Author:Cardiothoracic Group of the Chinese Medical Association Radiology Branch Corresponding author:Minwen Zheng, Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University, Xi'an 710032, China; Email: zhengmw2007@163.com; Bin Lv, Department of Radiological Imaging, Fu Wai Hospital, National Center for Cardiovascular Diseases, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing 100037, China, Email: blu@vip.sina.com; Zhengyu Jin, Department of Radiology, Peking Union Medical College, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100730, China, Email: jin_zhengyu@163.com; Shiyuan Liu, Department of Diagnostic Radiology, The Second Affiliated Hospital of Naval Medical University, Shanghai 200003, China, Email: cjr.liushiyuan@vip.163.com.
Aortic coarctation is one of the most life-threatening cardiovascular emergencies, and symptomatic acute ascending aortic coarctation in particular is very dangerous, with a mortality rate of 1% to 2% per hour after the onset of symptoms [ 1 , 2 ], and the mortality rate is further increased when combined with complications such as pericardial tamponade, acute myocardial ischemia or infarction, stroke, and poor organ perfusion [ 1 ]. In patients with acute type B aortic coarctation without complications, the 30-day mortality rate is 10% [ 1 ].
Imaging examinations are crucial for the diagnosis of aortic coarctation, especially CT angiography (CTA) of the aorta, which has become the examination of choice for definitive diagnosis [ 3 ] and has generated a large amount of medical imaging data. Artificial intelligence (AI) has seen rapid development in the medical field in recent years, especially in the processing and application of imaging big data, and its preliminary research in aortic coarctation, including the use of convolutional neural networks to predict the risk of aortic coarctation rupture on CTA images [ 4 ] , the establishment of aortic coarctation auxiliary diagnostic models based on integrated learning The establishment of an integrated learning-based aortic clamp assisted diagnostic model [ 5 ] , the use of deep learning models to predict the risk of aortic clamp in-hospital death, acute kidney injury, and the length of stay in the postoperative intensive care unit, etc. [ 6 , 7 , 8 ] . These studies basically require uniformly labeled image data, and the quality and accuracy of the labeling will directly affect the effectiveness of the AI model. At present, although there is a clinical database of aortic coarctation [ 9 ], the CT image database, which is the most important for diagnosis, is still blank. Moreover, multicenter image big data annotation faces problems such as different sources of image data, varying image quality, and inconsistent annotation methods. Meanwhile, the long coverage of aortic coarctation lesions, the difficulty of identifying and measuring the rupture and the true/false lumen due to the influence of beating artifacts, and the difficulty of labeling due to the involvement of many branches have also largely limited the promotion and application of AI imaging studies of aortic coarctation.
Based on this, the Cardiothoracic Group of the Radiology Branch of the Chinese Medical Association has organized cardiovascular imaging experts in the industry to prepare an expert consensus on CTA data annotation of aortic coarctation, aiming to establish a standard for CTA image annotation of aortic coarctation, so as to promote the application of AI technology in the accurate diagnosis, risk prediction, decision-making guidance, etc. of aortic coarctation (this annotation consensus does not include aortic intramural hematoma, and it does not involve the assessment of aortic coarctation postoperatively and the evaluation of complications, etc.). assessment and evaluation of complications, etc.).
一、Definition and staging of aortic dissection
The wall of the aorta is divided into three layers: intima, media and periphery. Aortic dissection is a serious cardiovascular emergency in which the aortic wall is torn due to a rupture of the intima-media, resulting in the entry of blood into the intima-media layer and expanding in the direction of the aorta's long axis, which may involve the branch arteries [ 10]. After the wall is torn, it splits into two layers, and the lumen forms a true lumen and a false lumen. There may be no traffic between the true and false lumens during the process of tearing, or there may be traffic through the reperforation. The direction of endothelial sheet tearing is either prograde or retrograde.
There are two commonly used types of aortic coarctation: DeBakey's type and Stanford's type, which classify aortic coarctation according to the location of the rupture and the extent of the tear as type I (rupture in the ascending aorta, with a distal tear involving the aortic arch, descending aorta, etc.), type II (both the rupture and tear are located in the ascending aorta, with distal extension), and type III (the rupture is located in the thoracic aorta and extends to the distal part of the aorta. The Stanford classification mainly considers the extent of the tear rather than the location of the rupture, and is divided into type A (the tear involves the ascending aorta) and type B (the tear does not involve the ascending aorta) according to whether the ascending aorta is involved [ 11], which is related to surgical procedures, and is therefore more frequently adopted by clinics and guidelines [ 2].
