华中科技大学同济医学院附属协和医院
董念国教授

Guest authors
LIU Ming, WANG Yixuan, DONG Nianguo, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, China
Heart failure is the only disease in the field of cardiovascular disease that is currently showing a growing trend. With the continuous growth of China's economy and the aggravation of the aging population, the number of cardiovascular disease patients in China is now about 330 million, of which there are about 8.9 million people with heart failure. Studies have shown that heart failure has a 5-year mortality rate of 50%, and in severe cases, the 1-year mortality rate is as high as 50%, and heart failure has become one of the most important causes of threat to human health. Since the world's first successful heart transplantation in 1967, after more than 50 years of development, heart transplantation has become the most effective treatment for end-stage heart failure. However, the shortage of donor hearts has severely constrained the development of heart transplantation, and only about 6,000 heart transplants are performed worldwide each year, which cannot meet the continuously increasing demand for end-stage heart failure treatment. After more than 50 years of development, the technology of mechanical circulatory assist (MCS) has become more mature, and it can partially or completely replace the function of the heart, and has become an effective treatment for patients with heart failure.
MCS can be categorized according to the duration of assistance into durable MCS (dMCS) and temporary MCS (tMCS); according to the mode of use into implantable, extracorporeal, and percutaneous interventional; according to the assisted ventricle into: biventricular assist device (BiVAD), left ventricular assist device (LVAD), right ventricular assist device ( RVAD), and total artificial heart (TAH); according to the principle of operation into: pacing, rotating (centrifugal or axial flow) devices. RVAD) and total artificial heart (TAH); and according to the principle of operation: pulsatile, rotating (centrifugal or axial flow) devices.The current treatment modalities of MCS can be categorized as bridging to heart transplantation (BTT), recovery transition therapy (BTR), or alternative transplantation end-point therapy (DT).
Short-term Mechanical Cycle Support (tMCS)
Short-term mechanical circulatory assistance (tMCS) is one of the most important tools in the treatment of severe or refractory cardiogenic shock. tMCS rapidly improves systemic perfusion of critical organs, provides effective circulatory support, and provides hemodynamic support and organ perfusion for patients from hours to weeks, bridging the gap between recovery or clinical decision-making (transplantation or long-term mechanical circulatory assistance). Over the past decade, the use of tMCS has increased rapidly worldwide and has become an important technology in the field of heart failure treatment.
Currently, the main tMCS devices commonly used in clinical practice are intra-aortic balloon counterpulsation (IABP), extracorporeal membrane pulmonary oxygenation (ECMO), CentriMag pumps, and percutaneous ventricular assist devices (pVADs) such as the TandemHeart, and the Impella system. tMCS devices are categorized as follows: ① By implantation: percutaneous peripheral vascular implantation, transthoracic center implantation, Hybrid implantation; ② according to the way of blood flow pulsation: axial flow pump, centrifugal pump. IABP and ECMO are the products with more clinical applications in China at present.
Long-term mechanical circulatory assistance (dMCS)
Long-term mechanical circulatory assistance (dMCS) generally refers to MCS assisted for more than 3 months, and is dominated by in vivo implantable LVAD (artificial heart), which is currently dominated by Heart Mate 3 in foreign countries. Although China's artificial heart technology started late, in recent years, under the leadership of academician Hu Shengshou of National Center for Cardiovascular Diseases and Fu Wai Hospital, China's ventricular assistive technology has been developing rapidly, and the number of LVAD implantation has been increasing year by year. At present, there are mainly Evaheart, CH-VAD, Heart Con and CorHeart 6, which is currently the lightest in weight and the smallest in size, registered and marketed through the FDA in China. Long-term MCS indications are: ① advanced heart failure dependent on positive inotropic drugs; ② frequent hospital admissions for heart failure with hypoxemia; ③ progressive cardiogenic cachexia; ④ reversible end-organ dysfunction secondary to low cardiac output; ⑤ 6min walking distance <300 meters; ⑥ poor quality of life with optimal drug therapy, New York Heart Association's Cardiac Function Classification (NYHA) class III-IV; ⑦ Ineffective cardiac resynchronization therapy, etc.
