
With the advantages of less trauma, less bleeding, and faster postoperative recovery, EVAR has become the main treatment for AAA. With the increasing maturity of the technology, the indications for treatment have become broader. Although the perioperative risk of EVAR patients has been greatly reduced, the number of problems during the follow-up period is still high, requiring close follow-up and reoperation if necessary.On May 18, 2024, at the 2nd Tianfu Large Vessel Society Conference (TFS 2024), Prof. Jichun Zhao from West China Hospital of Sichuan University shared the data and results of the “EVAR Cohort Study” at West China Hospital of Sichuan University, and the results of the “EVAR Cohort Study” at West China Hospital of Sichuan University. Data and Complications of Endoluminal Treatment of Complex Abdominal Aortic Aneurysms”.

The Department of Vascular Surgery, West China Hospital, Sichuan University, is the main Engage Asia-Pacific enrollment unit, ranking 1st in Asia-Pacific for the number of cases enrolled in the early years (2011 to 2016), and more anatomically complex AAAs were included in the later years (2017 to 2021).Based on the Engage study model, a team of vascular surgeons from West China Hospital, Sichuan University, conducted the EVAR cohort study, enrolling patients between 2011 and 2021.
Inclusion criteria: 1) infrarenal abdominal aortic aneurysm; 2) abdominal aortic aneurysm with or without common iliac artery aneurysm; and 3) meeting the indications for surgical intervention.
Exclusion criteria: 1) abdominal aortic pseudoaneurysms or penetrating ulcers; 2) abdominal aortic intermural hematomas, abdominal aortic entrapment; 3) infected abdominal aortic aneurysms; 4) thoracic and abdominal aortic aneurysms as well as abdominal aortic aneurysms with renal arterial or other visceral arterial involvement; 5) patients with the use of the CERAB technique or Kissing's technique; 6) re-intervention after aneurysm surgery; and 7) lack of a preoperative abdominal aortic CT or those who were unable to obtain anatomical parameters.
Intervention Methdds: Uniform standardized surgical procedures were used for all patients; performed by a senior aortic endoluminal repair vascular surgeon; and intervention-related confounders were small.
Short-term outcome indicators: primary outcome indicator: 30-day mortality. Secondary outcome indicators: 30-day reintervention, 30-day aneurysm rupture, 30-day adverse cardiovascular events, and postoperative acute kidney injury
Long-term outcome metrics: primary outcome metric: 3-year reintervention rate. Secondary outcome indicators; 3-year adverse aortic events, 3-year overall survival, 3-year aortic-related deaths, etc.
1. Baseline data on patients
A total of 1,095 patients meeting the criteria were included, with a mean age of 71.14 ± 9.60 years, 83.01% male, 66.63% with combined hypertension, 12.8% with diabetes mellitus, 18.15% with pulmonary disease, 17.42% with coronary heart disease, and 5.35% with chronic kidney disease. The average neck length of AAA lesions in this cohort was 27 mm, the diameter was 20 mm, the neck was severely angular in 26.66% of cases, the average diameter of the tumor was 51.8 mm, the average diameter of the left common iliac artery was 15 mm, and the average diameter of the right common iliac artery was 16 mm.Compared with the Engage total cohort, the anatomy of the AAA necks in the present cohort was more complex, and the necks of the tumors were mainly twisted.
2. Short-term outcome
The 30-day mortality rate was 1.36% (15/1,095), and the main causes of death were postoperative abdominal hypertension syndrome after ruptured abdominal aortic aneurysm (27%), adverse cardiac events (27%), and pulmonary infection (20%).
3. Medium- and long-term survival outcomes
The mean follow-up was 49.1±32.0 months, and the median survival follow-up was 45.8 months.The survival rate from aortic-related events was 99.1% at 1 year, 98.3% at 3 years, and 95.8% at 5 years. The main causes of death were tumor (15.3%), heart attack (9.0%), stroke (9.0%), and pulmonary infection (8.6%). Aortic-related causes of death were unknown cause tumor rupture (n = 17), stent dissection (n = 1), stent infection (n = 2), type Ib endoleak (n = 4), and proximal aortic coarctation (n = 1).
