
Popliteal artery aneurysm (PAA) is the most common peripheral artery aneurysm, with a mean patient age of 71 years. It is significantly more prevalent in men than in women, often involves both sides, and is most often associated with abdominal aortic aneurysms (AAA).2021 SVS guidelines for the management of popliteal aneurysms recommend that patients with PAA undergo screening for contralateral PAA and AAA (1B). If left untreated, PAA can lead to embolization/thrombosis, distal outflow tract embolization, limb ischemia, rupture, and even amputation. At the recent 50th International Vascular and Endoluminal Vascular Congress (VEITH 2023), Prof. Fred A Weaver from the University of Southern California, USA, shared an update on popliteal artery aneurysm management strategies and differences in treatment strategies for female patients.
PAA Natural History
In 2022, Beuschel et al [1] summarized the natural history of PAA disease, suggesting a high incidence of thromboembolic and amputation complications in PAA, which occurred at a mean time of 18 months. At 5 years of follow-up, about 50% of patients had complications.
Indications for urgent PAA repair include thrombosis or rupture; indications for elective repair include, PAA diameter >2 cm, appendage thrombus, evidence of distal embolization, and chronic thrombosis associated with CLI.2021 The SVS Guidelines for the Management of Popliteal Artery Aneurysms recommend repair in asymptomatic patients with PAA diameters >20 mm to reduce the risk of thromboembolic complications and limb loss (1B).
Elective popliteal artery aneurysm repair includes open surgery and endoluminal repair surgery, where open surgery includes medial open access (bypass + ligation of the PAA), and posterior open access (graft replacement); endoluminal repair is stent-graft implantation to isolate the aneurysm.
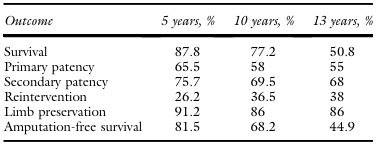
The 33-year experience of open surgical treatment of PAA shared by Dorigo et al [2] focused on early and long-term postoperative outcomes. A total of 196 patients with PAA were included in this study and 234 open interventions were performed. At 5 years postoperatively, the patient survival, phase I patency, reintervention, and limb preservation rates were 87.8%, 65.5%, 26.2%, and 91.2%, respectively; at 10 years postoperatively, 77.2%, 58%, 36.5%, and 86%, respectively; and at 13 years postoperatively, 50.8%, 55%, 38%, and 86%, respectively (Table 1). Moreover, the cumulative perioperative mortality rate was 1%, the thrombosis rate was 7.7%, and the cumulative amputation rate was 3.8%. Thus, it can be seen that open surgery for PAA can achieve good long-term efficacy.
Table 1.Main forward results
In 2016, Phair et al [3] retrospectively analyzed the efficacy of medial and posterior open approaches. The results showed that the posterior access group had a superior performance in terms of distant phase I (P = 0.02), phase II patency rate, aneurysm isolation, and need for reintervention.
Open vs. endoluminal treatment strategy
In 2014, Huang et al [4] compared the efficacy of endoluminal PAA repair and open surgery, enrolling 120 patients with 149 PAA lesions. Forty-two limbs of 35 patients (all male) underwent endoluminal repair with a technical success rate of 98%. 107 limbs of 91 patients (90 male) underwent open surgery. Comparison showed that the 30-day MAE rates were comparable between the endoluminal repair and open surgery groups. In contrast, there was a tendency for endoluminal prosthetics to reduce the incidence of MAE in elective interventions, but there was no statistical difference (Fig. 1). It is reasonable to perform endoluminal repair in older and high-risk patients with appropriate anatomy.
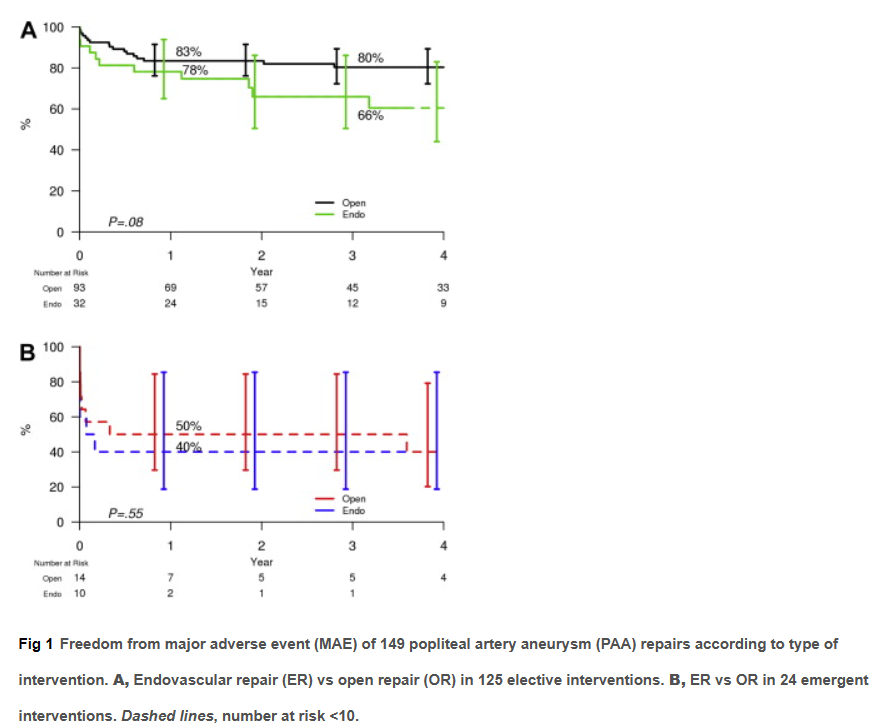
Figure 1.Comparison of major adverse events in endoluminal and open restorative surgery
In 2017, Leake et al [5] retrospectively compared and analyzed the efficacy of open and endoluminal repair for popliteal artery aneurysms. A total of 14 studies covering 4,880 patients with PAA were included in this study, comprising 3,915 open and 1,210 endoluminal. Compared to the endoluminal patients, the open surgery patients were younger and had poorer below-knee outflow tracts. Postoperatively, the open surgery patient group had a higher rate of wound complications and a longer hospital stay, but thrombosis occurred less frequently and there were fewer reinterventions. Compared with endoluminal surgery, open surgery had higher rates of one-stage patency at 1 year (88.3% vs. 81.2%) and 3 years (79.4% vs. 68.2%), but there was no difference in second-stage patency or amputation rates.
