Heavy stenosis and occlusive lesions at the beginning of the subclavian and vertebral arteries can cause blood flow in the vertebral artery on the affected side to retrograde into the distal end of the subclavian artery on the affected side, resulting in ischemia of the vertebral arteries or basilar arteries, which can in turn cause symptoms of ischemia in the affected limb. For the management of bilateral subclavian-vertebral artery lesions. At the 7th Vascular Innovation Forum (VINNOVA 2022), Prof. Kun Fang of Fu Wai Hospital, Chinese Academy of Medical Sciences, elaborated in detail the one-stop treatment strategy of composite surgery through two cases.

Case Sharing
Case 1 (Male, 56 years old) - Open + Interventional Simultaneous Management of Bilateral Subclavian Arteries
Complaint: dizziness with ataxia for 2 years.
Physical examination: low blood pressure in both upper extremities, normal blood pressure in both lower extremities.
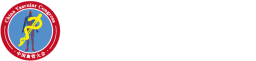
CTA: Occlusion of the long segment of the left subclavian artery and severe stenosis at the opening of the right subclavian artery.
SURGICAL STRATEGY: According to the 2017 ESVS guidelines for the diagnosis and management of peripheral arterial disease, surgical intervention is recommended for bilateral subclavian artery lesions, even in the absence of symptoms. Considering that for hardware facilities and technical conditions up to standard, the simultaneous one-stop treatment strategy is more advantageous. Therefore, a simultaneous one-stop treatment strategy of open (left side) + intervention (right side) was chosen. Based on the fact that open surgery requires blocking blood flow and the right side is less difficult to treat than the left side, the right side was treated first before the left side.
Procedure (1): aortic arch imaging suggests no forward flow in the bilateral vertebral arteries, delayed retrograde return of blood from the left vertebral artery, and low iFlow parameters in the bilateral subclavian arteries.
Surgical procedure (2): PTA + stenting was performed in the diseased segment of the right subclavian artery using the double guidewire protection technique, and the right vertebral artery was reexposed.
Surgical procedure (3): simultaneous left subclavian transverse incision, LCCA-LSA artificial vascular bypass surgery, LCCA blocked for 9 min.
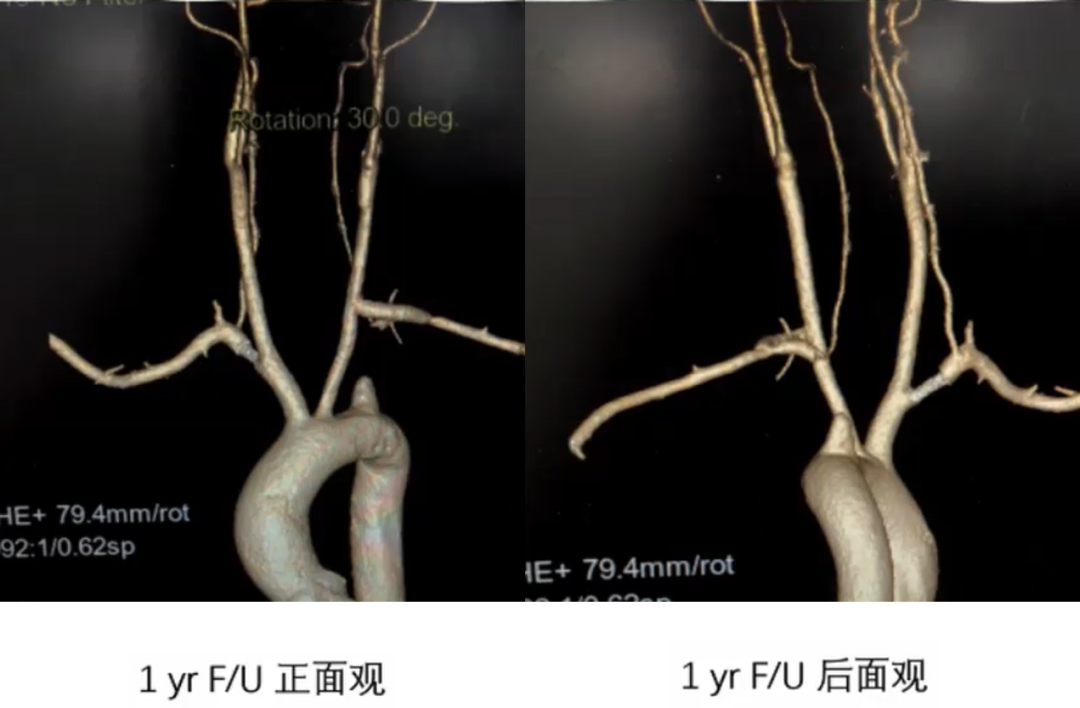
Repeat CTA at 1 and 2 years postoperatively: bilateral vertebral artery flow was restored to positive direction, and bilateral bypasses and stents were patent.