二、Labeling requirements
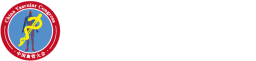
1. Quality control requirements for labeled source images: The scanning process and parameter settings of the original CTA images of aortic coarctation to be included in the labeling should be unified and standardized, in compliance with the following requirements: (1) Scanning equipment: it should be CT scanning of 64 rows or more; (2) Scanning parameters: tube voltage 100 kV [body mass index (BMI) <25 kg/m 2] or 120 kV (BMI≥25 kg/m 2), reference tube current 300 mAs, tube current modulation enabled (if available); (3) Scanning range: routine from the thoracic inlet to the pubic symphysis; if the patient has combined neurological symptoms, the scanning range should include the carotid artery from the angle of the mandible to the pubic symphysis; (4) Contrast agent: it is recommended to use the contrast agent with iodine concentration ≥350 mg/ml, and the contrast dose is 1.0~1.2 ml, and the dose of the contrast agent is 1.0~1.2 ml. 1.0~1.2 ml/kg, injection flow rate 4~5 ml/s; (5) Reconstruction kernel: a moderately sharp soft-tissue reconstruction kernel is used (due to the different names of reconstruction kernels from different manufacturers, no specific recommendation is made); (6) Scanning layer thickness and reconstruction layer thickness: 0.75~1.00 mm; (7) Scanning quality control: cardiac gating scanning should be used as much as possible to minimize root sinus pulsation artifacts, but it is limited by the The condition of patients with aortic coarctation is severe, the heart rate of patients is not equal, and non-cardiac gated scanning can also be used in case of emergency; (8) image quality control: the CT value of the aortic lumen should be ≥250 HU [ 12], and the border of the root sinus and the intima-media slice are clear and free of artifacts, or only mild artifacts, but do not affect the border and the intima-media slice outlined in the image can be used for segmentation. Images with obvious respiratory or pulsatile artifacts that prevent assessment and further segmentation should be excluded (Figure 1-4).
Figures 1~4 Schematic diagram of aortic CT angiography (CTA) image quality evaluation. Figure 1 shows that the aortic root sinus is free of any beating artifacts, and the sinus border and intima-media slice are clearly displayed; Figure 2 shows that a slight beating artifact exists in the aortic root sinus, but the aortic sinus border and intima-media slice can be recognized and used for segmentation; Figure 3 shows that the beating artifacts in the aortic root sinus lead to intima-media slice not being able to be clearly displayed and not being able to be evaluated; and Figure 4 shows that there are obvious beating artifacts in the aortic root sinus leading to the aortic sinus border not being clearly visible and Unable to assess
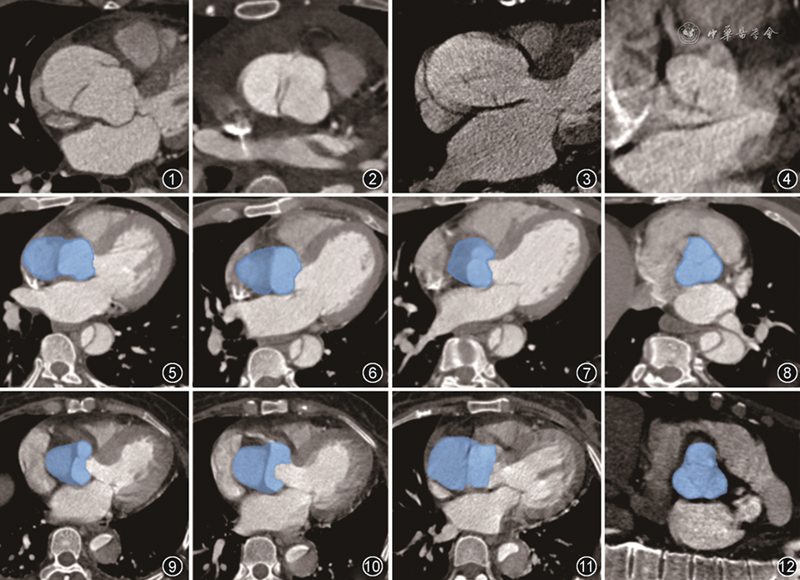
Figures 5 to 8 CTA images of the aortic sinus closure state. Figures 5-7 show the labeling of the sinus closure status (level from bottom to top), the line-like aortic valve edge is poorly displayed but distinguishable, and the labeled portion is in blue color; Figure 8 shows the vertical cross-sectional reorganization of the sinus, which clearly shows that the 3 sinuses present the closure state
Figures 9~12 CTA images of the open state of the aortic sinus. Figures 9~11 show the labeling of the aortic sinus during the open state of the aortic valve (the level is from the bottom to the top), and the line-like edge of the aortic valve is shown clearly and easy to label. Figure 12 shows the vertical cross-section reorganization of the sinus section, which can clearly show that the 3 sinuses present open state
2. Label the source data retention requirements:CTA image data were saved in DICOM format to ensure that there were no missing layers, wrong layers, etc.; the original data could not be modified or edited in any way, and lossy compression could not be performed; the original DICOM format data should be desensitized, and the desensitized information included, but was not limited to, name, age, gender, and hospital name. Research protocols based on labeled source data should be approved by the Ethics Committee in order to fully protect patients' rights and interests and data security.