Progress of domestic and international research on mechanical cycling assistance
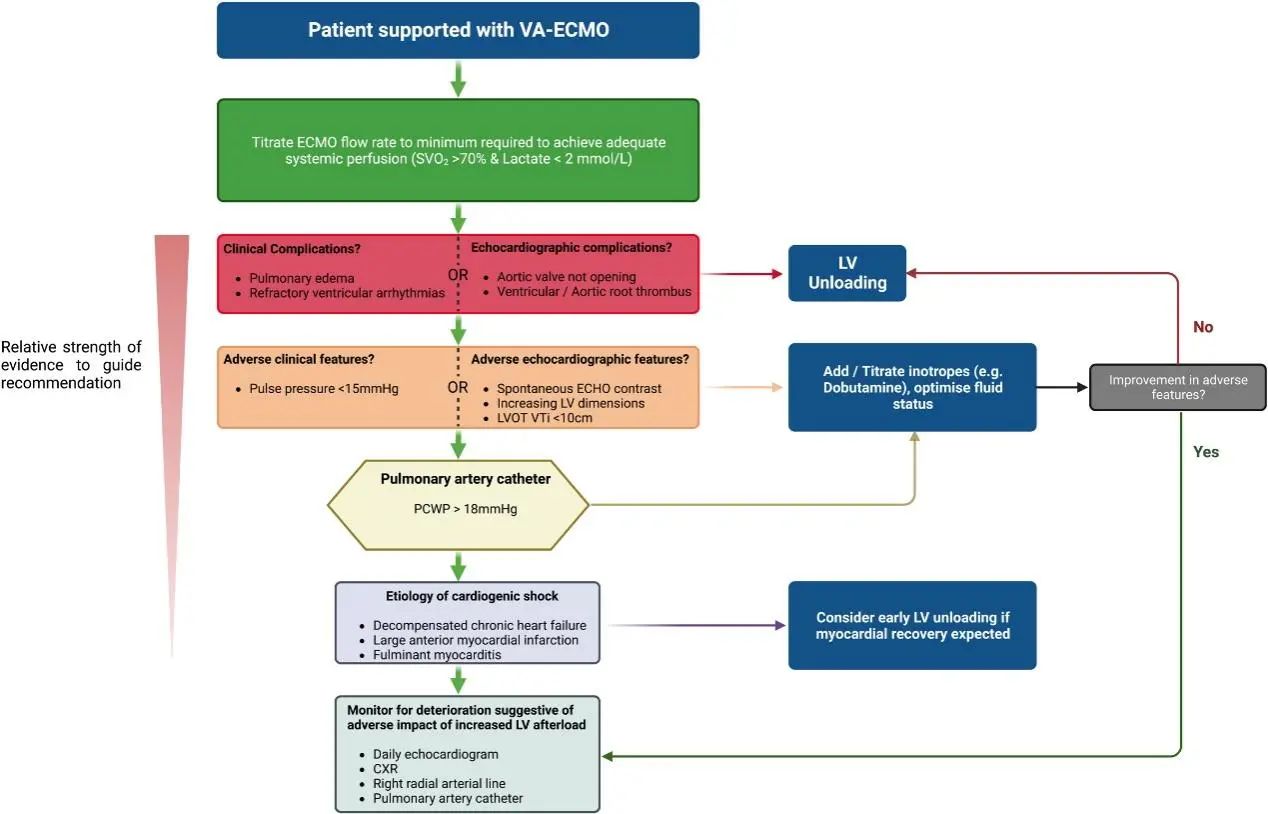
Circulation:Left ventricular unloading during VA-ECMO: who needs it, when to perform it, and how to perform it?Veno-arterial extracorporeal membrane pulmonary oxygenation (VA-ECMO) is a powerful MCS strategy to support systemic perfusion and provide oxygenation for cardiopulmonary support in patients with cardiogenic shock, but this comes at the cost of increased left ventricular ( LV) afterload, and the additional hemodynamic load may impair myocardial recovery, cause LV dilatation, and lead to complications including cardiogenic thrombosis, arrhythmias, and pulmonary edema. Complications. Patients with limited systolic reserve or depleted preload reserve are particularly susceptible to complications associated with increased afterload and may benefit from prophylactic LV unloading.LV unloading can be accomplished through the use of additional circulatory support devices to mitigate the adverse effects of mechanical overload, which may increase the likelihood of myocardial recovery. Whether prophylactic unloading improves myocardial recovery and reduces mortality in patients without adverse consequences of LV afterload is unknown, and the potential benefits of prophylactic unloading must be weighed against the risks of additional MCS devices. The choice of LV offloading depends on the expertise of the local medical staff, and the article presents a recommended process for LV offloading that can help guide medical staff in determining when, for whom, and how best to perform LV offloading in VA-ECMO-supported patients.
