
With the aging of the population, the incidence of aortic disease is increasing every year. The number of elderly, high-risk patients with aortic disease is likely to continue to increase in the future. Data from the National Hospital Quality Monitoring System (HQMS) suggests that the number of aortic surgeries is on the rise year after year, including both open and endoluminal minimally invasive surgeries.On May 18, 2024, Prof. Shu Chang of Fu Wai Hospital, Chinese Academy of Medical Sciences, shared advances in minimally invasive treatment of the aorta at the 2nd Tianfu Congress of the Great Vasculature (TFS 2024), a conference held in Beijing, China, on the theme of “Aortic Disease”.

In the early days, ascending aortic disease was off-limits to endoluminal surgery, and the main surgical approaches were open procedures such as ascending aortic replacement, Bentall's procedure, and David's procedure. However, with advances in minimally invasive techniques and instrumentation, endoluminal surgical repair has expanded to include the treatment of ascending aortic disease.
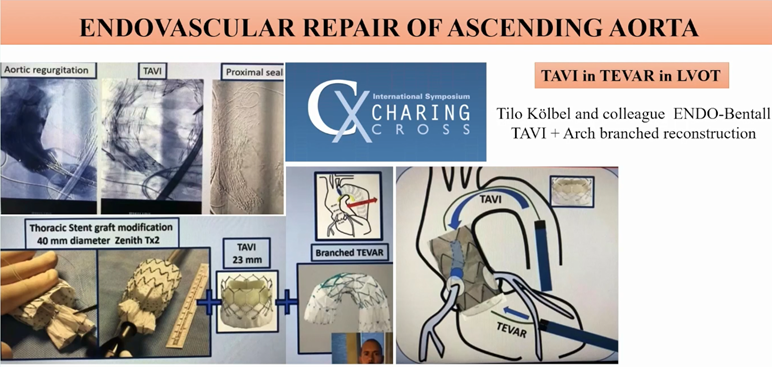
As early as 2001, Academician Wang Zhonghao performed the first ascending aortic stenting for the treatment of acute total aortic coarctation.In 2015, Prof. Shu Chang successfully performed his country's first ascending + descending aortic stenting in Indonesia.In 2017, Profs. Rylski and White proposed the Endo-Bentall/Endo-Wheat technique aimed at one-stage complete endoluminal repair of aortic root and ascending aortic lesions.In 2020, Prof. Gaia et al. performed the world's first Endo-Bentall procedure in a patient after aortic valve replacement with success.In 2023, Prof. Kölbel et al. demonstrated the Endo-Bentall TAVI + supra-arterial arch branching reconstruction procedure during the CX conference Demonstration.
Treatment Strategies for Aortic Arch Disease
The treatment of aortic arch disease needs to focus on the etiology, pathology and anatomical structure to develop individualized treatment strategies. Based on this, Prof. Shu proposed the “HENDO” treatment system, which includes Hybrid Arch Repair, Endovascular Repair and Open Arch Repair.
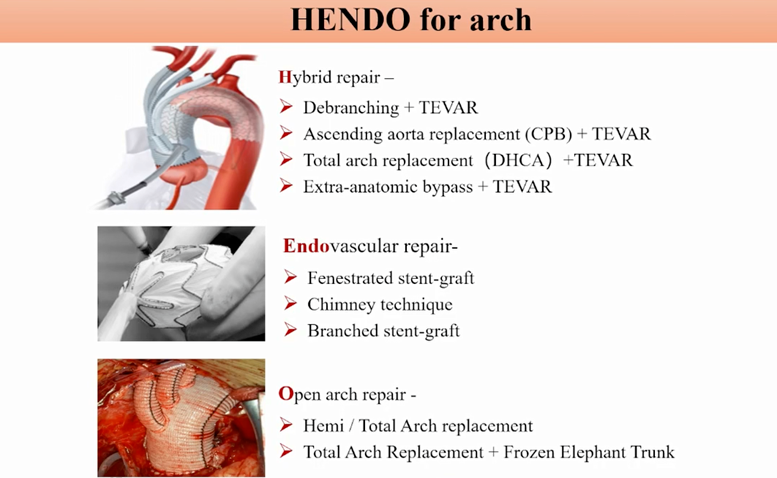
Open surgical procedures include half-arch replacement, full-arch replacement, and full-arch replacement + frozen elephant trunk stent. It should be noted that the aortic arch anatomy is reconstructed during the procedure, which requires deep hypothermia hypoperfusion (DHCA) and carries a high surgical risk.
