma, pregnancy, surgery, braking, and malignancy, etc.Therefore, DVT occurs more often in patients with surgical procedures, trauma, prolonged bed rest, braking of the lower limbs, family history, and patients with advanced malignant tumors.
3.1 DVT staging
According to the clinical symptoms and onset time of DVT, it was categorized into acute stage (onset time ≤14 d), subacute stage (onset time 15-30 d), and chronic stage (onset time >30 d).
3.2 DVT typing
DVT is classified as proximal or distal according to the site of DVT; thrombus involving the iliac, femoral and/or popliteal veins, with or without involvement of the deep veins of the calf, is referred to as proximal DVT, which is further classified as iliofemoral and femoropopliteal DVT; thrombus confined to the deep veins of the calf is referred to as distal DVT.
The diagnostic strategy for DVT focuses on the following 3 areas, i.e., evaluation based on the patient's history and clinical symptoms, D-dimer assessment, and imaging tests including venous ultrasound, venography, computed tomography venography (CTV), and magnetic resonance venography (MRV). resonance venography (MRV).
4.1 Symptoms and signs of DVT
Acute lower limb DVT is mainly characterized by sudden swelling and pain in the affected limb, edema of the affected limb, increased muscle tone, increased skin temperature, and tenderness in the posterior calf and/or medial thigh, the femoral triangle, and the affected iliac fossa. Positive Homans' sign (pain in the posterior calf muscle group when the affected limb is straightened and the foot is passively dorsiflexed) and positive Neuhof's sign (localized pain due to compression of the posterior calf muscle group) when the thrombus is located in the muscular venous plexus of the calf.
Patients with severe lower extremity DVT may develop femoral cyanosis and femoral leukoedema, which are the most serious conditions in lower extremity DVT. Clinical manifestations include extreme swelling of the lower extremities, severe pain, shiny greenish-purple skin, low skin temperature accompanied by blisters, disappearance of dorsalis pedis arterial pulsation, strong systemic reaction, and elevation of body temperature, and shock and venous gangrene may occur if not treated in time.
4.2 Stratified diagnostic and treatment strategies for DVT with D-dimer testing
For outpatients and hospitalized patients with suspected DVT, it is recommended that the DVT risk level be assessed based on the patient's history, symptoms, and signs. Due to the low specificity of the D-dimer assay, it is recommended to rule out the diagnosis of DVT in patients with low or intermediate risk of DVT. For patients at high risk for DVT, D-dimer testing is not necessary and imaging is sufficient to make a definitive diagnosis.
4.3 Venous ultrasound
Venous ultrasound is the imaging method of choice for the diagnosis of DVT, with high sensitivity and accuracy, and is widely used in clinical practice for screening and monitoring. For patients with negative ultrasound results but persistent or worsening symptoms, repeat ultrasound or angiography is needed.
4.4 CTV and MRV
The use of CTV and MRV as independent diagnostic tools for patients with suspected DVT has not been widely recognized and is not currently appropriate as a routine test. Further pelvic ultrasound, CTV or MRV are needed to clarify the diagnosis only for specific patients, such as obesity, suspected DVT in the inferior vena cava-iliac vein segment or pelvic mass.
4.5 Venography
Shunt venography is currently the gold standard for the diagnosis of lower extremity DVT and is effective in determining the presence or absence of thrombus, the location and extent of thrombus, the time of formation and collateral circulation. However, venography is invasive and has limitations in patients with renal insufficiency and allergic reactions to contrast media.
Determine the DVT risk level of patients with suspected DVT based on their clinical signs and symptoms and adopt appropriate diagnostic strategies (Level of Evidence: C; Strength of Recommendation: I); D-dimer is a screening tool for DVT (Level of Evidence: C; Strength of Recommendation: I); venous ultrasound is the first-line imaging test for the diagnosis of DVT (Level of Evidence: C; Strength of Recommendation: IIa); CTV and MRV are the imaging tests for individualized assessment of DVT (level of evidence: C; strength of recommendation: IIa); and cis-venous angiography is the gold standard for definitive DVT diagnosis (level of evidence: C; strength of recommendation: IIa).