3. Labeling platform and tool requirements:The selection of image annotation platforms and tools should be adapted to local conditions and time, and the appropriate platforms and tools should be selected according to the situation and conditions and meet the following requirements: (1) meet the requirements of network security and data protection; (2) have basic image reading functions, such as zoom in, zoom out, adjusting the window width/position, panning and rotating, level switching, grayscale inversion, threshold filtering, etc.; (3) have multi-plane reorganization and three-dimensional reconstruction functions, to facilitate accurate and complete measurement, assessment, and outline the marked structure from multiple directions; (4) with basic annotation functions, such as brush sketching, semi-automatic identification, automatic cross-layer, automatic boundary adjustment, automatic filling, fast correction, etc.; (5) in addition to the axial plane image, with the function of annotation in the coronal plane, sagittal plane, and other reorganization of the image; (6) to achieve the different needs of the annotation process, such as two initial labeling, a review, etc.; (7) labeling export format can choose some public formats, such as Nifti, NRRD, RAW, MetaImage, in order to facilitate data exchange. At present, the labeling tools can be divided into stand-alone version and network version, also can be divided into open source version and commercial version. The available annotation tools mainly include Flying Scale, 3D slicer [ 13 ], MITK [ 14 ], ITK-SNAP [ 15 ] and so on, among which Flying Scale is the commercial network version, and 3D slicer, MITK, ITK-SNAP are the open source stand-alone versions.
4. Labeling method:Labeling methods can be manual, semi-automatic, fully automatic, etc., separately or jointly. Different labeling methods may bring heterogeneous differences, but the impact is small. Manual and semi-automatic labeling is less efficient, but accurate and flexible, fully automatic labeling is efficient and fast and convenient, but there will be a lack of detail labeling, which needs to be adjusted manually. In principle, in the case of a variety of ways are available, the first recommended full-automatic or semi-automatic labeling methods, the conditions do not have only manual labeling. This consensus describes the labeling methods are manual labeling, which is the basis of semi-automatic and fully automatic labeling methods.
5. Label the personnel qualification requirements:Labeling personnel play a decisive role in labeling quality, and the labeling team should be composed of labeling physicians, auditing physicians and arbitration physicians. The annotation team must be senior diagnostic cardiovascular imaging physicians, specific requirements: (1) annotation physician: at least 2, radiology diagnostic attending physician, 5 years and more cardiovascular imaging diagnostic work experience; (2) audit physician: at least 1, radiology diagnostic deputy director physician and above, 10 years and more cardiovascular imaging diagnostic work experience; (3) arbitration physician: at least 1, radiology diagnostic director physician, 15 years and more cardiovascular imaging diagnostic work experience. (3) Arbitrator: at least 1 director physician specialized in diagnostic radiology, with 15 years or more working experience in diagnostic cardiovascular imaging.
6. Labeling personnel training and assessment:Based on the content and requirements of this expert consensus, the labeling physicians were uniformly trained. Each person first tries to annotate 5 cases of aortic coarctation CTA image data, and the annotation process is guided and corrected by the auditing physician and/or the arbitration physician, so that the annotating physician will gradually familiarize with the requirements of outlining until he/she is qualified. The qualification criteria are: to be able to accurately outline the entire aortic border, true and false lumen, intima-media sheet and rupture, as well as all the first-level branching vessels in each case, and to ensure that all the edges of the outline are clear and accurate. After familiarizing with the labeling requirements, labeling content, labeling methods and qualification standards, the labeling physician should label at least 5 cases of aortic coarctation CTA image data as an assessment, and the labeling data can only be defined as a qualified labeling physician after the auditing physician and/or the arbitration physician decide that all of them are qualified.
7. Review/arbitration of labeled data:Each case of data to be labeled should be labeled by 2 trained and qualified labeling physicians using a blinded method, comparing the consistency of labeled anatomical structures and lesions, as well as attribute information, etc., and submitting the inconsistent data to the reviewing physician for determination or modification. The review session was performed by at least one reviewer, whose main task was to define the correct side of the inconsistent labeling results and to correct problems such as mislabeling and inaccurate boundaries. If the reviewing physician also has difficult problems that cannot be solved, the arbitration session can be entered, and at least 1 arbitrating physician can be organized to discuss and confirm. After this session, each case has been labeled by 2 physicians and reviewed/arbitrated by at least 1 senior physician.
8. Quality of post-labeling data:All qualified CTA labeling data for aortic coarctation should ensure completeness, consistency, and accuracy.
三、Labeling methodology and content
Before labeling CTA images of aortic coarctation, the labeler should repeatedly browse the images based on axial and multiplanar reorganization to assess the image quality and confirm the tear extent of the aortic coarctation, the true lumen and false lumen, the intima-media sheet and the rupture, and the major branches with or without intima-media sheet involvement. In order to better observe the borders of the aorta and the intima-media sheet, the window width and window position should be adjusted appropriately, with a recommended window width of 600-800 HU and a window position of 100-300 HU. Narrower window widths and higher window positions are chosen to enhance the contrast between the blood vessels and the surrounding tissues, as well as between the intima-media sheet and the false lumen. The labeling content should include the aortic sinus (including the proximal section of the coronary artery), the entire aortic trunk, all the first-order branches of the aorta, the true lumen and the false lumen, the intima-media slice and the rupture, and so on. The specific methods and contents of the labeling are as follows.