4. Medium and long-term complications
The most common cause of reintervention was type Ib endoleak (28.4%), followed by type Ia endoleak (16.4%). Type I endoleaks associated with reintervention exceeded 60%. The incidence of stent infection is low, but management is very complex. Stent distal iliac artery aneurysm or internal iliac artery aneurysm formation, renal artery stenosis, and wound-related factors are also noteworthy.
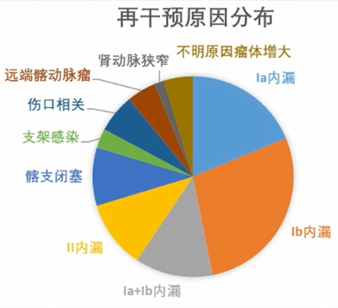
The median imaging follow-up time was 13.7 months. The incidence of freedom from type Ia endoleak was 98.7% at 1 year, 96.9% at 3 years, and 92.7% at 5 years postoperatively. The incidence of freedom from type Ib endoleak was 98.3% at 1 year, 94.7% at 3 years, and 88.1% at 5 years.The incidence of freedom from type II endoleak was 90.0% at 1 year, 77.2% at 3 years, and 68.7% at 5 years.The incidence of freedom from iliac branch occlusion was 97.1% at 1 year, 96.2% at 3 years, and 93.0% at 5 years.
Management of postoperative complications of EVAR
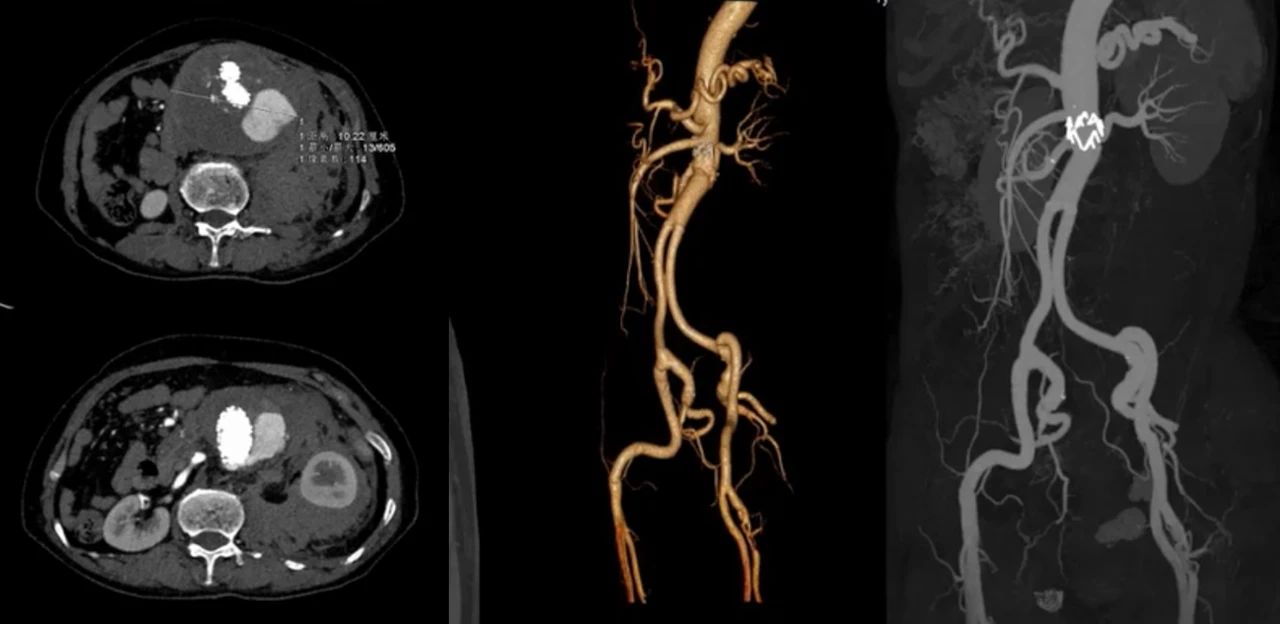
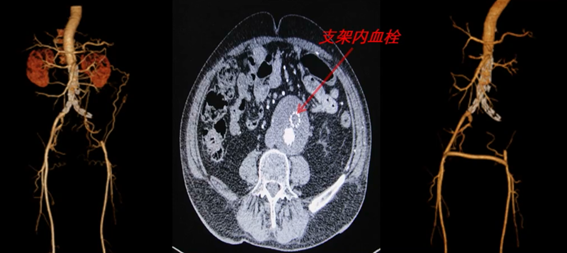
Complex abdominal aortic aneurysms include severe angulation, short necks, large aneurysms, combined access thrombus, combined iliac aneurysm, aneurysm rupture, stenosis, tortuosity, and occlusion of the access artery. Complex AAA has always been a challenge for endoluminal treatment and has a greater probability of postoperative complications.Common complications after EVAR include endoleak, iliac branch occlusion, stent migration, stent twisting, stent infection, and aneurysm rupture.
