VEITH 2023 | Vikram S. Kashyap: Do pre-expansion, post-expansion during TCAR therapy increase adverse events
时间: 2024-03-22
作者: 小编:
阅读量: 232
关键词:

Extracranial carotid artery stenosis is a major cause of atherosclerotic stroke. Transfemoral carotid artery stenting (TF-CAS) is an important therapeutic procedure for carotid artery stenosis. The balloon dilatation strategies during its treatment are preexpansion only (PRE), postexpansion only (POST), and preexpansion + postexpansion (PRE + POST). Concerns have been raised about higher neurological risk and hemodynamic instability associated with POST and PRE + POST during TF-CAS. Studies have shown that post dilatation for TF-CAS increases the risk of stroke by 2.4-fold and increases the risk of hemodynamic instability by 3.8-fold, which can lead to increased myocardial infarction (MI), LOS, and mortality. Transcarotid artery revascularization (TCAR) bypasses the manipulation of the device through the aortic arch and across the diseased segment, providing better embolic protection. Whether performing balloon dilatation during TCAR also results in the above adverse events is not yet known.At the recent 50th International Congress on Vascular and Endoluminal Vascularization (VEITH 2023), Professor Vikram S. Kashyap from the Cleveland Medical Center analyzed the results of performing PRE or POST or PRE+POST balloon dilation strategies during TCAR.

Research methodology
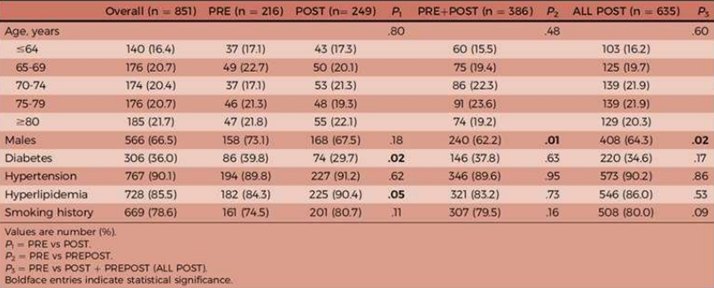
Data from the ROADSTER 1 and ROADSTER 2 trials and the ROADSTER Extended Access TCAR trial were collected prospectively. All patients had anatomic or clinical factors at high risk for carotid endarterectomy (CEA), asymptomatic carotid stenosis of >80%, and symptomatic carotid stenosis of >50%. The primary outcome indicators were stroke, death, and MI at 30 days postoperatively. data were statistically analyzed using χ2, analysis of variance, and multivariate analysis. After screening, 851 patients who met the criteria were finally included.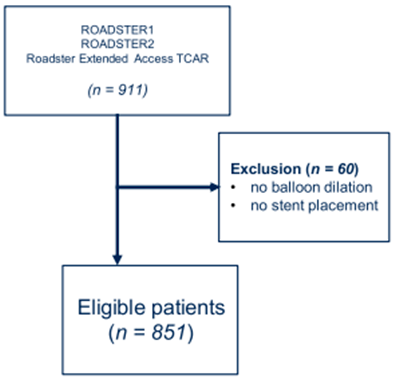
Findings
A total of 851 patients were included, with 66.5% male patients. In the full cohort, the proportion of combined hypertension was 90.1%, hyperlipidemia 85.5%, and diabetes mellitus 36.0%; carotid stenosis was >70% in 97% (n = 828) of the patients and >90% in 41% (n = 348) of the patients.216 patients were enrolled in the PRE group, 249 patients in the POST group, and 386 patients in the PRE + POST group. In contrast, fewer patients had stenosis >90% in the POST group, but there was no significant difference. the proportion of patients with previous ipsilateral stroke was significantly higher in the PRE group (PRE 22.2%, POST 10.8%, PRE + POST 14%, p = 0.002).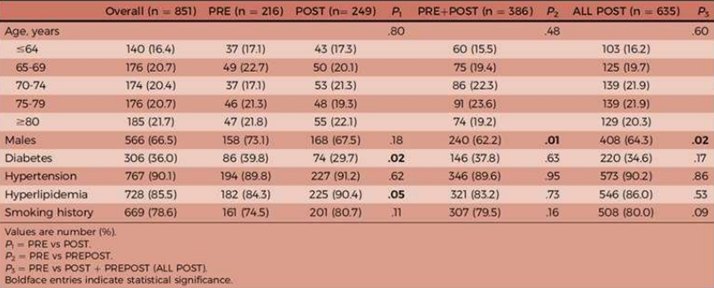
2. Surgical characteristics
The PRE + POST group had a significantly higher proportion of patients receiving general anesthesia and a longer mean time to flow reversal, as well as an additional 4 to 5 min of operative time (skin-to-skin). This was due to additional angioplasty maneuvers. In addition, the size of the balloon used was significantly larger in the PRE group compared with the PRE + POST group (4.3 ± 0.75 mm vs. 3.6 ± 0.73 mm, P < 0.001); whereas there was no significant difference in the postexpansion balloon (5.1 ± 0.81 mm vs. 5.0 ± 0.49 mm, P = 0.37).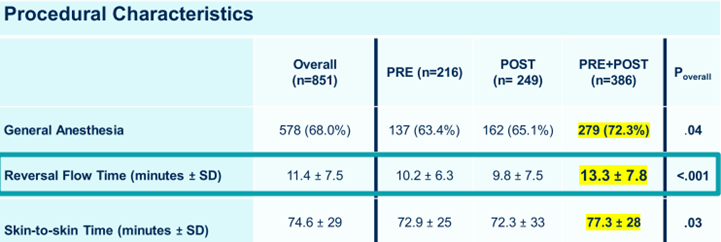
3. 30-day postoperative outcomes
In the full cohort, the 30-day postoperative stroke rate was 1.9%, the mortality rate was 0.5%, and the MI rate was 0.94%. Comparing the primary outcomes in the PRE, POST, and PRE+POST groups, there were no statistically significant differences between the groups in the incidence of stroke, death, MI, and stroke/death/MI.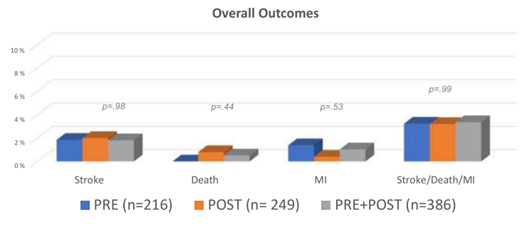
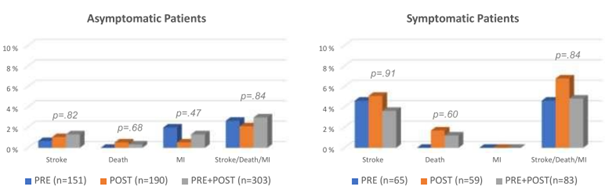
Asymptomatic patients had lower 30-day postoperative stroke rates (1.1%) and mortality rates (0.3%) and higher MI rates. Comparing the primary outcomes in the PRE, POST, and PRE+POST groups, there were no statistically significant differences between the groups in the incidence of stroke, death, MI, and stroke/death/MI in either symptomatic or asymptomatic patients.
summarize
Based on these prospective trial data, there was no difference in neurologic complications resulting from balloon dilation strategies during TCAR. Therefore, avoidance of POST during TCAR may be unnecessary, contrary to the results of TF-CAS. As to whether POST improves stent durability/reduces restenosis, and reduces reintervention remains unclear.
Reprinted from Outpatient Magazine