Anticoagulation is the basic treatment for DVT, which inhibits thrombus spread, facilitates thrombus autolysis and lumen recanalization, and reduces the incidence of PE and morbidity and mortality. All patients with DVT should receive anticoagulation therapy for at least 3 months. Anticoagulant drugs include subcutaneous injection of low molecular heparin or intravenous continuous administration, vitamin K antagonist (VKA) or direct oral anticoagulant (DOAC). Anticoagulation therapy for patients with special types of DVT, such as infants and children and during pregnancy, should refer to the consultation guidelines or consensus of the relevant specialties.
Although anticoagulation is the basic treatment for DVT, anticoagulant drugs do not have the effect of dissolving fibrin, and some patients may still develop moderate or severe PTS after aggressive anticoagulation. early thrombus removal by endoluminal therapy can help to recirculate venous flow and protect the function of the venous valves, preventing the development of venous hypertension, and reducing the incidence or severity of PTS. In addition, compared with traditional anticoagulation, endoluminal therapy can effectively reduce the residual thrombus after treatment and lower the risk of recurrence of DVT. Currently, endoluminal treatments for lower limb DVT mainly include catheter-directed thrombolysis (CDT), percutaneous mechanical thrombectomy (PMT), large-lumen catheter aspiration, balloon dilatation and stenting. Stenting.
PMT has become the first choice of surgical treatment for thrombus removal through mechanical aspiration and/or catheter suction, rapid thrombus removal, and opening of occluded veins to alleviate the symptoms of the affected limbs, especially for patients with severe symptoms (femoral bruising) and high thrombus load of DVT. In addition, residual thrombus that cannot be removed by PMT can be combined with CDT to achieve the goals of reducing the dose of thrombolytic drugs, lowering the rate of thrombolysis-related bleeding complications, and shortening the duration of the disease. The purpose of the disease duration.
6.1 Indications and contraindications for PMT
Adaptation:(1) Acute proximal or total lower extremity deep vein DVT, patients with good systemic condition, expected survival > 1 year, and low to moderate bleeding risk; (2) Acute proximal or total lower extremity deep vein DVT with relative contraindications to thrombolysis, such as post-surgical, postpartum, or elderly patients; (3) Subacute iliofemoral vein DVT with obvious symptoms; (4) Femoral bruising; and (5) Recurrence of acute proximal DVT based on PTS of the deep veins of the lower extremities. recurrent acute proximal DVT on the basis of deep vein PTS of the lower extremity.
Contraindications:(1) chronic phase DVT; (2) deep vein PTS; and (3) distal segment DVT.
6.2 Types and characteristics of PMT devices
Common clinical PMT devices can be categorized into rheological thrombus removal devices, rotational thrombus removal devices, and large lumen catheter thrombus aspiration devices according to their working principles.
6.2.1 Rheostatic thrombolytic devices
Representative species:The Medrada Thrombus Aspiration System is a rheostatic thrombus removal device commonly used in clinical practice today and consists of 3 components: a single-use catheter, a single-use pumping device, and a pump drive unit.
Fundamentals:By applying Bernoulli's principle of hydrodynamics, the high-speed jet of sterile saline produces a local vacuum effect at the tip of the catheter, and the thrombus is sucked in by the inflow holes on the corresponding position of the catheter, and then crushed by high pressure inside the catheter, and then suctioned with the flow of water into the waste fluid bag. For relatively old thrombus, a certain amount of thrombolytic drug is injected into the thrombus by high pressure to break up and dissolve the thrombus before thrombus aspiration.
Clinical Scope:Medrada Thrombus Aspiration System device is an effective treatment for DVT in patients with acute iliofemoral vein or whole limb type DVT and low to medium risk of bleeding, which can quickly open the occluded vein, relieve the symptoms of patients with severe DVT faster and save the valve function. Meanwhile, combined CDT treatment can reduce thrombolytic time and thrombolytic dose, and increase the effect of thrombus clearance.
Complications:The Medrada Thrombus Aspiration System causes less damage to the endothelium of the blood vessels, but during aspiration it can cause mechanical damage to the red blood cells in the blood, resulting in intravascular hemolysis, elevation of the broken cell membranes in the blood, and consequently hemoglobinuria and even acute kidney injury. Therefore, the total working time of the Medrada Thrombus Aspiration System for aspiration of thrombus is recommended to be no more than 8 minutes. In addition, the reduction of complications can be achieved through enhanced hydration and alkalinization of the urine in the perioperative period.
