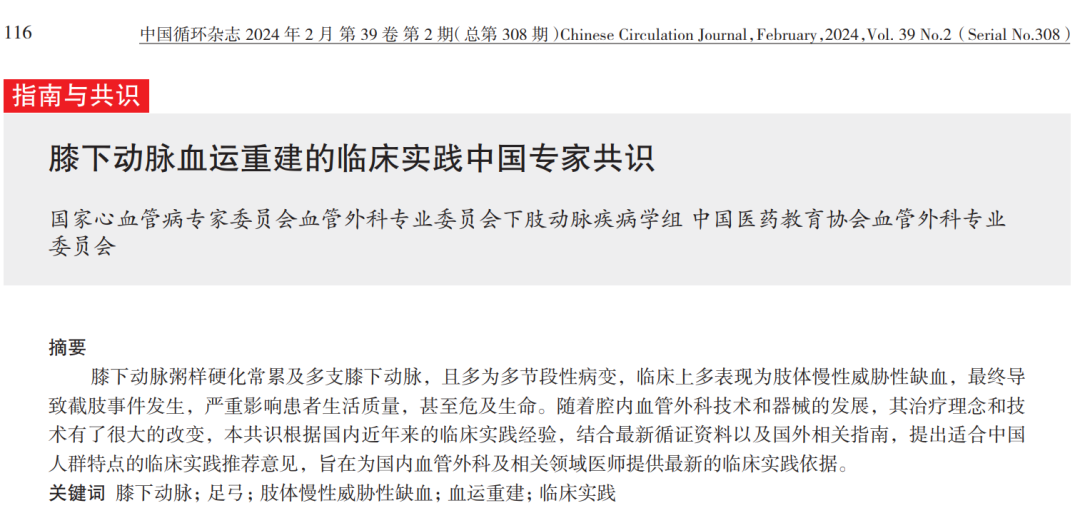
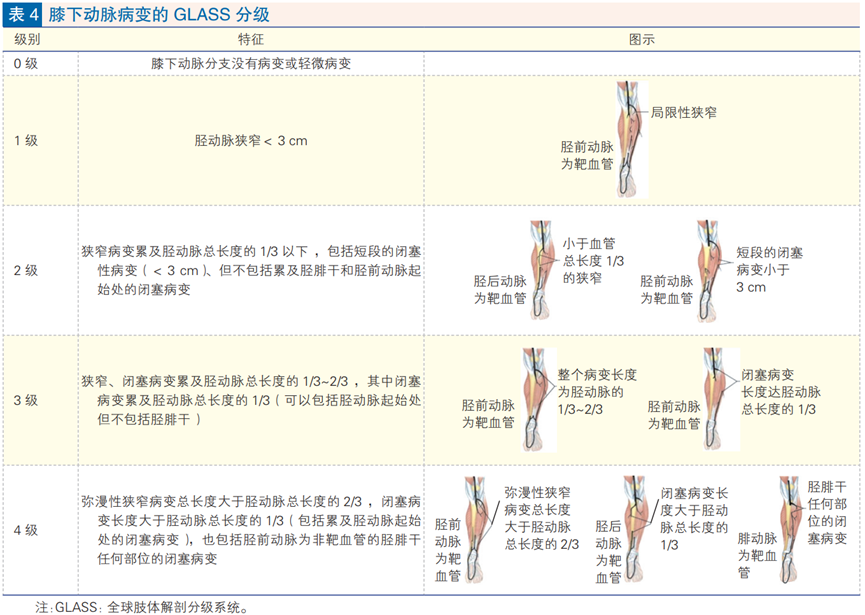
Infrapopliteal atherosclerosis often involves multiple infrapopliteal arteries and is often a multisegmental lesion, which clinically manifests as chronic threatening ischemia of the limb, ultimately leading to amputation events, which seriously affects the quality of life of patients and is even life-threatening. With the development of endoluminal vascular technology and devices, its treatment concept and technique have changed greatly. Recently, the Lower Extremity Arterial Disease Group of the Vascular Surgery Committee of the National Committee of Experts on Cardiovascular Diseases formulated and released the Chinese Expert Consensus on Clinical Practice of Below-Knee Arterial Revascularization, which puts forward recommendations for clinical practice suitable for the characteristics of the Chinese population, with the aim of providing physicians in the field of vascular surgery and related fields in China with the basis for the most up-to-date clinical practice. Anatomical characteristics of the infrapopliteal artery and typing of lesions 01 Anatomical features of the infrapopliteal artery The distal popliteal artery is divided into the anterior tibial artery, peroneal artery, and posterior tibial artery; the anterior tibial artery is the first branch, which continues downward into the dorsalis pedis artery, which in turn gives off a deep plantar branch, the arcuate artery and so on; the popliteal artery is divided into the anterior tibial artery and continues into the tibial fibular trunk, which is further divided into the peroneal artery and posterior tibial artery, which runs along the back of the lower leg between the deep and superficial flexor muscles, and then passes through the back of the inner ankle into the sole of the foot, and is then divided into two branches, the internal plantar artery and the external plantar artery. It divides into two branches: the internal plantar artery and the external plantar artery. The dorsalis pedis artery is mostly connected to the lateral plantar artery via the deep plantar branch, forming the dorsalis pedis arterial arch. 02 Staging of infrapopliteal arterial lesions In 2015 the Transatlantic Collaboration (TASC) published the first international classification of infrapopliteal artery lesions, the TASC II classification.The 2019 Global Guidelines for the Management of Threatening Ischemia in the Chronic Limb propose a new global limb anatomical classification system - the GLASS classification. -GLASS classification, in which the classification of infrapopliteal arterial lesions (table below) differs from the TASC II classification in that it places more emphasis on the pathology of whether the completely occluded lesion involves the tibiofibular trunk and tibial artery opening. Treatment modalities for infrapopliteal artery disease non-surgical treatment Patients with combined atherosclerotic lesions of the infrapopliteal arteries are usually older and have more comorbidities. Therefore, good metabolic management, including hypoglycemia, antihypertension, lipid regulation, anticoagulation, antiplatelet, and vasodilator drugs, is the basis of treatment. Pharmacological treatment with vasodilators, antiplatelet agents, and anticoagulants is the basis for treatment of below-knee arterial ischemia, but most patients with severe lower limb ischemia do not achieve symptomatic improvement and limb preservation through pharmacological treatment. Therefore, for patients with severe ischemia for whom conventional medical treatment is ineffective, hemodynamic reconstruction therapy must be adopted. 