Eur J Heart Fail: bridging strategies and cardiac replacement outcomes in patients with cardiogenic shock associated with acute decompensated heart failure.With the current high percentage of patients admitted to cardiac intensive care units for acute decompensated heart failure-related cardiogenic shock (ADHF-CS), there is increasing interest in the optimal treatment options for CS. For eligible patients with ADHF-CS, treatment options include heart transplantation (HTx) or long-term left ventricular assist device (LVAD) implantation. The article describes outcomes associated with bridging long-term left ventricular assist device ( LVAD) or heart transplantation in patients with ADHF-CS. In the American Association of Thoracic Surgeons Adult Cardiac Surgery Database, patients (27,262) aged 18 years or older who underwent HTx or long-term LVAD implantation between 2014 and 2019 were included in the analysis. The primary outcome was operative or 30-day postoperative mortality. Secondary outcomes included postoperative hemorrhage (requiring intervention), cerebrovascular accident, cardiac arrest, prolonged mechanical ventilation, renal failure, and postoperative sepsis or pneumonia. Of the 9783 patients with preoperative CS, 8777 (89.7%) had ADHF-CS. pharmacologic therapy (n = 5013) was the most common bridging strategy, followed by aortic balloon counterpulsation (IABP; n = 2816), catheter-based temporary mechanical circulatory support (TMCS; n = 417), and venoarterial-extracorporeal membrane pulmonary oxygenation (VA-ECMO; n = 465).Patients bridged by VA-ECMO had the highest mortality rate (22%), followed by TMCS (10%), IABP (9%), and medication (7%). Adverse postoperative outcomes were more common with LVAD recipients than with HTx recipients. Among ADHF-CS patients receiving HTx or long-term LVAD, VA-ECMO bridging patients had the highest mortality and adverse events during hospitalization, followed by catheter-based TMCS, IABP, and pharmacotherapy. Postoperative complication rates were higher in patients with bridged LVAD compared with HTx. Prospective trials are needed to determine the optimal bridging strategy for patients with ADHF-CS.

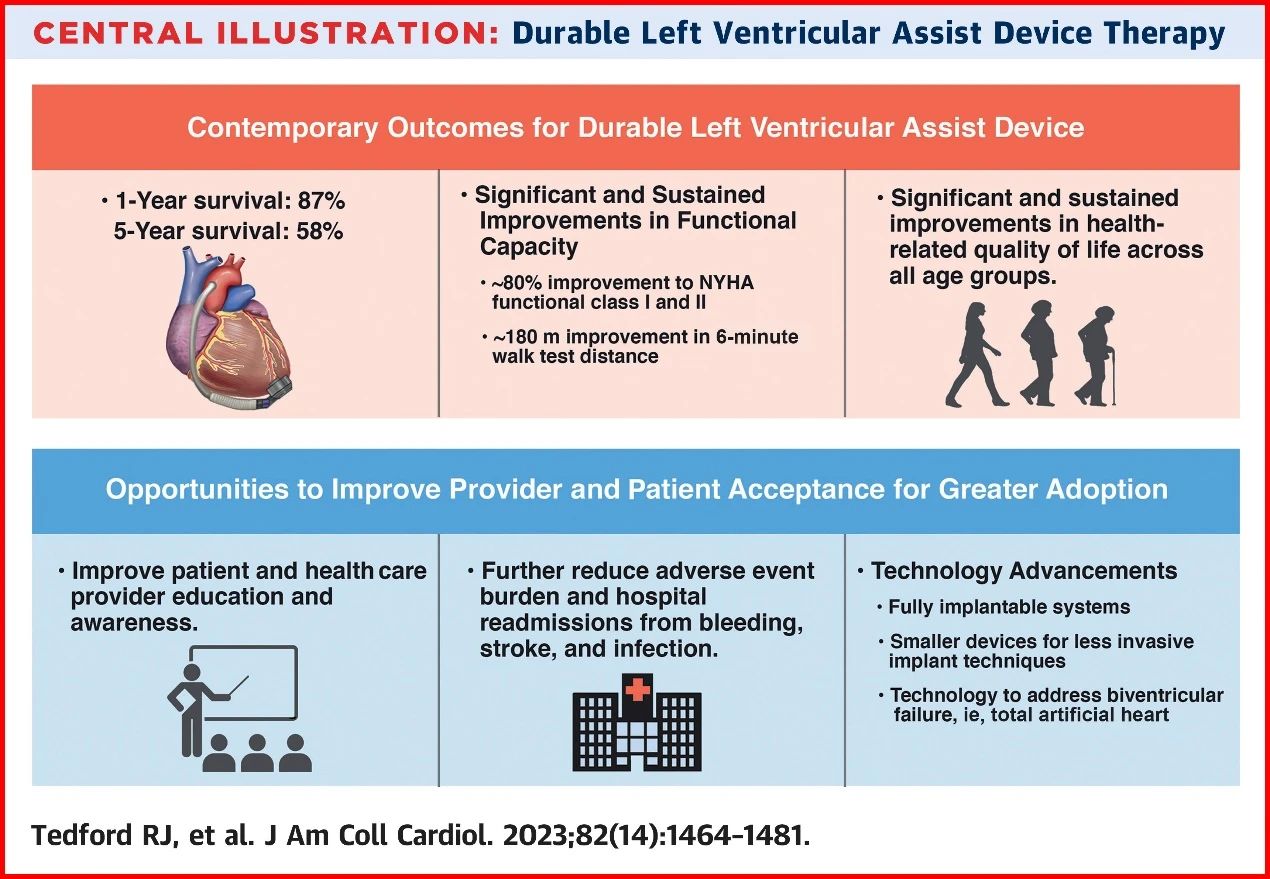