6.2.2 Rotary thrombus removal devices
Representative species:The more common rotary thrombus removal device in China is the Straub, a device that consists of 3 parts: a drive unit, a thrombus removal catheter, and a thrombus collection kit.
Fundamentals:The high-speed rotating spiral device creates a stable vacuum zone within the thrombus removal catheter, allowing the thrombus to enter the thrombus removal catheter and be transported into the thrombus collection bag.
Clinical Scope:The Straub device has been shown to be effective in the treatment of lower extremity DVT, with proven efficacy and safety. Similar in clinical scope to the Medrada Thrombus Aspiration System, the Straub device provides immediate restoration of venous blood flow, accelerates swelling in the affected extremity to improve symptoms, reduces thrombolytic time and dose of thrombolytic agents, and reduces the potential risk of bleeding.
Complications:Since the Straub device removes thrombus by mechanical rotation may cause venous intima-media damage (venous wall damage/rupture), the thrombus removal time should not be too long. Especially when removing old thrombus and passing through stenotic lesions, it is important to stop the thrombus suction operation in time if abnormal vibration or sound of the instrument occurs to prevent vascular damage, guide wire breakage, and so on.
6.2.3 Large-lumen catheter/sheath thrombus aspiration devices
Representative species:Manual aspiration thrombectomy (MAT) is the most commonly used thrombus aspiration device, mostly using catheters/sheaths of more than 8F, which is characterized by simple operation, fast thrombus aspiration speed, and low price, etc. Other large-lumen catheter/sheath aspiration devices include the Indigo device, which is equipped with proprietary catheter-tracking and thrombus mechanical separation systems. Other large lumen catheter/sheath aspiration devices include the Indigo device with its proprietary catheter tracking and thrombus mechanical separation system.
Fundamentals:The thrombus is physically aspirated by delivering a large diameter catheter/sheath to the lesion site and using manual/mechanical suction to create negative pressure.
Clinical Scope:MAT combined with CDT, balloon angioplasty and stenting is the first-line endoluminal treatment for acute and subacute lower extremity DVT combined with iliac vein compression syndrome and femoral bruxism, while minimizing the risk of bleeding complications, especially in patients with contraindications to thrombolytic therapy.MAT is inexpensive and easy to perform, which is beneficial for hospitals that do not have other mechanical thrombus-removal devices. MAT is inexpensive and simple to perform, which is conducive to its popularization and implementation in hospitals that do not have other mechanical thrombolytic devices, as well as shortening the overall length of hospital stay for fewer patients and reducing their financial burden.
Complications:MAT aspiration may result in a large amount of thrombus and blood being aspirated in a short period of time, causing a decrease in the patient's hemoglobin level; therefore, MAT should be chosen with caution in anemic patients.In addition, because MAT requires multiple catheter entries and exits, the patient may experience longer procedure times and radiation exposure times, and MAT has limited utility in relatively old thrombotic lesions.
Currently, CDT is a commonly used method of endoluminal thrombolysis, which provides patients with more precise and effective thrombolytic therapy by reducing systemic drug exposure and lowering the risk of systemic hemorrhage compared with previous systemic systemic thrombolysis.CDT places a thrombolytic catheter directly to the thrombus site and pumps a relatively low dose of thrombolytic agents, such as urokinase, recombinant streptokinase, the novel thrombolytic drug reteplase ( recombinant human tissue-type plasiminogen (r-tPA) or tenecteplase-type plasiminogen (TNK-tPA), etc., to achieve the purpose of rapid thrombus dissolution. During CDT, normal heparin anticoagulation is used to control the activated partial thromboplastin time (APTT) at 1.5~2 times of the normal value.
7.1 Indications and contraindications for CDT
Indications: acute central DVT (iliac and femoral veins) or whole-limb DVT; good general condition; expected survival > 1 year and low risk of bleeding complications.