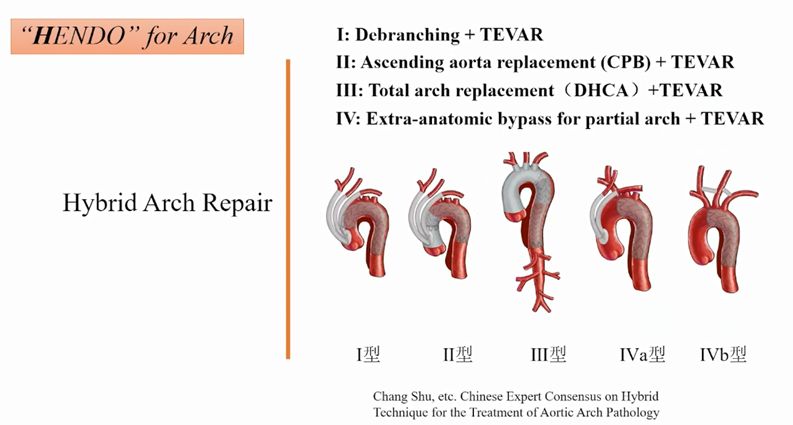
The aortic hybridization technique combines open surgical procedures with minimally invasive endoluminal repair techniques and is divided into 4 types:
(1) Hybrid type I is ascending aorta-head and brachial artery artificial vessel diversion combined with endoluminal repair of the aortic full-arch coated stent;
(2) Hybrid type II is an ascending aortic replacement (with or without treatment of the aortic root, CPB) with debranching of the cephalic and brachial vessels, combined with endoluminal repair of the aortic arch with a membranous stent;
(3) Hybrid type III is ascending aortic replacement (with or without treatment of the aortic root) and aortic arch replacement, with or without placement of a hard or soft elephant trunk, followed by evaluation or repair of the descending aorta and distal lesions that cannot be treated by conventional open surgery with the aid of a guidewire catheterization technique;
(4) Hybrid type IV is non-corporeal circulation, open thoracic artificial vascularization of one or both arteries of the ascending aorta-arch (type IVa) or open thoracic artificial vascularization of the neck (type IVb), combined with endoluminal repair of part of the aortic arch with a coated stent.
The development of endoluminal techniques and devices has advanced dramatically, with parallel stenting, open-window techniques, and branching stenting; newer devices include the Longuette™ stent, the CSkirt aortic arch partial-branch stenting system, and the Ankura™ stent, among others.
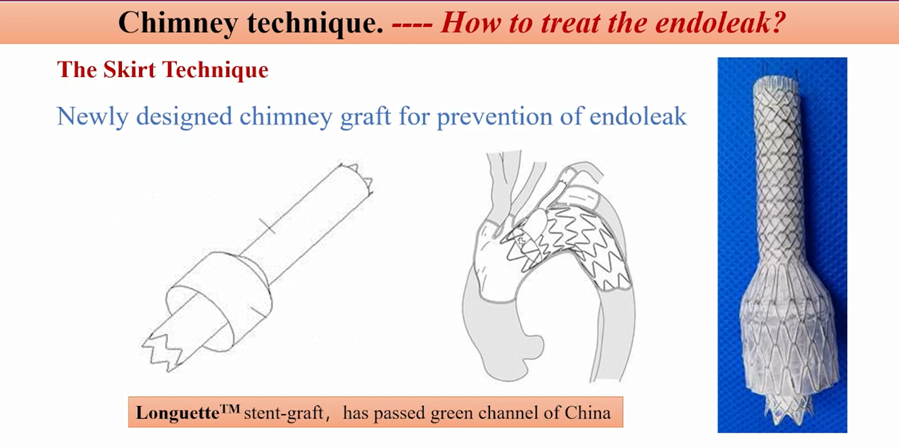
Parallel bracket technology (chimney technology, ch-TEVAR) can be used to single chimney technology, double chimney technology or triple chimney technology as required. It should be noted that it is recommended to choose a large bracket with good flexibility, which can easily be squeezed out of the gap by a small bracket, while a branch bracket needs to be chosen with strong support. In addition, the overlapping portion of parallel stents should be as adequate as possible to minimize endoleak. ch-TEVAR is simple to perform, with relatively controllable surgical risks and less restrictive surgical equipment, and is suitable for lesions with complex anatomy. Parallel stenting is also an option to remedy the situation when the supra-aortic arch branches are accidentally covered.