1. Labeling of the aortic sinus:The aortic sinus is connected to the left ventricular outflow tract and consists of three sinuses: the left coronary sinus (emanating from the left coronary artery), the right coronary sinus (emanating from the right coronary artery), and the non-coronary sinus (emanating from the non-coronary artery).The three sinuses are surrounded by three semicircular valve leaflets, and the leaflets (i.e., the edges of the sinuses) are linear and low-density, and the sinuses surrounded by the leaflets are filled with blood and are high-density. When labeling with axial images, regardless of whether the aortic sinus is closed (Figure 5-8) or open (Figure 9-12), the sinus anatomy can be observed dynamically up and down, confirming the upper and lower boundaries of the sinus, and then sketching along the edges of the sinuses layer by layer. Care should be taken to avoid drawing the left ventricular outflow tract into the sinus.
2. Labeling of the aortic trunk:The aortic trunk is labeled to include the ascending aorta, aortic arch, thoracic aorta, and abdominal aorta. On cross-sectional CTA images, the lumen of the aorta is usually round and dense, and the wall of the aorta is very thin and hypointense, so the outer edge of the wall should be included as much as possible when outlining the aortic trunk (Figure 13-15). When atherosclerotic plaques or other lesions are present in the wall, the wall should be outlined along with the lesions (Figures 16-18). The order of labeling can start from the root of the aorta adjacent to the sinus and go upward along the course of the aorta, or from the end of the abdominal aorta upward layer by layer, after crossing the diaphragm, the ascending aorta and thoracic aorta will appear at the same time, can be labeled at the same time, and go upward until the arch is confluent. In oblique sagittal reconstruction, the ascending, arch and descending segments of the aorta can be presented simultaneously in one image, which facilitates a wide range of outlining and labeling of the aortic trunk, and the labeling speed is faster (Figure 19-21).
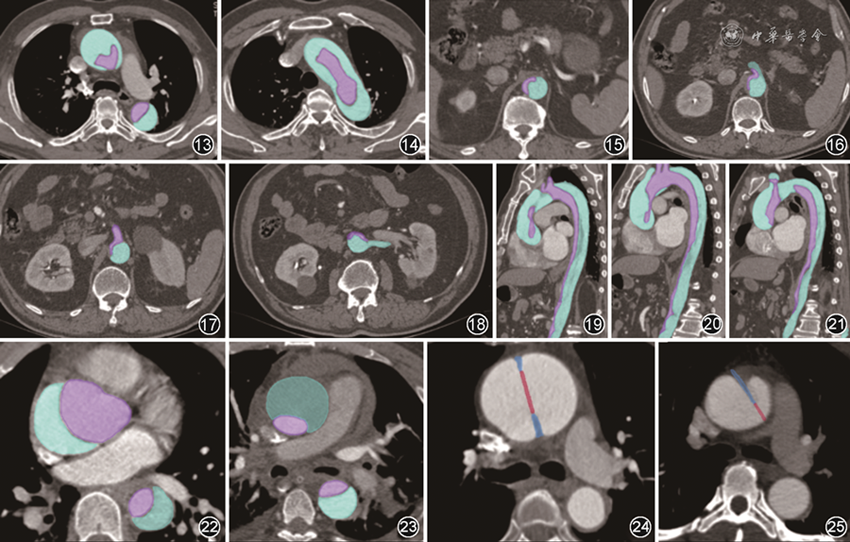
Figures 13 to 18 Six typical cross-sectional aortic trunk labeled CT angiography (CTA) images. Figure 15 shows the level of the abdominal aorta, the abdominal aorta is close to the left anterior part of the spine, sketch the outer edge of the wall of the aorta and differentiate between the true lumen (purple) and the false lumen (cyan) inside the lumen; Figures 16-18 show the level of the abdominal trunk (Fig. 16), the superior mesenteric artery (Fig. 17), and the level of the renal arteries on one side (Fig. 18), sketch the outer edges of the wall of the abdominal aorta and its branches and then differentiate between true lumen and false lumen borders, especially pay attention to the true and false lumens inside the branches
Figures 19~21 3 oblique sagittal plane aortic trunk labeled CTA images. Oblique sagittal reconstruction images can show the ascending, arching and descending segments of the aorta and its branches in a wide range, and outline the outer edge of the aortic wall as well as the true lumen (purple) and false lumen (cyan) with higher speed and efficiency
Figures 22, 23 CTA images of cross-sectional true lumen and false lumen labeling of type A entrapment in the thoracic aorta. Figure 22 shows that the tear of the intima-media sheet involves the whole aorta, and the true lumen (purple) should be outlined along the inner edge of the ascending aorta and thoracic aortic wall and the lateral edge of the true lumen of the intima-media sheet in the cross-sectional image; the false lumen (cyan) is outlined along the inner edge of the ascending aorta and thoracic aortic wall and the lateral edge of the false lumen of the intima-media sheet; Figure 23 shows that there is low-density thrombosis in the false lumen of the ascending aorta, and the false lumen is outlined with the edge of the low-density as the The boundaries are outlined
Figs. 24, 25 CTA images of a cross-sectional intima-media sheet and rupture labeling of a type A entrapment in the thoracic aorta. Figure 24 shows that the lumen of the ascending aorta is obviously enlarged, the middle part of the low-density thread-like intima-media sheet (blue) is broken and missing, and the two ends of the thread-like structures are attached to the anterior and posterior walls of the ascending aorta, respectively; the outlines should include the true lumen side, the false lumen side, and the fracture end of the intima-media sheet, and the rupture between the fracture ends of the two sides of the intima-media sheet (red) is outlined separately; Figure 25 shows that the lumen of the ascending aorta is obviously enlarged, and the false lumen is seen to be a small amount of low-density thrombi Figure 25 shows a clearly enlarged lumen of the ascending aorta with a small amount of low-density thrombus in the false lumen and a low-density thread-like intima-media sheet (blue) attached to the anterior wall of the ascending aorta, with a breach (red) at the left posterior defect of the free end of the dissection, which should be outlined separately