Contraindications: (1) allergy to thrombolytic drugs; (2) recent (within 2-4 weeks) active bleeding, including severe intracranial, gastrointestinal and urinary tract bleeding; (3) recent major surgery, biopsy, cardiopulmonary resuscitation, and puncture that can not be performed with compression; (4) recent severe traumatic injuries; (5) severe and uncontrollable hypertension, i.e., blood pressure ﹥180/100mmHg (1mmHg= 0.133kPa); (6) severe hepatic or renal insufficiency; (7) bacterial endocarditis; (8) history of acute hemorrhagic or ischemic stroke; (9) aneurysm, aortic coarctation, and arteriovenous malformations; (10) age > 75 years, pregnant women.
7.2 Complications of CDT and Points to Note
The most common complication of CDT is bleeding. Although the dose of thrombolytic drugs used in CDT is relatively small compared with systemic systemic thrombolysis, it is necessary to actively reduce the risk of bleeding associated with thrombolytic drugs and intravenous catheter placement, and the following key points need to be paid attention to: (1) patients who have had recent active bleeding, surgery or trauma, severe liver disease, known bleeding disorders, abnormalities in coagulation or platelet counts or function, and recent cerebral infarcts patients should cautiously undergo or avoid CDT treatment; (2) selection of long-acting anticoagulants and continuous assessment of coagulation function during thrombolysis; (3) precise intraoperative manipulation, and ultrasound-guided access to the vein should be obtained to avoid bleeding-related complications caused by puncture; (4) during the period of thrombolysis, the patient should be placed on bed rest, and the limb in which the catheter is left in place should avoid activity, and timely attention should be paid to signs of possible bleeding (e.g., obvious peri-catheter oozing, hematoma formation, etc.), in addition, the level of fibrinogen (FIB) should be detected every 4 hours, and the thrombolytic dose should be reduced by half when FIB ﹤1.5g/L, and thrombolysis should be stopped when FIB ﹤1g/L; (5) arterial puncture and intramuscular injections should be minimized; (6) the progress of thrombolysis should be assessed by imaging at 24-48 h after CDT, in order to adjust the thrombolytic strategy in a timely manner. The following is a summary of the results of thrombolysis.
Both PMT and CDT therapy are relative indications for inferior vena cava filter implantation, and retrievable filters should be chosen whenever possible. If prophylactic inferior vena cava filter implantation has been performed, the filter should be removed as soon as possible after complete clearance of the lower extremity venous thrombus or after the risk of thrombosis has been reduced and adequate anticoagulation is available to avoid filter-related complications.
Iliofemoral vein stenosis and occlusion is one of the important factors leading to the occurrence and progression of DVT, therefore, for DVT patients with iliofemoral vein stenosis and occlusion after thrombectomy, PTA and stent implantation are needed to relieve chronic stenosis and occlusion of iliofemoral vein. In the case of relatively complete thrombus removal, if iliofemoral vein stenosis of >50% is still found on imaging, one-stage stent implantation is recommended.
Stent implantation in the iliofemoral vein is recommended after adequate PTA, and the following points should be noted in the selection of stents: (1) try to choose a special stent for the iliofemoral vein with a certain degree of compliance and sufficient support; (2) the diameter of the implanted stent should be equal to or slightly larger than the diameter of the neighboring normal vessels, to prevent stent occlusion caused by the stent's chronic regression, and perform posterior dilatation when necessary; (3) the length of the stent should be sufficient to cover the stenotic segment; (4) if the (4) If the blood flow in the inflow tract is insufficient, stent implantation should not be performed in one stage; (5) It is not recommended to implant stents in the middle and distal femoral vein, popliteal vein and infrapopliteal vein.
PMT is the first choice of treatment for acute DVT involving the iliofemoral vein, especially for patients with severe symptoms, high thrombus load and relative contraindications to CDT (Level of Evidence: A; Strength of Recommendation: IIa); for patients with DVT with stenosis or occlusion of the common iliac/femoral vein, one-stage PTA and stent implantation of the common iliac/femoral vein (Level of Evidence: C; Strength of Recommendation: IIb) is recommended, on the premise that thrombus is adequately cleared, and the inflow/outflow tract is good. implantation (Level of Evidence: C; Strength of Recommendation: IIb); postoperative standardized anticoagulation therapy lasts for at least 6 months, supplemented by venous active drugs and elastic compression therapy (Level of Evidence: C; Strength of Recommendation: I).