Case 2 (Male, 62 years old) - Open + Interventional Sequence for Bilateral Posterior Circulation Lesions
Complaint: right upper limb numbness with weakness for 3 years, intermittent dizziness.
Past history: history of left lower extremity arterial stenting.
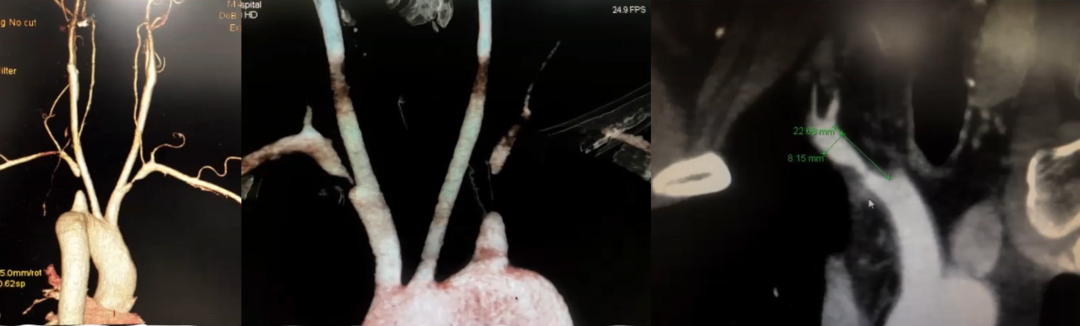
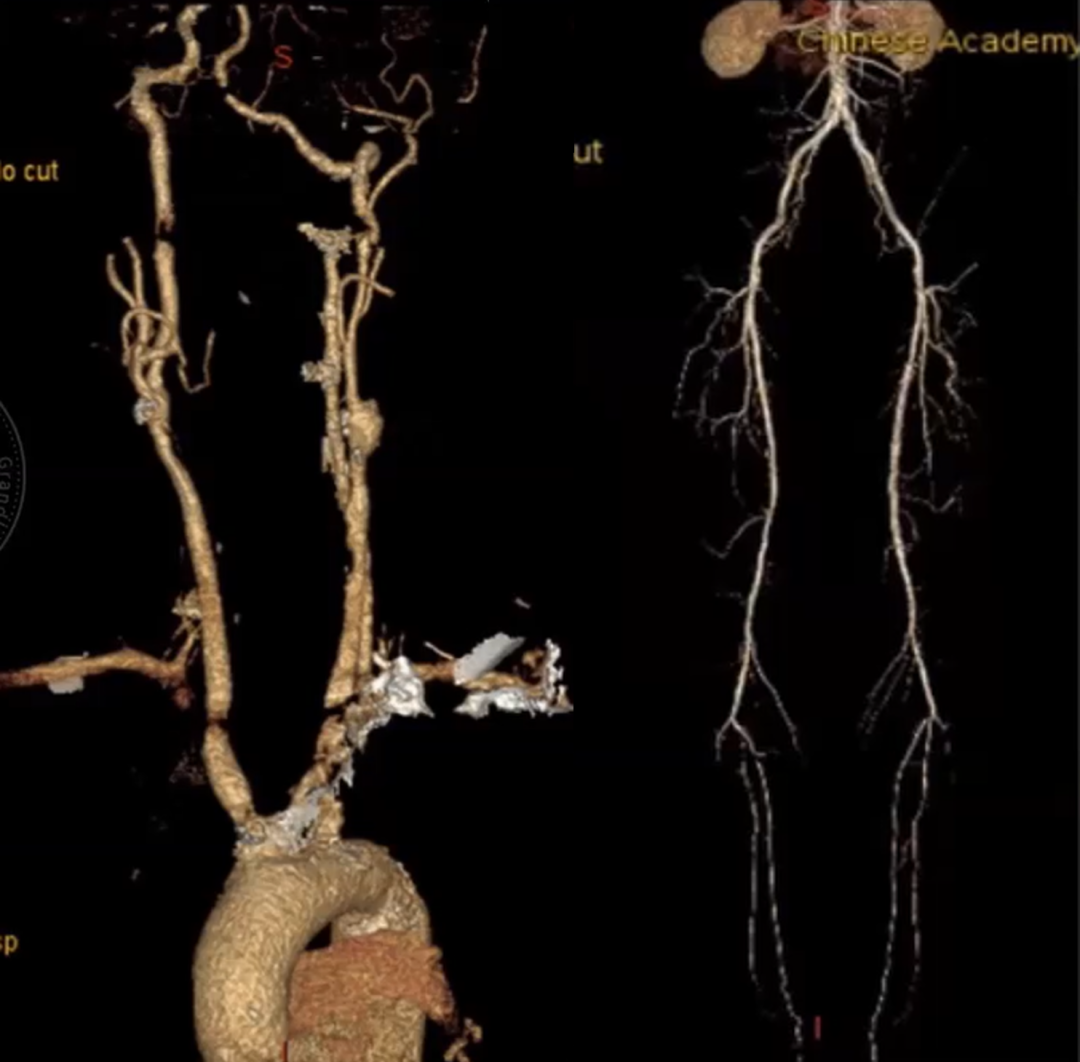
CTA:Stenosis at the opening of the left vertebral artery; occlusion of the right subclavian artery, stenosis of the right internal carotid artery and bilateral external carotid artery stenosis; severe stenosis of the bilateral anterior tibial arteries near occlusion and stenting of the left superficial femoral artery after stenting with stenting; multiple ulcers in the abdominal aorta and both iliac arteries, and stenosis of the internal iliac arteries of both iliac arteries >70%.
Preoperative diagnosis: pan-vascular disease with lesions involving the right subclavian, internal carotid, left vertebral, internal carotid, left renal, and left femoral arteries, atherosclerotic heart disease of the coronary arteries (left main stem + three branches lesions), type 2 diabetes mellitus, and old cerebral infarction.
Surgical strategy:open + interventional sequential management of bilateral posterior circulation lesions, + coronary artery bypass grafting.