1. Treatment of internal leakage
The 2018 SVS guidelines recommend that type I endoleaks should be managed, type II endoleaks followed closely, type III endoleaks should be managed, and type IV endoleaks should be left untreated; surgery is recommended for patients who have failed endoluminal treatment for type I and II endoleaks who underwent tumor dilatation (1B).The 2019 ESVS AAA guidelines recommend prompt intervention for postoperative type I endoleaks after EVAR (1B).
If the type Ia endoleak disappears or the amount of endoleak does not increase and the tumor body does not increase in size, clinical observation can be continued. If the proximal type Ia endoleak and the tumor diameter increases compared with the surgery, balloon dilatation of the neck of the tumor and addition of a Cuff stent can be performed again, or spring coil embolization can be performed, and satisfactory results can be achieved. For type Ib endoleak, reoperation to lengthen the leg support is performed. For type II endoleak, spring coil embolization can be performed if the tumor grows progressively during the follow-up period.
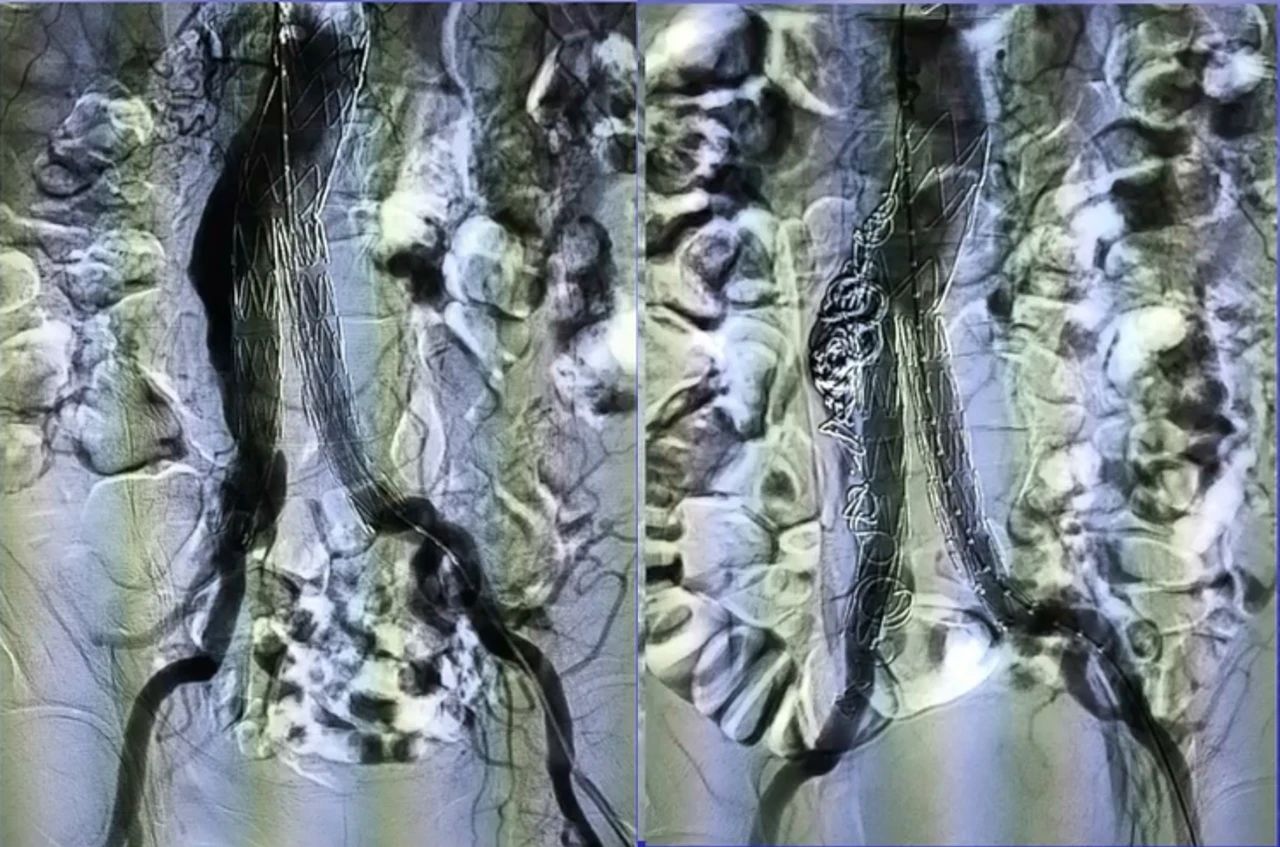
Case 1: 78-year-old man with proximal type Ia endoleak (proximal tumor neck dilatation) and right internal iliac artery traffic 3+ years after EVAR. The tumor lumen and right internal iliac artery were embolized with spring coils, and follow-up imaging showed significant improvement of the endoleak.