JACC: Long-term Mechanical Circulation Auxiliary Scientific Statement.Despite advances in the pharmacologic treatment of patients with stage C heart failure ( HF), the 5-year survival rate for patients with end-stage heart failure is still less than 20 %. Continuous left ventricular assist device ( dLVAD ) support is an important therapeutic option for patients with advanced HF. innovations in dLVAD technology have reduced the risk of a number of adverse events, including pump thrombosis, stroke, and bleeding. Currently, average 2-year patient survival is similar to that of heart transplantation, and 5-year dLVAD survival is approaching 60 %. However, the use of dLVAD has not yet become more widespread due to delayed referral of patients to advanced heart failure centers, insufficient knowledge among clinicians of current dLVAD outcomes, including quality-of-life improvements, and reduced heart transplantation priority for patients already receiving dLVAD support. Despite the tremendous technological advances in MCS over the past 2 decades, with significant improvements in HRQOL, morbidity, and mortality, gaining wider adoption in patients with advanced HF remains a challenge. trategies for intraoperative management of aortic, mitral and tricuspid valve disease: 1. Aortic valve disease: when the aortic valve is mildly closed, it can be left untreated. When aortic valve closure is moderate or greater, aortic valvuloplasty or prosthetic valve replacement can be considered and needs to be replaced with a bioprosthetic valve to avoid thrombosis.2.Mitral valve disease: Mild to moderate mitral valve closure does not require specific management and can mostly be improved with assistive device support. The need for plasty or replacement in severe mitral valve insufficiency is controversial and is currently recommended to be left untreated.3. Tricuspid valve disease: In moderate to severe tricuspid valve insufficiency, plasty or replacement may be considered to reduce right heart volume and hepatic venous pressure overload. However, recent studies have shown that management of the tricuspid valve alone has not significantly improved right heart function. The need for tricuspid valvuloplasty or replacement requires further study.
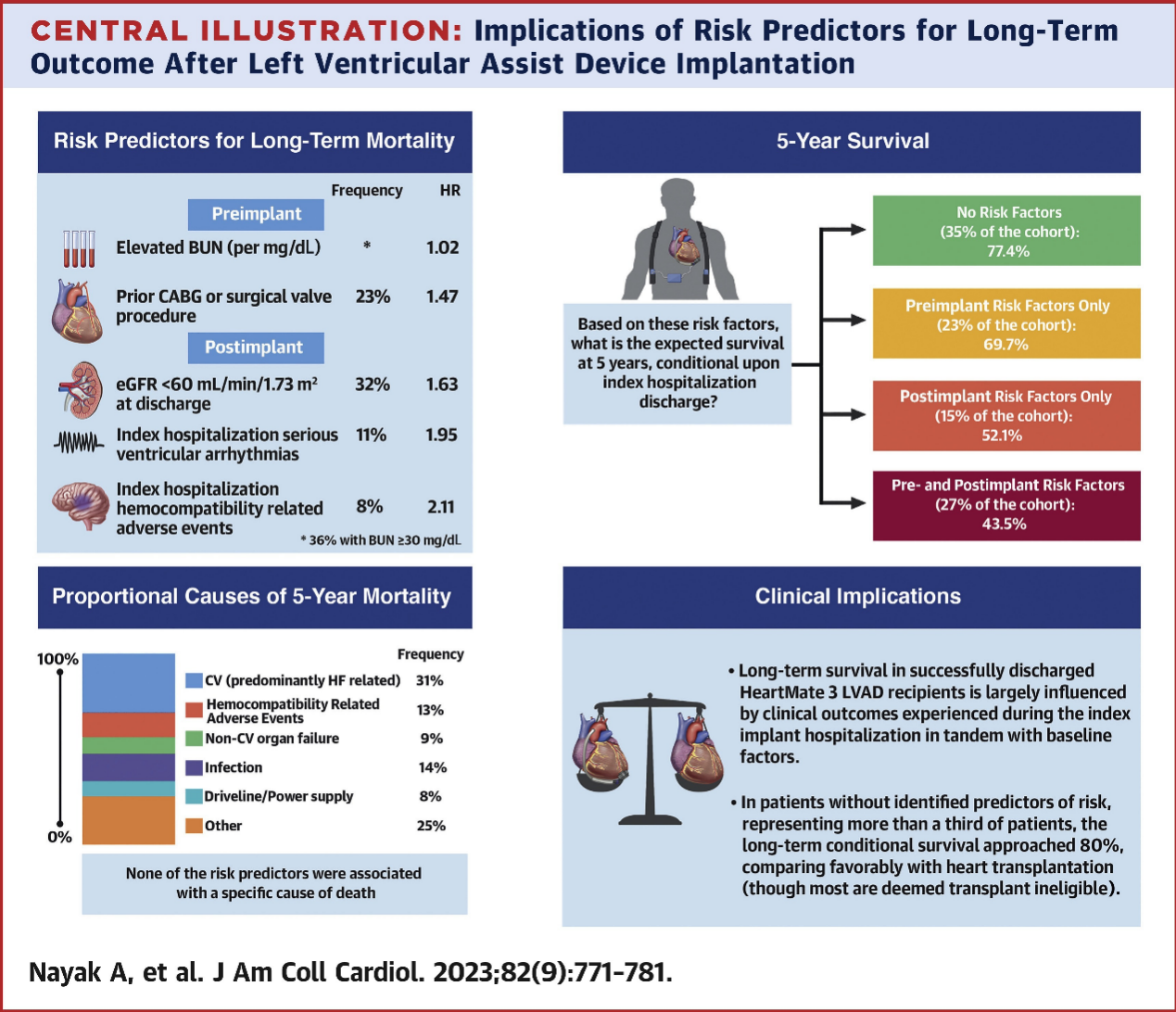
Left ventricular assist devices (LVADs) are an important therapeutic tool for prolonging survival and improving quality of life in patients with medically refractory advanced heart failure. With the introduction of the fully magnetically levitated HeartMate 3 (HM3, Abbott) LVAD, relevant studies have demonstrated significant reductions in blood compatibility-related adverse events (HRAEs) (pump thrombosis, ischemic and hemorrhagic stroke, and nonsurgical bleeding). BACKGROUND: In a recent analysis of data from the pivotal MOMENTUM 3 (Multi-Center