02 hemodialysis Resting pain (Fontaine stage 3, Rutherford grade 4) or presence of ulcers/gangrene (Fontaine stage 4, Rutherford grades 5-6); Poorly improved infrapopliteal outflow tracts in femoropopliteal artery reconstruction therapy; In the presence of milder symptoms such as numbness and coldness in the foot that do not respond to medication, and in the absence of other etiologies, reconstruction of the infrapopliteal artery may be performed at the discretion of the patient to improve the local blood supply. Presence of uncorrected hemodynamic instability due to severe systemic infection and presence of uncorrectable coagulation abnormalities; Known history of severe contrast allergy; Recent cardiovascular accident; Presence of contraindications to antiplatelet or heparin therapy. Patients with rest pain (Fontaine stage 3, Rutherford grade 4) or the presence of ulcers/gangrene (Fontaine stage 4, Rutherford grades 5-6) should be aggressively revascularized. Patients with diabetic foot should undergo aggressive below-knee arterial revascularization based on comprehensive medical therapy. In the case of ischemia combined with severe foot infection, it is recommended that hemodialysis should be taken aggressively after clearing and draining the foot and controlling the infection. In cases of ischemia combined with severe gangrene of the foot, aggressive preoperative hemodialysis is recommended for amputation/toe. In patients with good saphenous vein conditions, autologous saphenous vein bypass grafting from the popliteal to infrapopliteal arteries may be preferred if systemic conditions permit. Not many studies have directly compared the efficacy of surgical open surgery and endoluminal treatment for infrapopliteal arterial lesions. Although the BEST-CLI study showed that the efficacy of extra-anatomic bypass grafting of the autologous saphenous vein was superior to endoluminal treatment, in view of the fact that patients with CLTI are mostly of advanced age and high risk, difficult to tolerate open surgery, and lack of good vein grafts, endoluminal treatment is increasingly becoming the preferred treatment for infrapopliteal arterial occlusions due to the advantages of less invasiveness, quicker recovery, ease of tolerability, and reproducibility. The efficacy of endoluminal therapy is improving with the development of techniques and devices. The main goal of hemodialysis is to improve the blood supply to the ischemic trauma of the foot and to establish a straight line of blood flow to the ischemic trauma of the foot as much as possible. Currently, revascularization of the infrapopliteal artery is based on simple balloon dilatation, and the diameter of the balloon can be measured by DSA or with the aid of extracorporeal ultrasound and endovascular imaging [intravascular ultrasound (IVUS) or optical coherence tomography (OCT)]. For stenotic lesions, a straight or curved 0.014“ or 0.018” infrapopliteal guidewire can be used to open the stenosis. For chronic total occlusion (CTO) lesions, true intraluminal opening should be pursued, with the option of a specialized 0.014“ or 0.018” guidewire. Subendocardial opening is also a common method of opening the infrapopliteal artery. If the downstream opening attempt fails, the distal branch vessels can be selected for retrograde puncture, trans-lateral branch, or retrograde opening via the dorsal plantar arch of the foot. When target vessel spasm occurs during hemodialysis, intravascular push injection of antispasmodics (e.g., nitroglycerin 100-200 μg) or local balloon delayed dilation may be considered. Attempts at revascularization of multiple vessels are feasible when technique permits, but should still be evaluated on a case-by-case basis and on a risk/benefit basis. Overall, hemodialysis is beneficial in shortening the healing time of the wound under the guidance of both the normal below-knee artery branch foot supply zoning (Angiosome) system and the adequate and complete vascular staining of the ischemic area of the foot as assessed by intraoperative angiography to obtain the Angiographosome system, both of which have similar limb preservation results in diabetic patients. Since the pathology of infrapopliteal artery lesions is