The 2021 SVS guidelines for the management of popliteal artery aneurysms recommend open repair in asymptomatic patients with a life expectancy of >5 years and adequate saphenous veins. For patients with a shortened life expectancy who require surgical intervention, endoluminal repair is recommended (2C).
By analyzing the data of 1,509 patients, Ravn et al [6] found that the symptoms of PAA were similar in females and males, but females had less bilateral involvement, and their symptomatic PAA was usually less than 2 cm in diameter.Despite the fact that life expectancy is generally longer in females, the survival of female patients with PAA is the same as that of males.
Peeran et al [7] compared the surgical outcomes of female and male patients with PAA. A total of 485 female patients were included in this study and only 8 (1.6%) underwent surgery for having degenerative PAA. This shows that the percentage of patients with surgical intervention is relatively low among female patients. Long-term mortality was higher in female patients requiring PAA repair compared to male patients with similar cases and treatment strategies (Figure 2).
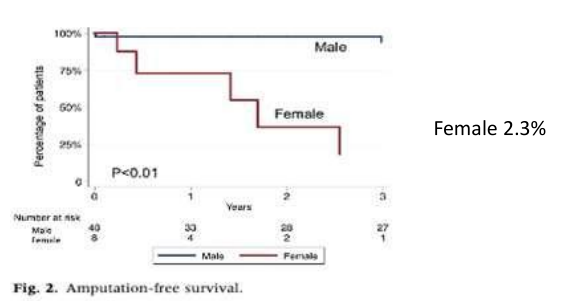
Figure 2. significantly lower survival from amputation in female patients
Naazie et al [8] analyzed 3,807 patients with PAA and only 160 females (4.2%). The comparison shows that female patients were younger and had a significantly higher percentage of symptomatic PAA. At 1 year postoperatively, there was no difference between the two groups in terms of phase I patency and overall survival; however, female patients were significantly lower than males in terms of amputation rates (Table 2).
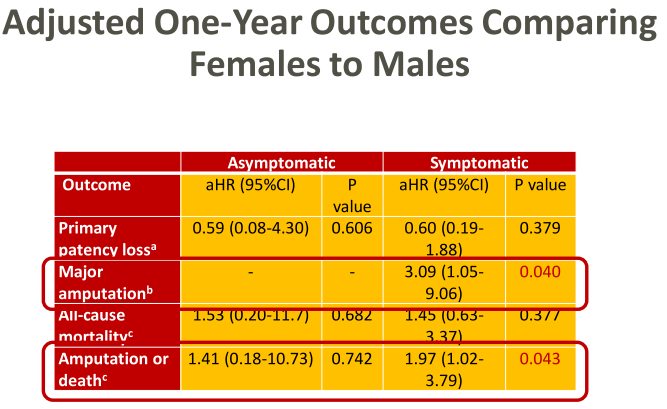
However, for symptomatic PAA, female patients have 3 times the risk of a 1-year major amputation and 2 times the combined risk of major amputation or death (Figure 3). Thus, early identification and treatment of PAA before it becomes symptomatic can optimize limb preservation outcomes in female patients with PAA.
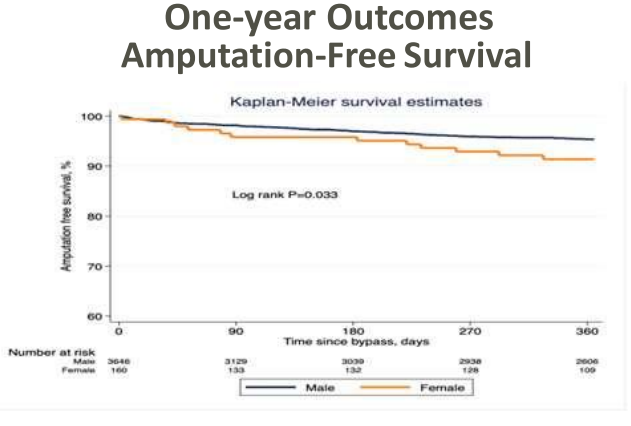
Figure 3. 1-year post-operative survival from amputation
summarize
For patients with PAA, open repair surgery with a posterior lateral open approach is advantageous. Endoluminal surgery is indicated for patients with localized lesions and 2 to 3 outflow tracts. In the treatment of women with PAA, considering the increased acuity of smaller diameters, the question of "whether invasive treatment should be performed at smaller size thresholds" is still worthy of consideration.
参考文献