Study of Patients Treated with Heartmate 3 Mechanical Circulatory Support) trial, the median survival of patients supported with the HM3 LVAD exceeded 5 years, with 68% of those patients achieving and sustaining significant symptomatic improvement (NYHA Functional Classification I-II) at this time point. However, how preimplantation factors and postimplantation metrics affect 5-year mortality in patients discharged from the hospital with advanced heart failure implanted with HM3 LVADs is unknown. OBJECTIVE: To examine the clinical predictors associated with 5-year postdischarge mortality (total and cause-of-death mortality) in HM3 LVAD recipients. METHODS: Of 515 patients with HM3 LVAD implantation, 30 patients who died during hospitalization for the implantation procedure were excluded and 485 patients (94%) were included in the analysis. Hospitalization characteristics such as pre-implantation (baseline) and post-implantation surgery indicators were analyzed separately as multivariate risk predictors of death at 5 years. RESULTS: Patients (baseline data: median age 62 years, 80 % male, 65 % Caucasian) had a cumulative 5-year mortality rate of 38 %. 2 pre-implantation characteristics (elevated blood urea nitrogen and history of previous coronary artery bypass grafting or valve surgery) and 3 post-implantation characteristics (hemocompatibility-related adverse events, ventricular arrhythmia, and a glomerular filtration rate at discharge of < 60 mL/ min / 1.73 m2) were independent predictors of 5-year mortality. Analysis of patients ( 171 patients, 35.3 %) without any predictors of death reduced 5-year mortality to 22.6 % ( 95 % CI : 15.4 % ~ 32.7 %). Even in patients with 1 or more predictors, the 5-year mortality rate was less than 50 % ( 45.7 % [ 95 % CI : 39.0 % ~ 52.8 % ]). CONCLUSION: Long-term 5-year mortality after successful discharge following HM3 LVAD implantation is largely influenced by clinical events experienced during hospitalization for implantation surgery, as well as by preimplantation factors. Clinical events experienced during hospitalization for implantation surgery included stroke, bleeding, severe ventricular arrhythmia, and renal insufficiency, but overall survival of patients with advanced heart failure who were able to be discharged from the hospital after implantation of an HM3 LVAD exceeded 5 years. In patients without identified prognostic risk factors, long-term mortality after discharge may be reduced and comparable to reported heart transplant mortality.