3. Labeling of true and false cavities:The torn intimal sheet divides the intact aortic lumen into true and false lumens. Recognition of the true and false lumen on CTA images of aortic coarctation is usually not difficult. The true lumen is usually smaller and denser, and the false lumen is usually larger and less dense, showing a beak or beak sign at the ends that border the true lumen on axial images. The true lumen should be outlined along the inner edge of the aortic wall (i.e., lumen side) and the true lumen-side edge of the intima-media sheet; the false lumen should also be outlined along the inner edge of the aortic wall (i.e., lumen side) and the false lumen-side edge of the intima-media sheet (Figure 22). When the false lumen is essentially thrombus-filled, the boundary of the false lumen is outlined with the medial border of the outer edge of the low-density wall (Figure 23).
4. Labeling of inner membrane pieces and ruptures:The endothelial sheet of a high-density aortic luminal tear shows a linear, low-density shadow that is extremely thin. The image should be enlarged when labeling and both edges of the intimal sheet should be carefully outlined. When it is difficult to distinguish the border between the low-density intimal sheet and the low-density false lumen, it is necessary to try to narrow the window width and raise the window position to make the demarcation between the intimal sheet and the false lumen more obvious, and then outline the edge of the intimal sheet on the side of the false lumen in conjunction with the visual assessment. It should be noted that when the endocardial sheet has a pulsatile double line-like shadow, it should be uniformly sketched layer by layer in accordance with the line-like shadow close to the true lumen side.
The rupture is a low-density linear discontinuity in the intima-media sheet on the CTA image.The rupture of a type A dissection is usually located in the aortic root, which is often poorly visualized due to pulsation artifacts, while the rupture of a type B dissection is usually located in the descending arch, which is poorly affected by pulsation and is often clearly visualized. Re-rupture can also exist in the aortic arch, thoracic aorta, and abdominal aorta. Due to the equal density of the rupture and the true and false lumen, it is difficult to use the threshold-based method for semi-automatic segmentation, and is usually obtained by manual outlining. After magnifying the image, along the direction of the tangent line of the intima-media sheet, connecting the intima-media sheet or connecting the intima-media sheet and the aortic wall, and outlining the thickness of the same as the intima-media sheet, it can be used to manually outline the edge of the true lumen side of the intima-media sheet, the edge of the false lumen side, and the edge of the fractured end of the consecutive interruptions; and the interruption between the fracture ends of the intima-media sheet of both sides is outlined separately The rupture between the ends of both endosseous segments is outlined separately (Figure 24), and when the rupture is on one side, the rupture should be defined by the anterior tendency of the broken end of the endosseous segment (Figure 25). When the rupture artifacts are large and difficult to recognize on axial images, the rupture should be flexibly labeled after multidirectional observation in combination with multiplanar reconstructed images to obtain the accurate boundary of the rupture. Similarly, all re-ruptures need to be labeled in the same way. The intima-media slice can be obtained by logical calculation using the intact aorta, true lumen, and false lumen, and the logical calculation can be performed by customizing the code through the outlining software platform, and then corrected manually.
5. Labeling of aortic branches:(1) Labeling of the coronary arteries: the right and left coronary arteries emanate from the right and left coronary sinuses of the aorta, and the proximal coronary arteries can often be extended in the case of endothelial sheet tears in the sinus of the aorta in type A entrapment, which should include the proximal segment of the right coronary artery, the left main trunk, the proximal segment of the anterior descending branch (Figure 26), and the proximal segment of the circumflex branch in the labeling. If a non-gated scan is used, artifacts in the root sinus and coronary arteries can be particularly large, and the coronary arteries may not be labeled at this time.