Surgical procedure
First surgery:percutaneous left vertebral artery stenting on July 3, 2019
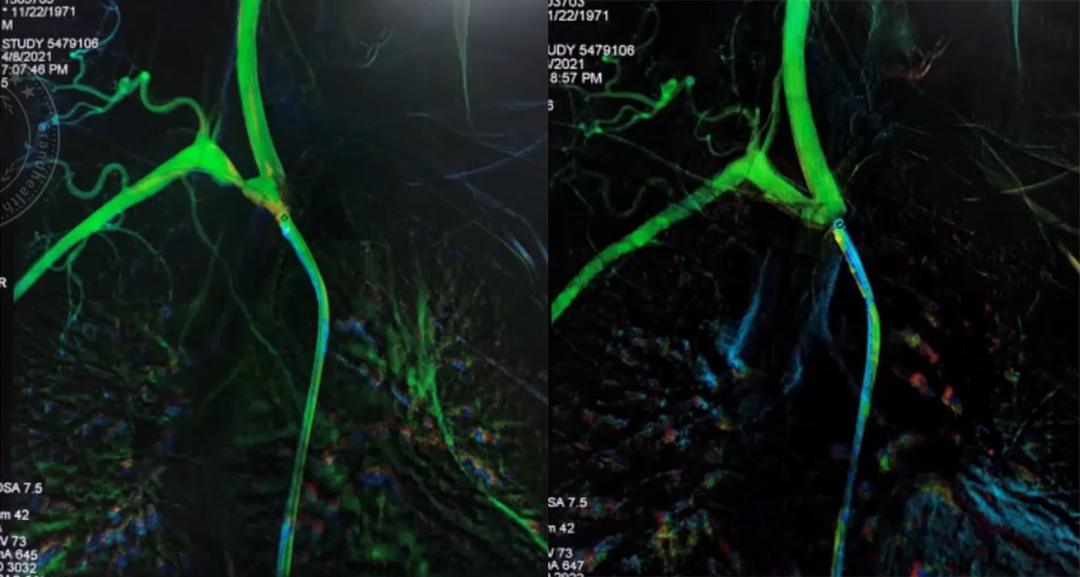
Surgical procedure (I):imaging showed normal aortic arch alignment, sclerotic plaque in the aortic arch, mild stenosis of both carotid arteries, mild stenosis of the left subclavian artery, occlusion of the right subclavian artery, retrograde blood flow of the right vertebral artery, and severe stenosis of the opening of the left vertebral artery; a double-guidewire protection technique was used, with the introduction of a 3 mm and 4 mm balloon to dilate the opening of the left vertebral artery.
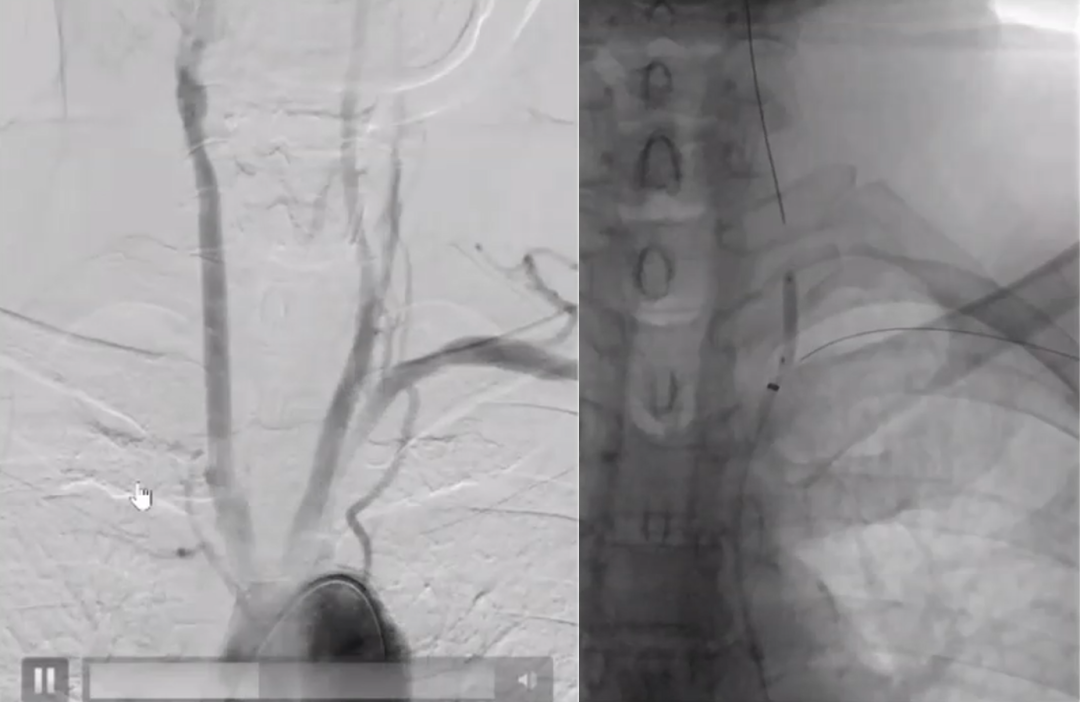
Surgical procedure (II):After balloon dilatation, elastic retraction was seen, and a 6×14 mm balloon stent was introduced into the opening of the left vertebral artery, which showed good blood flow on imaging, and the stenosis of the left vertebral artery was relieved. After the operation, the patient complained that the discomfort of the right upper limb improved significantly, and the imaging showed that the blood flow of the right subclavian artery improved.