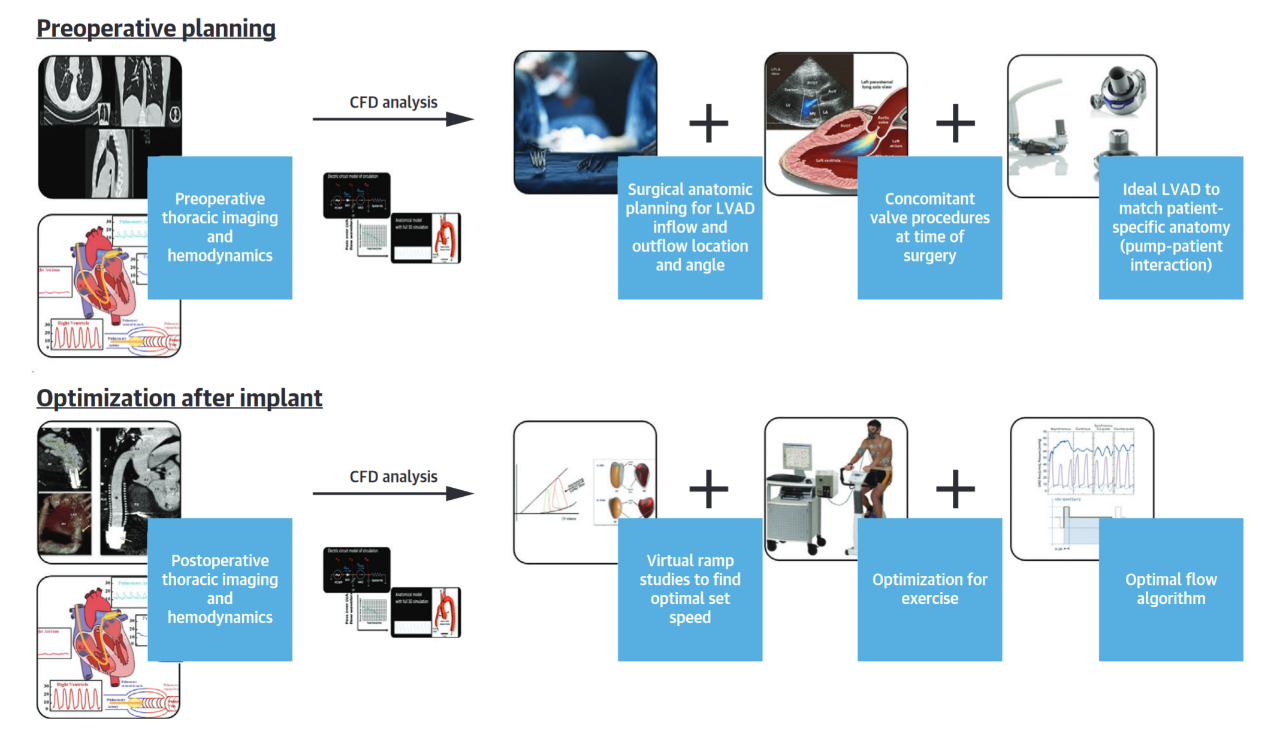
JACC: Adverse hemodynamic effects of left heart assist.Left heart assist (LVAD) is a life-saving treatment for patients with end-stage heart failure (HF), with two-year survival rates approaching those of heart transplantation. Patients receiving the newer-generation HeartMate 3 LVAD (HM3) implant have a higher five-year survival rate than HeartMate II LAVD (HMII) patients, and LVAD patients live longer with the machine. Pump thrombosis, stroke, and nonsurgical bleeding are recognized as hematocompatibility-related adverse events ( HRAEs), which have decreased with improvements in pump design, patient selection, and clinical management protocols. However, especially as patients survive longer with the device, sustained bleeding can make patients more susceptible to right-lateral heart failure ( right-lateral heart failure, RHF ) and aortic valve closure insufficiency ( aortic deficit, AI ).Considering the hemodynamic impact on AI and RHF, these comorbidities can be categorized as hemodynamic-related events ( HDREs ). Hemodynamic-driven events are time-dependent and tend to occur later than HRAEs.Strategies tailored to the hemodynamic environment based on patient-specific characteristics can mitigate these comorbidities and improve clinical outcomes.
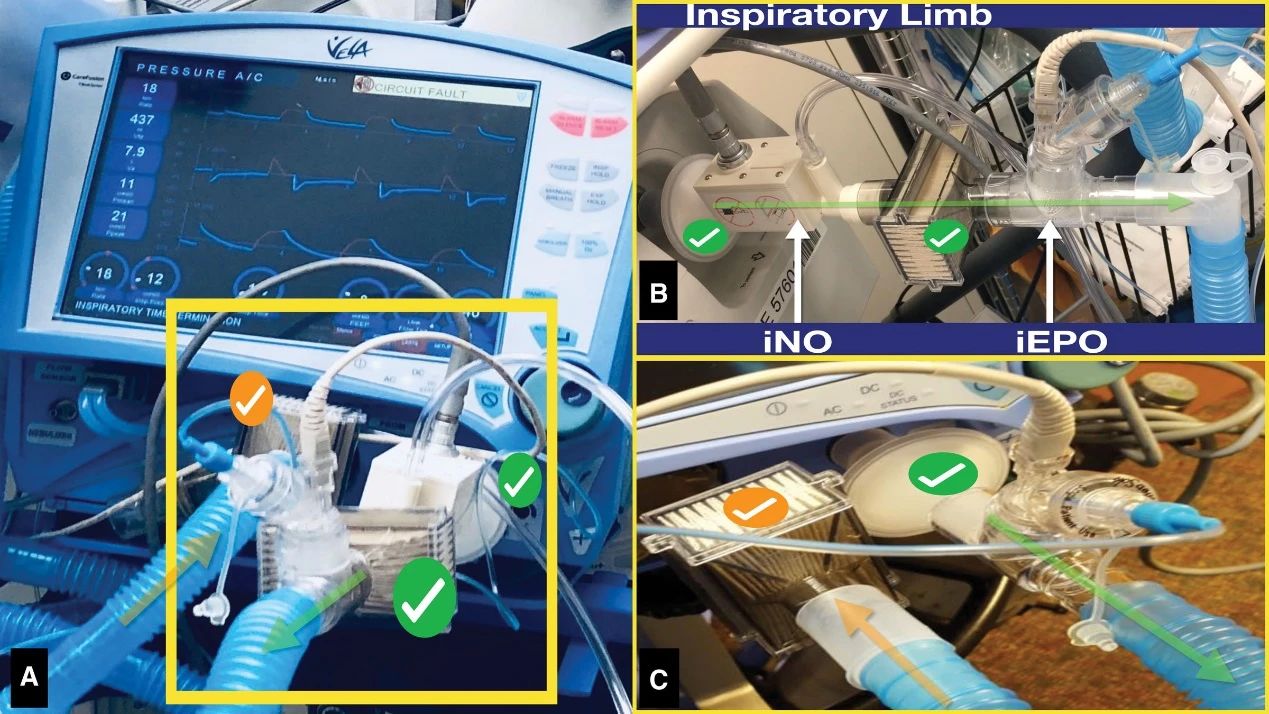
BACKGROUND: Right ventricular failure (RVF) is a major driver of morbidity and mortality after major cardiac surgery for advanced heart failure, including in situ heart transplantation and left ventricular assist device implantation. Inhaled pulmonary selective vasodilators, such as inhaled epoprostenol ( iEPO ) and nitric oxide ( iNO ), are important agents for the prevention and treatment of RVF after cardiac surgery. Despite the significant cost considerations of iNO therapy, evidence from clinical trials remains limited to guide drug selection. From an economic perspective, the pricing of iNO places significant financial pressure on patients, which has led to the increasing use of iEPO as a cost-saving