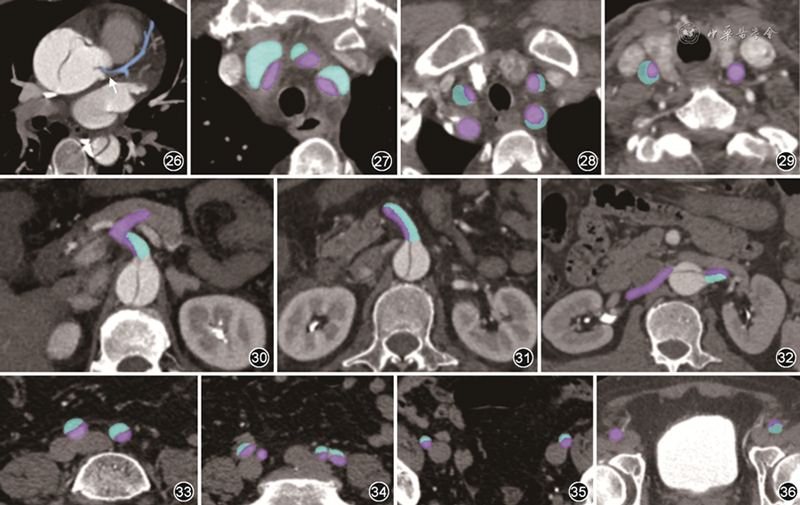
Figures 26 to 36 CT angiography (CTA) images of the labeled branches of aortic coarctation. Figure 26 shows the labeling of the coronary arteries, and the cross-sectional image shows the tearing of the sinus intima-media sheet involving the left main trunk (blue), the formation of low-density thrombus in the false lumen (↑), and the labeling of the left main trunk (blue) and the proximal segment of the anterior descending branch; Figures 27-29 show the labeling of the supra-arterial branches, and the labeling of the tearing-involved left subclavian, left common carotid, and innominate arteries from the bottom to the top, one by one, respectively (Figure 27), the bilateral subclavian arteries and the bilateral carotid lower common carotid arteries (Figure 28), and middle common carotid arteries bilaterally (Figure 29), and the true lumen (purple) and false lumen (cyan) of the tear-involved supra-archicular branches were labeled separately; Figures 30 to 32 show the labeling of the abdominal aortic branches. The tear-involved celiac trunk arteries (Figure 30), superior mesenteric arteries (Figure 31), and bilateral renal arteries (Figure 32) were labeled layer by layer from top to bottom on the cross-sectional images, with the true lumen (purple) and false lumen (cyan), respectively; and the iliofemoral arteries were labeled in Figures 33 to 36. Bilateral common iliac arteries (Figure 33), bilateral internal and external iliac arteries (Figure 34), bilateral external iliac arteries (Figure 35), and bilateral femoral arteries (Figure 36) involved in the laceration were labeled layer by layer from the top down, with the true lumen (purple) and false lumen (cyan) labeled, respectively
(2) Labeling of supra-arch branches: The supra-arch branches of the aorta are thicker and include the innominate artery, bilateral subclavian arteries and bilateral common carotid arteries. The method of labeling branch vessels and true and false lumens is the same as that of the aorta and true and false lumens. On the axial image, the branch vessels are in the form of round lumens, and their boundaries can be carefully outlined along the edges of the branch vessels, and in the order from bottom to top, from the beginning of the arch of each branch upward layer by layer, to the uppermost limit of the scan of the common carotid artery (Figs. 27-29), and the true and false lumens of the branch involvement can be labeled as above. The branches of the suprachiasmatic artery can also be outlined extensively on coronal or sagittal reorganization images.
(3) Labeling of the branches of the abdominal aorta: the abdominal aorta emits the celiac trunk artery, superior mesenteric artery, bilateral renal arteries and inferior mesenteric arteries from the top to the bottom, respectively, and should be labeled as far as possible with the entire length of the celiac trunk and its branching arteries, the upper and lower mesenteric arteries, and the entire length of the bilateral renal arteries (Figs. 30-32). The labeling method is the same as above.
(4) Labeling of iliac/femoral arteries: the bifurcation of the end of the abdominal aorta continues into the bilateral common iliac arteries, which emanate from the external iliac arteries and the internal iliac arteries, respectively, and the external iliac arteries continue downward into the femoral arteries. When labeling and outlining, the bifurcation can be labeled from top to bottom, the internal iliac arteries are labeled until the plane of the bifurcation, and the external iliac arteries to the femoral arteries are labeled until the lower limit of the scanning image (Figures 33~36).
四、Labeling reference process
Considering the actual clinical work and scientific research needs, referring to the mammography database construction method proposed by the Radiology Branch of the Chinese Medical Association [ 16], and the process of labeling liver lesions and colon cancer [ 17 , 18], the reference process for labeling CTA images of aortic coarctation and constructing a standardized database for CTA of aortic coarctation is shown in Figs. 37 and 38.