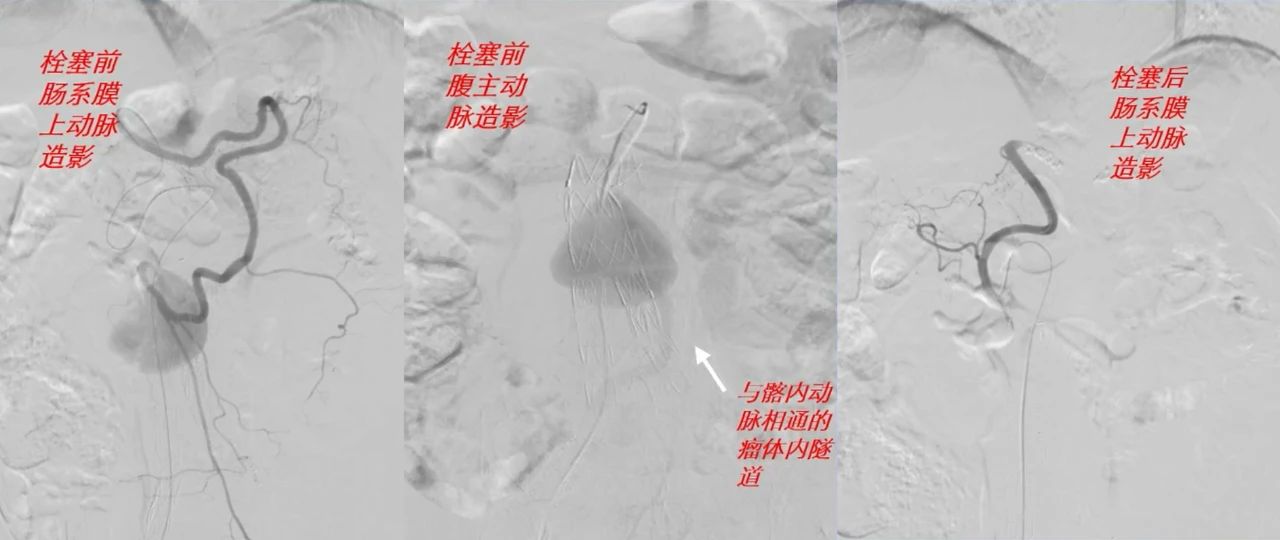
Case 2: A 77-year-old man, 66 months after EVAR, had a type II endoleak in the inferior mesenteric artery, which communicated distally with the embolized right internal iliac artery, and the aneurysm had increased 3 cm in size compared with the preoperative period. angiography showed that the type II endoleak communicated with the Riolan's arch formed by the superior mesenteric artery and then communicated with the right internal iliac artery. The Riolan's arch artery was embolized with a spring coil through the superior mesenteric artery, and the endoleak disappeared.
Case 3: 62-year-old woman, preoperatively diagnosed as EVAR postoperative type Ia endoleak with rupture, was operated openly, the tumor was resected, the stent was removed, and artificial vessel replacement was performed.
3. Management of acute iliac branch occlusion
Case 4: 70-year-old male with left iliac branch occlusion 1 year after EVAR. Bilateral femoral artery bypass surgery was performed.