Second surgery: right common carotid artery-right subclavian artery bypass on July 4, 2019
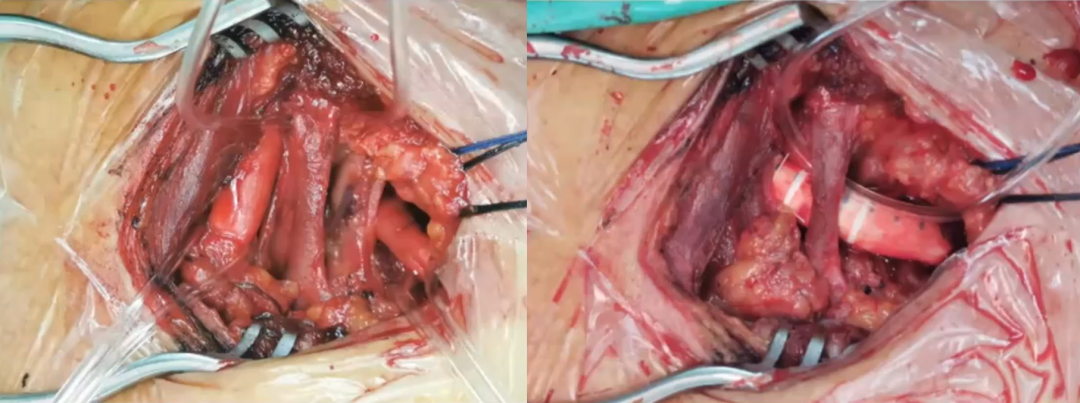
Surgical procedure (3): oblique incision at the anterior border of the right sternocleidomastoid, exploration revealed diffuse plaque from the opening of the right subclavian artery to the right vertebral artery, transection of the right subclavian artery, proximal ligation, distal endothelial stripping, plaque involvement of the opening of the vertebral artery, careful removal of the plaque, reinforcement of the endothelial sheet, and execution of the right subclavian artery-right common carotid end-side anastomosis.
Third Surgery: 5/9/2019, Coronary Artery Bypass Grafting.
Surgical procedure (4): preoperative imaging had indicated 70% proximal stenosis of the RCA, 99% in the middle segment, 90% proximal stenosis of the LAD, 90% proximal stenosis of the D1, and proximal occlusion of the LCX; a left internal mammary artery-anterior descending bypass graft was performed, an ascending aorta-diagonal graft graft was performed, an ascending aorta-obtuse rim graft graft was performed, and an ascending aorta-right coronary graft graft was performed.
Repeat CTA 2 years after surgery: right common carotid-right subclavian artery bridge vessel was patent and left vertebral artery stent was patent.

Summary
The pathophysiology of bilateral subclavian-vertebral artery pathology is somewhat altered by the way of the blood-stealing syndrome.
The principle of its treatment strategy and the development of the surgical program is from easy to difficult to ensure perioperative safety.
Individualized surgical strategies are selected according to the nature and extent of involvement of different lesions.
Hybridized one-stop surgery, integrating the advantages of open and endoluminal, simplifies surgical operation and reduces patient trauma.
For pan-vascular lesions, staged sequential treatment is recommended.
转载至《门诊》杂志