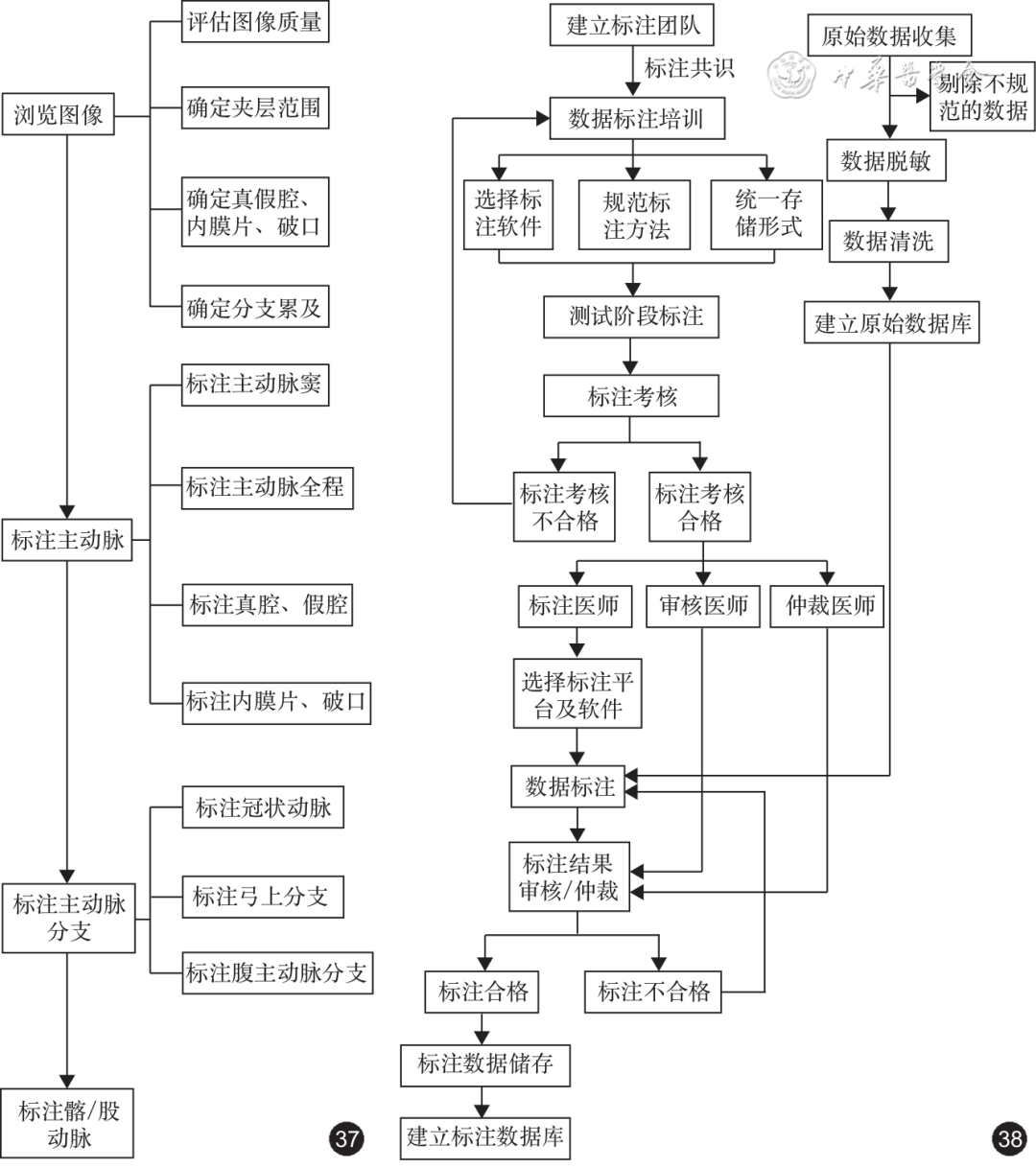
Figs. 37, 38 Flowchart of aortic dissection CT angiography image annotation (Fig. 37) and standardized database construction (Fig. 38)
五、Wrap-up
Acute aortic coarctation is a cardiovascular emergency with a high mortality rate, high risk of rupture, and many complications. CT imaging-based methods allow timely and accurate assessment of CTA signs and diagnosis. The establishment of a unified and standardized CTA annotation database for aortic coarctation is the basis for the use of AI technology to establish pre-diagnostic models, guide therapeutic decisions, and perform risk and prognostic assessments. This consensus on the annotation content, annotation requirements, and annotation process for aortic coarctation CTA image data provides strong technical guidance and quality assurance for the construction of a standardized aortic coarctation CTA annotation image database, and helps to validate, optimize, and promote the aortic coarctation AI image model, thus promoting the clinical application of the aortic coarctation AI image, and ultimately benefiting the patients.