The ch-TEVAR may have Gutter endoleak due to its own technical limitations, and the incidence of type Ia endoleak is about 1.2% to 20%. The Longuette™ stent, which was developed by Prof. Shu Chang, is capable of preventing endoleaks. Currently, the results of the multi-center clinical trial of the Longuette™ stent indicate that the immediate technical success rate is 100%, the freedom from secondary intervention rate is 97.88%, and the incidence of type I/III endoleaks during follow-up is only 1.4% (2/142).
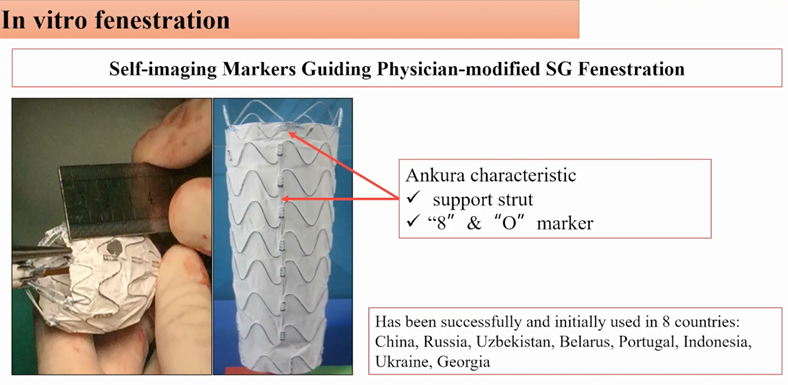
The windowing technique is categorized into extracorporeal preopening and in situ windowing techniques, which are selected according to the angle of the branch vessels, and sometimes combined with extracorporeal preopening and in situ windowing techniques to complete the surgery. This technique can maintain the original anatomical structure of the supra-arch branch vessels, conform to the morphology of the aortic arch, reduce the incidence of endoleak, and shorten the operation time. Prof. Shu Chang's team innovatively proposed to utilize the X-ray impermeable markings of the stent itself to guide the opening and positioning of the branch arteries - the stent self-expression positioning method of extracorporeal aortic windowing technique, and the stent used is the Ankura aortic stent. The Ankura aortic stent is used for this purpose. It has its own “8” and “O” marking points and reinforcement bars, and it takes only 5 minutes to complete the windowing operation. The Ankura stent is a fast and easy-to-use technique that can be used to reconstruct all three branches of the arch from a single puncture point in the femoral artery, and can be used for single-branch reconstruction in 30 min, double-branch reconstruction in 1 h, and triple-branch reconstruction in 1.5 h. The Ankura stent has been successfully used in more than 10 countries.