different from that of the femoropopliteal artery and there is a lack of stents suitable for infrapopliteal artery application, some special balloons can be tried to obtain a better lumen. Specialized balloons can be classified according to their principle of action as “pressure-focused dilatation” and “controlled dilatation”. “Pressure-focused dilatation” is the use of scoring balloons, cutting balloons, etc. to dilate the lesion, thereby reducing the formation of entrapment. “Controlled dilatation” utilizes the cushioning effect created by the relatively low-pressure zone created by the guidewire bundle on the surface of the “chocolate balloon” to minimize damage to the intima and reduce the formation of clips. In severely calcified lesions, the application of shockwave balloons with endovascular lithotripsy techniques helps to obtain better lumen access. Endoluminal volume-reducing devices (directional spinning, laser ablation, etc.) can also be used in infrapopliteal arterial lesions, but the indications need to be carefully selected. Drug (paclitaxel or rapamycin)-coated balloons suitable for the infrapopliteal artery, based on adequate target lesion vessel preparation, have been helpful in improving the 12-month one-stage patency rate of the infrapopliteal artery, but more clinical study data are needed to confirm this. For short-segment lesions of the infrapopliteal artery or lesions presenting with severe elastic retraction and flow-limiting entrapment, there is clinical evidence that drug-eluting stents (rapamycin) can achieve a better rate of first-phase patency, and that fractional stents can be used for localized entrapment management. Rehabilitation of the infrapopliteal artery in patients with diabetes mellitus should aggressively open up blood flow directly to the ischemic area of the foot. Complete arch reconstruction is important for wound healing, and dorsal plantar archplasty can be applied to reconstruct the arch when conditions permit. Plain balloon dilatation is preferred for revascularization of the infrapopliteal artery, with special balloons, volume-reducing devices, drug-coated balloons, and stents when available. If conditions permit, try to utilize 2D/3D perfusion angiography intraoperatively to quantify foot perfusion in real time, thereby improving mid- and long-term outcomes. 03 Medication and postoperative care Dual antiplatelet therapy (75mg clopidogrel + 100mg aspirin) is recommended postoperatively. Rivaroxaban 2.5mg twice/day and aspirin 100mg once/day may also be considered in CLTI patients with low bleeding risk and concomitant coronary artery disease. Lipid-lowering therapy should also be optimized and risk factors for atherosclerosis should be aggressively controlled. Traditional Chinese medicine (TCM) treatments including various types of internal formulas for symptom identification and external lotions have a role in symptom relief and postoperative tonification, especially in the management of limb ischemia or infected wounds, TCM has unique methods and advantages. 04 Postoperative follow-up management Patients with localized trauma should receive trauma care in a specialized trauma center or outpatient clinic. Moderate exercise should be encouraged when the patient's condition permits. Standardized outpatient follow-up is recommended at 1, 3, 6, and 12 months postoperatively, including clinical improvement, wound examination, and pulse, ABI, transcutaneous PaO2 (tissue perfusion monitoring), and Doppler ultrasound. Patient adherence to medication should be monitored during clinical follow-up. Article source: Lower Extremity Arterial Disease Group of the Vascular Surgery Committee of the National Committee of Experts on Cardiovascular Diseases, Vascular Surgery Committee of the Chinese Association for Medical Education. Chinese expert consensus on the clinical practice of below-knee arterial revascularization. Chinese Journal of Circulation. 2024;39(2):116-122.