Author: Jingsheng Xu (Department of Diagnostic Radiology, Xijing Hospital, Air Force Military Medical University), Xiaohu Li (Department of Medical Imaging, The First Affiliated Hospital of Anhui Medical University), Bing Liu (Department of Diagnostic Radiology, Xijing Hospital, Air Force Military Medical University), Hongliang Zhao (Department of Diagnostic Radiology, Xijing Hospital, Air Force Military Medical University)
Members of the Group of Experts Diagnostic Department, The Second Affiliated Hospital of Naval Medical University), Chunhong Hu (Department of Radiology, The First Affiliated Hospital of Soochow University), Yi He (Department of Radiology, Beijing Friendship Hospital of Capital Medical University), Yang Hou (Department of Radiology, Shengjing Hospital of China Medical University), Zhengyu Jin (Department of Radiology, Peking Union Medical College of the Chinese Academy of Medical Sciences, Peking Union Medical College, Peking Union Medical College, Peking, China), Dong Li (Department of Imaging and Medicine, General Hospital of Tianjin Medical University), Xiaohu Li (Department of Li Xinchun (Department of Radiology, The First Affiliated Hospital of Guangzhou Medical University), Liu Bing (Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University), Liu Hui (Department of Radiology, Guangdong Provincial People's Hospital), Liu Shiyuan (Department of Diagnostic Radiology, The Second Affiliated Hospital of Naval Medical University), Lu Minjie (Department of Magnetic Resonance Imaging, Fu Wai Hospital, National Center for Cardiovascular Diseases, Peking Union Medical College, Chinese Academy of Medical Sciences), Lv Bin ( Lv Bin (Department of Radiography, Fu Wai Hospital, National Center for Cardiovascular Diseases, Peking Union Medical College, Chinese Academy of Medical Sciences), Ma Yue (Department of Radiography, Shengjing Hospital, China Medical University), Peng Chengbao (Neusoft Research Institute of Intelligent Medical Science and Technology, Shenyang), Peng Liqing (Department of Radiography, Huaxi Hospital of Sichuan University), Pu Hong (Department of Radiography, Sichuan People's Hospital of Sichuan Academy of Medical Sciences), Wang Haiyan (Department of Medical Imaging, Provincial Hospital of the First Medical University of Shandong). Provincial Hospital of Shandong First Medical University), Wang Jian (Department of Radiology, The First Affiliated Hospital of Army Medical University), Wang Rongpin (Department of Medical Imaging, Guizhou Provincial People's Hospital), Wang Ximing (Department of Medical Imaging, Provincial Hospital of Shandong First Medical University), Wang Yan (Radiology and Imaging Center, People's Hospital of Xinjiang Uygur Autonomous Region), Wang Yining (Department of Radiology, Peking Union Medical College of the Chinese Academy of Medical Sciences, Peking Union Medical College, Peking Union Medical College, Peking, China), Wen Ti DiDi (Radiology Department, Xijing Hospital of Air Force Military Medical University, Beijing) Department of Diagnostic Radiology, Xijing Hospital, Air Force Military Medical University), Wu Jiang (Department of Medical Imaging, Shanxi Hospital of Cardiovascular Diseases), Wu Lianming (Department of Radiology, Renji Hospital, Shanghai Jiaotong University School of Medicine), Xiao Yi (Department of Diagnostic Radiology, The Second Affiliated Hospital of Naval Medical University), Xing Yan (Imaging Center, The First Affiliated Hospital of Xinjiang Medical University), Xu Lei (Department of Medical Imaging, Beijing Anzhen Hospital, Capital Medical University), Xu Jingjing (Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University), Xu Maosheng (Department of Medical Imaging, The First Affiliated Hospital of Zhejiang University of Traditional Chinese Medicine), Yang Benqiang (Department of Diagnostic Radiology, General Hospital of the Northern Theater of Operations of the People's Liberation Army), Yang Qi (Department of Radiology, Chaoyang Hospital of Capital Medical University), Yu Jing (Department of Medical Imaging, Zhongshan Hospital of Dalian University), Zhang Jiayin (Department of Radiology, Shanghai First People's Hospital), Zhang Lynn (Editorial Board of the Chinese Journal of Radiology Editorial Office), Longjiang Zhang (Department of Diagnostic Radiology, General Hospital of the Eastern Theater of the People's Liberation Army), Tong Zhang (Department of Medical Imaging, The Fourth Affiliated Hospital of Harbin Medical University), Xia Zhang (Neusoft Corporation), Xiaochun Zhang (Department of Imaging, Affiliated Women's and Children's Medical Center of Guangzhou Medical University), Xiaoqin Zhang (Department of Medical Imaging, People's Hospital of Inner Mongolia Autonomous Region), Weiguo Zhang (Department of Zhang Yan (Department of Imaging, Guizhou Medical University Hospital), Zhang Yonggao (Department of Radiology, The First Affiliated Hospital of Zhengzhou University), Zhang Zhang (Department of Medical Imaging, Tianjin Medical University General Hospital), Zhao Hongliang (Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University), Zhao Shihua (Department of Magnetic Resonance Imaging, Fuwai Hospital, National Center for Cardiovascular Diseases, Peking Union Medical College, Chinese Academy of Medical Sciences), Zheng Minwen (Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University), Zheng Minwen (Department of Diagnostic Radiology, Xijing Hospital, Air Force Medical University) (Department of Diagnostic Radiology, Xijing Hospital, Air Force Military Medical University), Zhu Li (Department of Radiology, General Hospital of Ningxia Medical University)
References (omitted)
Reprinted from the Chinese Journal of Radiology