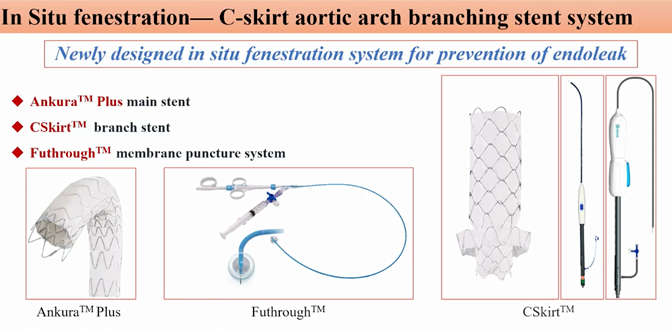
The Ankura™ Plus stent has a sparse stent beam in the windowing area of the arch laminating segment, which facilitates windowing, and in combination with the CSkirt™ stent, which has a “petticoat”, the prevention of endoleak can be better realized. In addition, the combination of the Futhrough™ System allows for smooth in situ puncture and precise window opening.
The branch stent conforms to the vascular anatomy and avoids the problems of gutter endoleak or stent displacement, which can effectively solve the aortic arch lesions.Castor® Branch Coated Stent is the first one-piece branch reconstruction stent for the aortic arch in China, which can complete the reconstruction of the left subclavian artery in one phase during the TEVAR procedure. In addition, Castor® combined with parallel stenting technology can realize LCCA and LSA reconstruction at the same time. Meanwhile, the WeFlow series of aortic arch branching stents developed by Prof. Guo Wei's team is able to realize single, double and triple branching of the arch in a fully endoluminal reconstruction, and the preliminary clinical results have shown good efficacy.
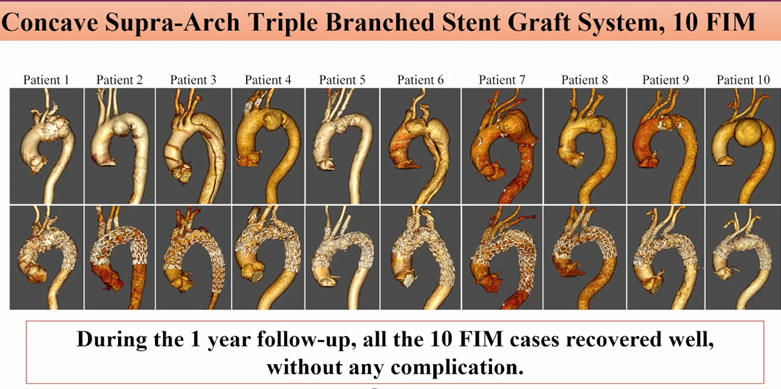
The FIM study of the new aortic stent developed under the leadership of Prof. Shu has completed 10 procedures with a short procedure time, less intraoperative bleeding, and satisfactory results in terms of immediate efficacy and during the follow-up period (1 to 2 years) without serious complications.
Treatment Strategies for Descending Aortic Disease
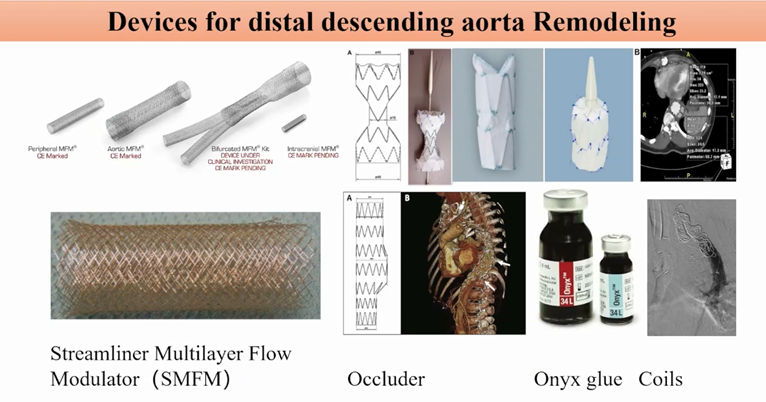
Treatment of descending aortic disease requires attention to distal aortic remodeling. Currently, TEVAR in the distal descending aorta still has challenges such as distal residual rupture triggering aneurysmal dilatation, failure of distal true lumen stenosis to resolve, and new entrapment rupture (SINE) distal to the laminated stent. To address these challenges, clinicians have made many attempts, such as distal use of multilayered bare stents, use of blockers, gel-fill, and spring-coil embolization.