After 2~3d after thrombolysis by retained catheter, patients may have mild fever, body temperature is 37.5~38.5℃, the cause of fever may be caused by thrombolysis, or the retained catheter itself with a pyrogen, or both, this situation often does not need special treatment, if necessary, can be replaced after strict disinfection of the catheter or extubation. Pay attention to other underlying diseases that may cause hypercoagulability. Young patients should be especially concerned about the presence of primary risk factors such as connective tissue disease, antiphospholipid thrombosis syndrome, AT-III deficiency, protein C deficiency, protein S deficiency, etc. Elderly patients should be especially concerned about the presence of secondary risk factors such as malignant tumors, long-term use of medication, and cardiorespiratory insufficiency. It is recommended to take oral anticoagulants directly after acute DVT intervention, at least until 6 months after the operation; low molecular heparin subcutaneous injection can also be used in the postoperative period, once every 12 hours, and at the same time, oral warfarin, and start to detect the international normalization ratio (INR) of the prothrombin time on the 4th day after the operation, and wait until the INR is controlled at 2~3, and then the INR is reduced to 2~3, and the INR is reduced to 3. When the INR was controlled at 2~3, low molecular heparin was stopped, and oral warfarin was continued until at least 6 months after surgery. For patients who have developed lower extremity venous insufficiency and are diagnosed with lower extremity deep vein PTS by Villalta score, intermittent pneumatic compression therapy and/or medical compression stockings should be given to the affected limbs for a long period of time to improve the symptoms, and at the same time, symptomatic medications should be used in conjunction with the patients to reduce the swelling, such as hepcidium saponin sodium tablets, meadowsweet flow infusion tablets, and diosmin tablets. Outpatient follow-ups were performed at 1, 3, 6, and 12 months postoperatively, and imaging or color Doppler ultrasound follow-ups were performed at 6 and 12 months postoperatively, and once a year after 1 year.
Corresponding author:
Yuehong Zheng (Peking Union Medical College Hospital, Chinese Academy of Medical Sciences)
Xinwu Lu (The Ninth People's Hospital of Shanghai Jiao Tong University School of Medicine)
Minyi Yin (Ninth People's Hospital, Shanghai Jiaotong University School of Medicine)
Ye Kaichuang (Ninth People's Hospital, Shanghai Jiaotong University School of Medicine)
Experts who participated in the discussion and revision of this consensus (ranked by surname in Hanyu Pinyin):
Cai Fanggang (The First Affiliated Hospital of Fujian Medical University) Chen Quan (Dongguan Hospital of Southern Medical University) Cao Wendong (Baiqiu'en Hospital of Shanxi Province) Cui Mingzhe (Henan Provincial People's Hospital) Dang Yongkang (Chifeng Municipal Hospital) Deng Hongping (People's Hospital of Wuhan University) Deng Jie (Affiliated Hospital of Guizhou Medical University) Guan Qiang (Shanxi Provincial People's Hospital) Guan Yunbiao (Union Medical College of Fujian Province) Guo Mingjin (Qingdao University Hospital) Guo Mingjin (Affiliated Hospital of Qingdao University) Guo Pingfan (The First Affiliated Hospital of Fujian Medical University) Hao Yingxue (Southwest Hospital of Army Medical University) He Ju (Tianjin First Central Hospital) Hou Peiyong (Liuzhou Workers' Hospital) Hu Hejie (Anhui Provincial Hospital)Huang Jianhua (Xiangya Hospital, Central South University) Huang Wen (The First Affiliated Hospital of Chongqing Medical University) Huang Xiaojin (Zhongshan Hospital, Xiamen University) Huang Xintian (The Ninth People's Hospital of Shanghai Jiaotong University School of Medicine) Li Huagang (The First Affiliated Hospital of Anhui University