alternative. METHODS: In this double-blind trial, participants were stratified according to surgical modality and key preoperative prognostic characteristics, and then randomized to receive either iEPO or iNO treatment starting at the end of extracorporeal circulation and continuing until admission to the intensive care unit. The primary outcome was the composite incidence of RVF after both procedures. Mechanical circulatory support was initiated according to the criteria of the Interagency Registry for Mechanically Assisted Circulatory Support after heart transplantation defined as isolated RVF and after left ventricular assist device implantation defined as moderate or severe right heart failure. An equivalence value of 15 percentage points for the difference in risk of RVF between the two groups was prespecified. Secondary outcomes assessed treatment differences and included: duration of mechanical ventilation; length of hospital stay and intensive care unit time during admission; occurrence of acute kidney injury and need for renal replacement therapy; and mortality at 30 days, 90 days, and 1 year after surgery. RESULTS: Of the 231 randomized participants eligible for enrollment at the time of surgery, 120 were treated with iEPO and 111 with iNO. 30 participants (25.0%) in the iEPO group and 25 participants (22.5%) in the iNO group experienced a primary outcome event, with a risk difference of 2.5 percentage points between the two groups (two one-sided 90% CIs, - 6.6% to 11.6%), supporting equivalence. The between-group differences for all postoperative secondary outcomes were not statistically significant. CONCLUSION: In patients with advanced heart failure treated with cardiac surgery, inhaled pulmonary selective vasodilator therapy with iEPO is associated with a similar risk of RVF and other postoperative secondary outcomes compared with iNO. CLINICAL IMPLICATIONS: High-level evidence supports the similarity between iEPO and iNO in the management of acute right ventricular failure and other outcomes after major cardiac surgery.
