
The main cause of early angioplasty failure elastic retraction and obtaining a lumen with infinite flow entrapment and adequate diameter is the ultimate quest of balloon angioplasty. However, targeting lesions with a high calcific load often requires a higher pressure and size of balloon for dilatation, but this leads to more intense elastic retraction and more severe entrapment. Studies have shown that 97% of below-the-knee (BTK) lesions experience >10% elastic retraction 15 min after POBA. At the 50th International Congress on Vascular and Endoluminal Vasculature (VEITH 2023), November 14-18, US local time, Prof. Francesco Liistro from the San Donato Hospital in Arezzo, Italy, presented the strategy of endovascular lithotripsy balloon (IVL) in combination with DCB therapy and compared the Difference in efficacy.

Prof. Francesco Liistro
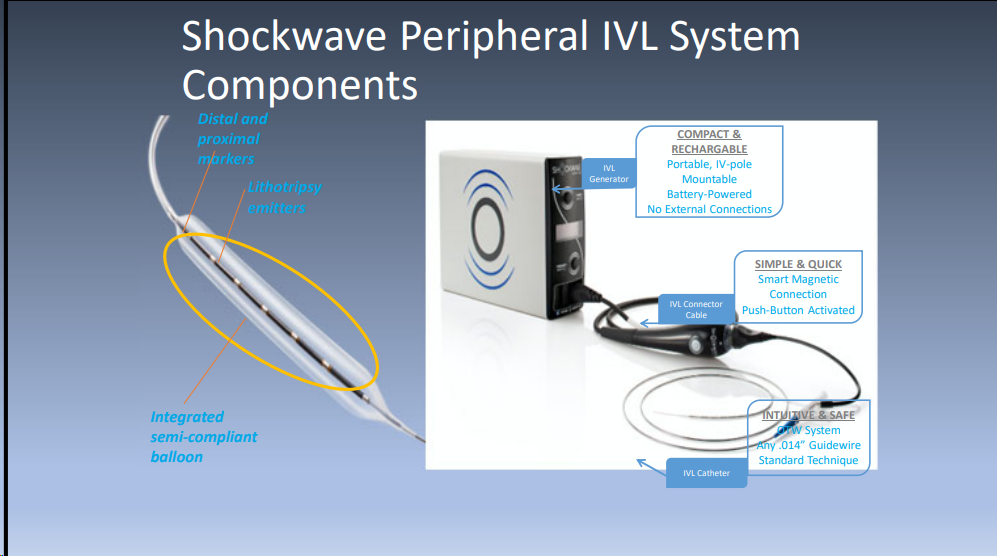
Advantages of peripheral IVL
The principle of IVL is that the energy generated by the energy generator in the shockwave balloon is applied to endothelial and intima-media calcified lesions; the shockwave energy is highly tissue specific and does not damage the endothelium or soft tissues while effectively breaking up the calcification. In addition, IVL results in complete vasodilation with reduced direct elastic recoil, no distal particle embolization, and can be used for subendothelial recanalization, as well as for BTA arteries. It is also unique in that the shock wave breaks up the calcified plaque without damaging the endothelium, and then the drug balloon is used, which allows the drug to penetrate easily through the gap and prevents intimal hyperplasia due to endothelial damage.
DEBATE-BTK SHOCK Study
The DEBATE-BTK SHOCK study was a single-center randomized preliminary feasibility study designed to assess the feasibility and efficacy of IVL in combination with DCB for the treatment of BTK lesions in patients with CLTI, and to evaluate the efficiency of drug application for calcified lesions after IVL treatment. The study was a sub-study of the DEBATE-BTK DUELL study, which included a total of 80 patients randomized 1:1 to the IVL + DCB group (n = 40) and the DCB alone group (n = 40), who were treated with aspirin + clopidogrel postoperatively for 3 months of pharmacological therapy, with the primary endpoint of 6-month distant lumen loss (LLL).
Inclusion criteria: grade RC 4, 5, and 6; stenosis/occlusion >40 mm; presence of distal outflow tracts; patency of popliteal artery (P3) segments; unlimited flow entrapment. Exclusion criteria: paclitaxel allergy; contraindication to combined antiplatelet therapy; life expectancy <1 year; no consent; need for BTA angioplasty.
Preliminary results of the DEBATE-BTK SHOCK Study
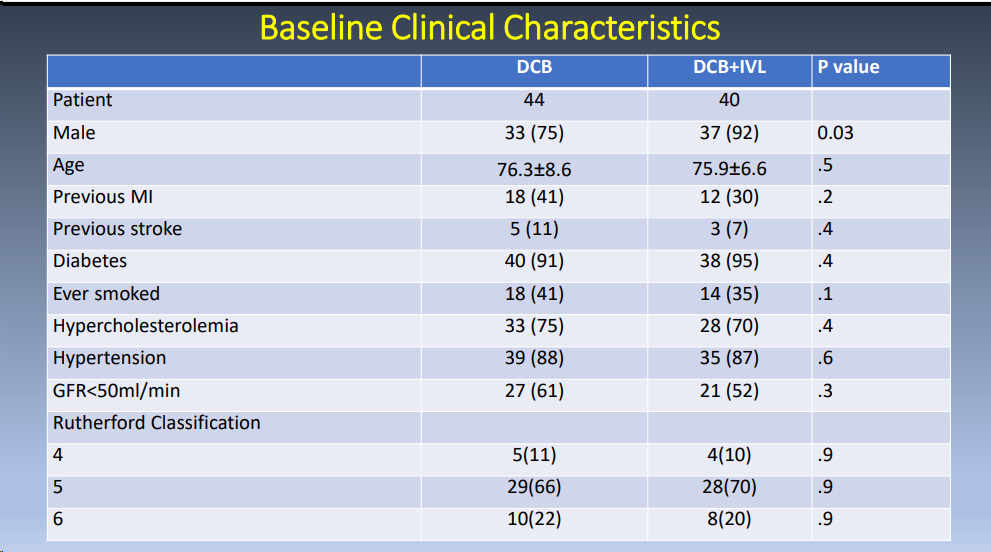
A total of 88 patients, 44 in the DCB group and 40 in the DCB + IVL group, were finally included. Comparing the baseline demographic characteristics of the two groups, there were no statistically significant differences in age, previous MI, stroke, diabetes mellitus, hypertension, hyperlipidemia, and other comorbidities, except that the proportion of male patients was significantly higher in the DCB + IVL group than in the DCB group (92% vs. 75%, P = 0.03).
