
Adventitial Cystic Disease (ACD) is a rare disease.In 1947, Atkins et al. first described a case of adventitial cyst involving the right external iliac artery. To date, there have been about 600 reports covering about 800 patients, with over 80% of lesions involving the popliteal artery. At the recent 50th International Vascular and Endoluminal Vascular Congress (VEITH 2023), Prof. Irwin V Mohan from the University of Sydney, Australia, shared the management of popliteal artery epiphyseal cyst disease.

ACD pathogenesis
Trauma theory: chronic degenerative lesions caused by repetitive trauma.
Ganglion theory: synovial cyst enlarges and spreads along vascular branches, eventually entering the periphery of neighboring great vessels.
Systemic disease theory: degeneration of the tunica albuginea and cyst formation are part of systemic connective tissue diseases.
Developmental theory: During the embryonic period, mucin-secreting mesenchymal stromal cells from nearby joints are located in the vascular epithelium, and the secretion of mucin leads to the formation of cysts.
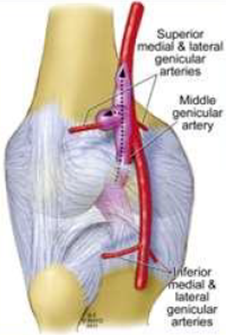
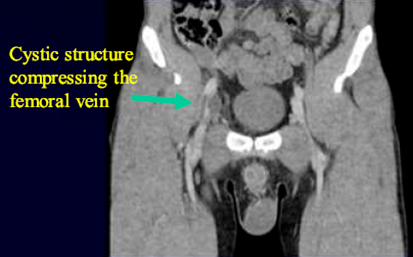
The typical symptom in cases of ACD involving the popliteal artery is claudication, which usually occurs briefly or suddenly or after a single episode of exertion. In contrast to claudication due to ischemia of the lower extremities caused by atherosclerosis, this symptom may disappear completely for a period of time, but it will soon reappear or deteriorate rapidly; and it takes longer to recover from the pain of this symptom. It may also manifest as below-knee pain due to pressure. Venous ACD lesions can lead to swelling of the limb (due to partial/complete occlusion). When veins are completely occluded, patients may develop deep vein thrombosis (Figure 2). Clinically, ACD is difficult to diagnose and needs to be differentiated from popliteal vascular entrapment syndrome, popliteal cysts, entrapment aneurysms, and popliteal artery embolism, taking into account the age of the patient, the location of the lesion, and the medical history. Venous ACD, on the other hand, is easily diagnosed as deep vein thrombosis because patients usually present with leg swelling.
ACD imaging
1. Ultrasound
CAD is seen in the wall of the diseased vessel as a pike-shaped or elongated cystic echogenic area with homogeneous and consistent signal, traveling along the wall of the vessel and presenting as a simple fluid-like pattern, which is often misdiagnosed as an aneurysm.

2. IVUS examination

3. CTA examination
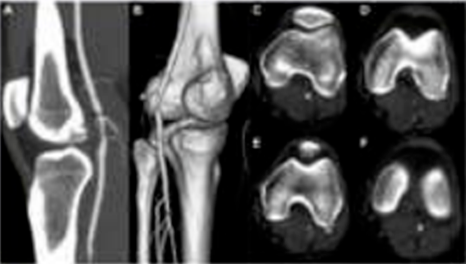
4. MRI/MRA examination


Management of ACD
Surgical treatment of ACD includes percutaneous aspiration, endoluminal intervention, and surgical resection + reconstructive surgery. Percutaneous aspiration may fail due to incomplete aspiration and has a high recurrence rate. In contrast, endoluminal intervention is performed by stenting to overcome cyst compression and maintain arterial lumen. However, this procedure lacks long-term data on transcatheter stenting in young patients. In addition, studies have shown that percutaneous intervention (aspiration or angioplasty) is a risk factor for cyst recurrence (P < 0.001). Currently, open cystectomy + arterial reconstruction is the optimal surgical management of ACD.