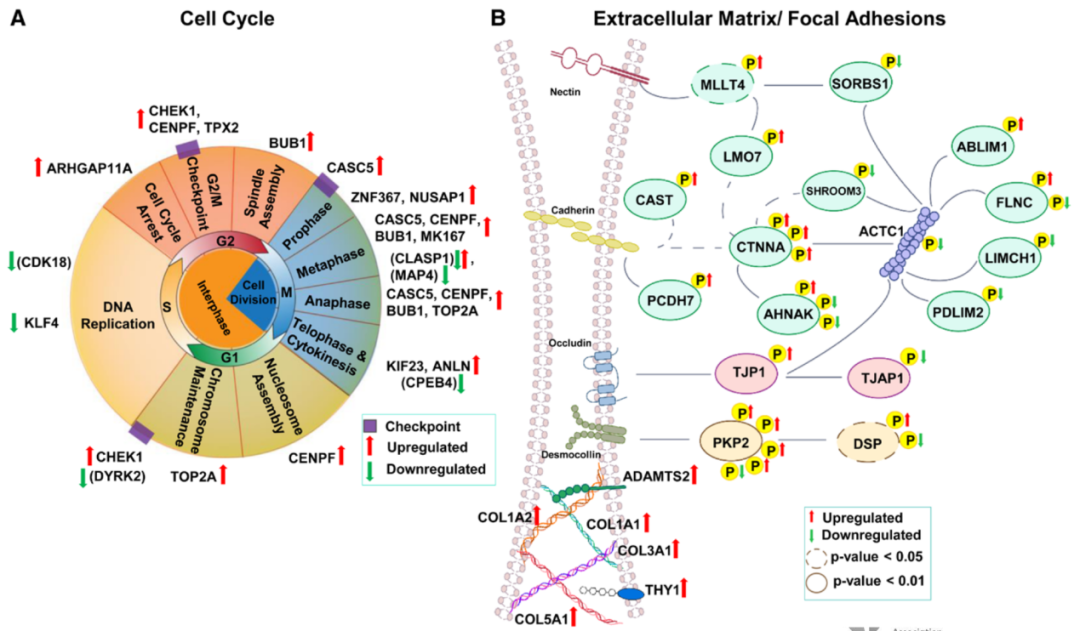
Circulation: transcriptomics- and proteomics-based determination of myocardial recovery potential after unloading of left ventricular assist and circulatory support devices.Left ventricular assist devices (LVADs) are now recognized as an important therapeutic tool for the treatment of patients with end-stage heart failure and as a temporary transition to heart transplantation. It is now known that restoration of cardiac function and reversal of cardiac structural remodeling can be observed in a subset of heart failure patients after LVAD withdrawal, and it has been demonstrated that LVAD implantation in combination with standard heart failure pharmacological therapy significantly improves cardiac structure and function, resulting in a high rate of LVAD withdrawal and favorable long-term outcomes. Although the underlying molecular mechanisms driving this recovery are largely unknown, this offers great promise for translational and clinical applications. The authors performed RNA transcriptome sequencing and phosphorylated protein analysis of left ventricular tissue from 93 patients with heart failure (HF) who underwent left ventricular assist device (LVAD) implantation and 12 nonfailing donor hearts. Patients were monitored prospectively by echocardiography to characterize their myocardial structure and function.The study detected 1341 transcripts and 288 phosphorylated peptides that were differentially regulated in cardiac tissues from control samples and HF patients. The study analyzed cardiac tissue with functional recovery after LVAD withdrawal (responders) versus unimproved tissue (non-responders) and detected 29 differentially expressed transcripts and 93 differentially expressed phosphopeptides. Further analysis revealed differential regulation in two key pathways: cell cycle regulation and extracellular matrix/adhesion junctions. This study is the first to comparatively analyze cardiac tissues from heart failure patients implanted with LVADs and non-failing donor patients by integrating a multi-omics platform including phosphoproteomics, transcriptome sequencing, and other technologies, expanding the understanding of the molecular basis of the relationship between normal and failing myocardial tissues, and revealing the key pathways that are deregulated during the onset of heart failure, as well as pathways that contribute to the myocardial functionality after unloading of mechanical circulatory support potential pathways for recovery. These findings may help guide patients to advanced HF therapies (undergoing heart transplantation or LVAD) and provide new targets for heart failure treatment.
Rapid development of domestic short- to medium-term ventricular assist
Domestic long-term ventricular assist is in a booming development stage, but the only two types of short- and medium-term ventricular assist applications in China are IABP and ECMO, with limited hemodynamic support in the former and potential problems such as increased cardiac afterload and complications in the latter. MoyoAssist®, a short- to medium-term external ventricular assist system developed by Prof. Dong Nianguo's team from the Department of Cardiac Surgery at Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, and HeartRock Medical, has obvious advantages in terms of time and flow rate of support, cardiac unloading, and blood compatibility, compared with IABP and ECMO. Short and medium-term extracorporeal ventricular assisted fully magnetically levitated blood pump, which can be used for heart failure, other high-risk critical illnesses that require temporary provision of cardiac pumping function, such as rescue and recovery of patients with low cardiac output who are unable to be removed from the extracorporeal circulation after cardiac surgery in fulminant myocarditis and cardiac surgery. The clinical trial of this technology was conducted by Professor Dong Nanguo of Wuhan Union Medical College Hospital as PI, with the participation of several clinical centers across China. The first subject has been enrolled since the end of June 2021, with full patient enrollment completed in early 2023, and current data show favorable clinical outcomes. The device can make a good complement with long-term ventricular assistance during the treatment process, meet the demand for short- and medium-term assistance for Chinese heart failure patients, and fill the current clinical gap.
Expert Profiles
Dong Nanguo
Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, China
Wang Yixuan
Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, China