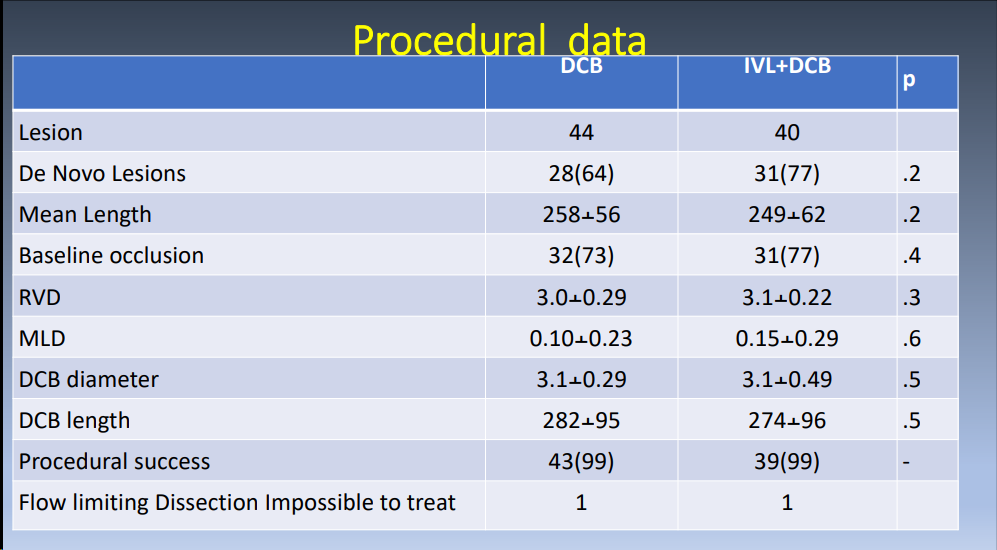
Surgical information: the RVD and MLD were 3.0±0.29 mm and 0.1±0.23 mm in the DCB group and 3.1±0.22 mm and 0.15±0.29 mm in the DCB + IVL group, respectively. the diameters of the DCBs used were 3.1±0.29 mm and 3.1±0.49 mm in the two groups, respectively. the surgical success rate was 99% in both groups.
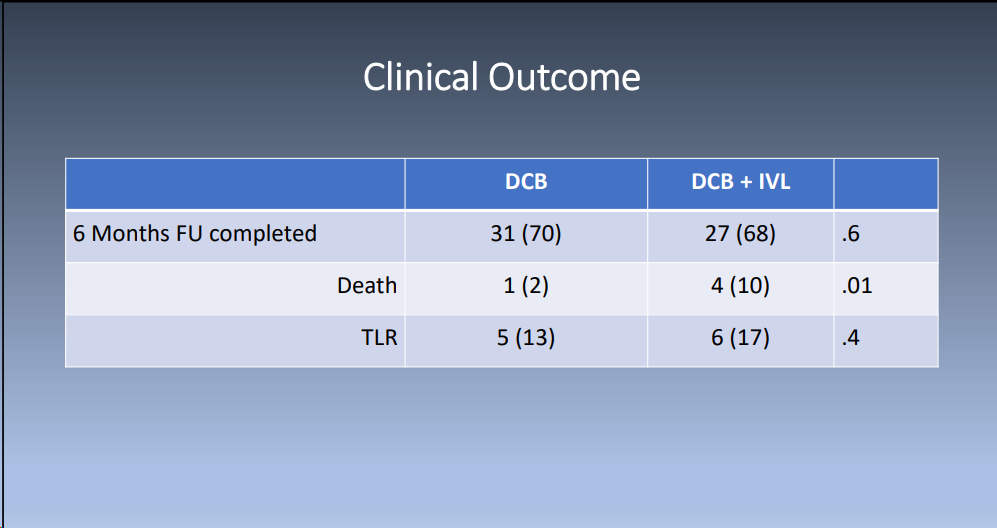
CLINICAL RESULTS: There was no statistical difference in the 6-month follow-up rates between the two groups. mortality was significantly lower in the DCB group, whereas the TLR rates were not statistically different. Further results are still being tallied.
Summary
The DEBATE-BTK SHOCK study evaluated the ability of IVL to improve the effectiveness of DCB drugs. Included patients had more complex lesions, consistent with real-world conditions, and contained more long-segment lesions and total occlusion lesions.
转载自《门诊》杂志