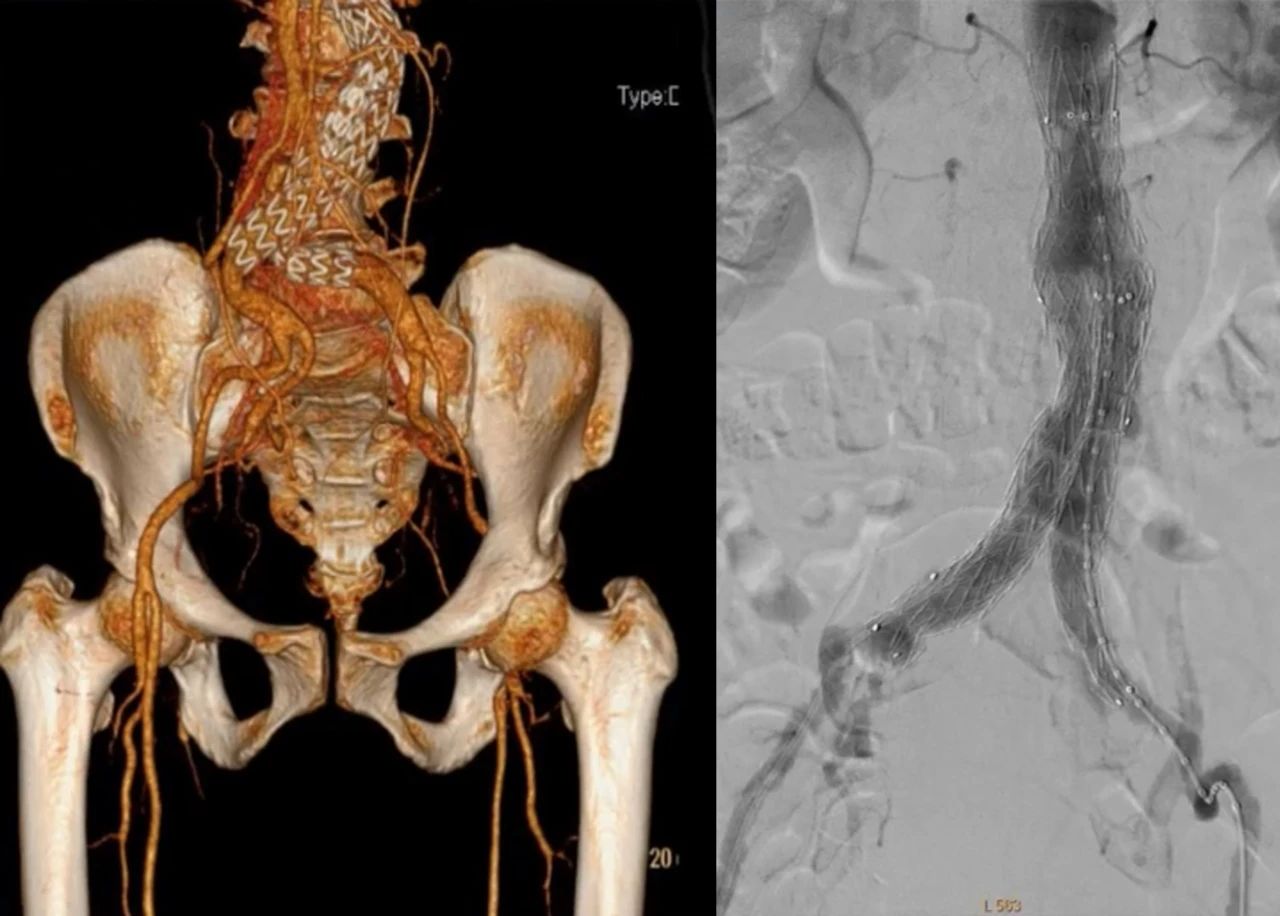
4. Management of graft infection after EVAR surgery

Summarize
Complex abdominal aortic aneurysm endoluminal repair requires detailed preoperative evaluation of EVAR surgical indications, aneurysm neck, aneurysm body, anatomical morphology of the iliac artery anchorage area, access artery, and precise intraoperative positioning. Postoperative close follow-up of the aneurysm diameter and endoleak changes, timely management of various complications during the follow-up period, the risk of rupture and graft infection require timely open surgical treatment to ensure the long-term results of EVAR treatment.