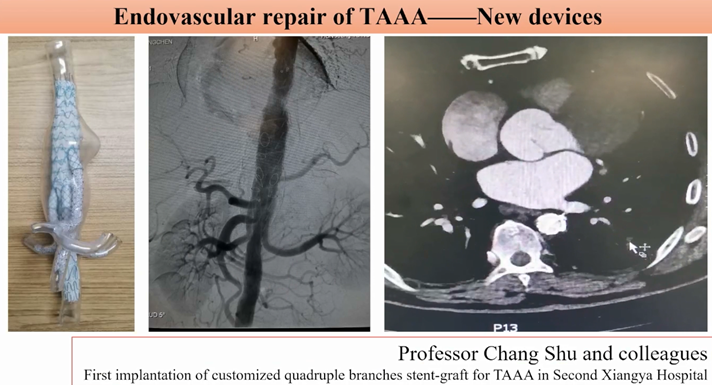
For total endoluminal repair of thoracoabdominal aortic aneurysms, clinicians are also actively developing new products, and many new products are in clinical trials. In China, the G-Branch™ Thoracoabdominal Aortic Coated Stent System developed by Prof. Guo Wei's team has completed the FIM study, which has initially verified its clinical feasibility; a multi-center clinical study is underway, and the preliminary results suggest that it can achieve good clinical efficacy. The customized four-branch thoracoabdominal aortic stent designed by Prof. Shu Chang's team has successfully completed its first clinical application at Xiangya II Hospital, and the case has been followed up for 2 years and still maintains good efficacy.
Strategies for the treatment of abdominal aortic disease
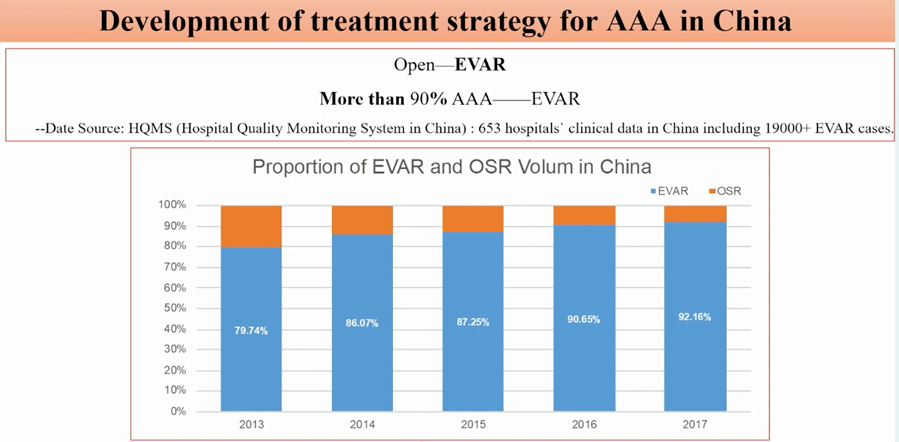
HQMS data suggests that as of 2016, the proportion of endoluminal treatment for AAA patients in China has exceeded 90%, including many patients with anatomically complex AAA (cAAA). Extreme flat kidney release, extracorporeal windowing technique, use of CUFF stent, chimney technique, and development and application of new stents are all endoluminal attempts made by clinicians to overcome cAAA. However, with the development of endoluminal surgery and follow-up time, clinicians have found that endoluminal surgery cannot solve all cAAA, and open surgery is still its basic treatment.
Summarize
The treatment of aortic disease is gradually transitioning from open surgery to hybridization and endoluminal repair. Minimally invasive treatments are the trend of the future. Surgical open surgery is still the basis for the treatment of aortic diseases, and subtle and precise surgery under direct vision is still the gold standard for the treatment of complex lesions. The anatomical and pathological features of aortic disease are diverse, and a precise individualized treatment plan should be chosen according to the specific lesion. The decision to branch reconstruction should be made cautiously, and branch reconstruction should be performed only when necessary. Many new non-customized single-, double-, and triple-branch stent systems are still in the developmental stage, and more safety and efficacy data are expected.