of Traditional Chinese Medicine) Li Xiaoqiang (Gulou Hospital of Nanjing University School of Medicine) Li Yiqing (Union Hospital of Huazhong University of Science and Technology Tongji Medical College) Li Zhen ( Li Zhen (The First Affiliated Hospital of Zhengzhou University) Liang Siyuan (Taizhou Municipal Hospital) Liang Wei (Renji Hospital of Shanghai Jiao Tong University School of Medicine) Liu Fengyun (The First Affiliated Hospital of Gannan Medical College) Liu Jianlong (Beijing Jishuitan Hospital) Liu Qiang (The First Affiliated Hospital of Nanchang University) Liu Yong (The Affiliated Hospital of Southwest Medical University) Lu Xinwu (The Ninth Affiliated People's Hospital of Shanghai Jiao Tong University School of Medicine) Lu Shaoying (The First Affiliated Hospital of Xi'an Jiao Tong University) Shaoying Lu (Xi'an Jiaotong University) Canhua Luo (Foshan First People's Hospital) Shaomang Lin (Second Affiliated Hospital of Guangzhou Medical University) Jiancang Ma (Second Affiliated Hospital of Xi'an Jiaotong University) Fei Mei (Yichang Central People's Hospital)Minyi Yin (The Ninth People's Hospital of Shanghai Jiao Tong University School of Medicine) Chaowen Yu (The First Affiliated Hospital of Bengbu Medical College) Shuiting Zhai (Henan Provincial People's Hospital) Dongming Zhang (The Second Affiliated Hospital of Dalian Medical University) Hongkun Zhang (The First Affiliated Hospital of Zhejiang University School of Medicine) Feng Zhang (The Second Affiliated Hospital of Hebei Medical University) Jinchi Zhang (The First Affiliated Hospital of Fujian Medical University) Jian Zhang (The First Affiliated Hospital of China Medical University) Yanrong Zhang (The Third Hospital of Hebei Medical University) Lei Zhang (The First Hospital of Hebei Medical University) Shuguang Zhang (The First Affiliated Hospital of Shandong First Medical University) Wangde Zhang (Beijing Chaoyang Hospital of Capital Medical University) Jun Zhao (The Sixth People's Hospital of Shanghai Jiao Tong University School of Medicine) Yu Zhao (The First Affiliated Hospital of Chongqing Medical University) Wenjun Zhao (Taizhou Hospital of Zhejiang Province) Yuehong Zheng (Peking Union Hospital, Chinese Academy of Medical Sciences) Zheng Yuehong (Peking Union Medical College Hospital, China) Zhu Guoxian (Shenzhen Second People's Hospital, China)Mei Jiacai (The Sixth People's Hospital of Shanghai Jiao Tong University School of Medicine) Meng Qingyi (Jinan Central Hospital) Meng Qingyou (The First People's Hospital of Shanghai Jiao Tong University School of Medicine) Qi Ming (The First Affiliated Hospital of Dalian Medical University) Qin Xiaoxiao (The First Affiliated Hospital of Guangxi Medical University) Qiu Jiehua (The Second Affiliated Hospital of Nanchang University) Ren Chuanyuan (The People's Hospital of Inner Mongolia Autonomous Region) Shi Zhenyu (Zhongshan Hospital, Fudan University) (Zhongshan Hospital, Fudan University) Song Xiaojun (Peking Union Medical College Hospital, Chinese Academy of Medical Sciences) Wan Shengyun (The Second Affiliated Hospital of Anhui Medical University) Wang Haiyang (The First Affiliated Hospital of Guangzhou Medical University) Wang Haofu (The Affiliated Hospital of Qingdao University) Wang Xu (The First People's Hospital of Jining City) Wang Ya (Nanyang City Center Hospital) Xiong Guozhuo (The Second Affiliated Hospital of South China University) Xiong Xiaowei (The First Hospital of Nanchang City) Xu Dunyuan (Yantai Yantaishan Hospital of Yantai) Xue Guanhua (Renji Hospital, Shanghai Jiao Tong University School of Medicine) Yao Chen (The First Affiliated Hospital of Sun Yat-sen University)
Conflict of interest All authors declare no conflict of interest
References: omitted
Source of information: Expert Consensus on Endoluminal Treatment of Acute Lower Extremity Deep Vein Thrombosis. Journal of Vascular and Endoluminal Vascular Surgery