
With the application of stenting in lower limb arterial disease, the problem of in-stent restenosis (ISR) has gradually come to the fore. Selection of appropriate therapeutic options to deal with the ISR problem has become unavoidable.On July 13-16, 2023, at the 16th Southern China Vascular Congress (SEC 2023), Prof. Chang Guangqi's team from the First Affiliated Hospital of Sun Yat-sen University (SZU) shared a DAART procedure for the treatment of a case of in-stent restenosis of the superficial femoral artery.
Case analysis
Case information (male, 62 years old)
The main complaint:Intermittent claudication for 2 months 2 years after atherosclerotic occlusion of the left lower extremity.
Ntecedent history:Hypertension for more than 10 years, atrial fibrillation for 2 years, hemiparesis of the left upper limb caused by a stroke 10 months ago; diabetes mellitus was denied; balloon dilatation stenting of the left iliofemoral artery of the lower limb was performed 3 years ago; balloon dilatation stenting of the left superficial femoral artery was performed more than a year ago.
Personal history:Smoked for over 30 years, about 1 pack a day, no alcohol.
Body check:The skin of both feet was warm and cool, with bilateral femoral artery pulsations (+), right popliteal and dorsalis pedis artery pulsations were diminished, and left popliteal and dorsalis pedis artery pulsations were not palpated.
ABI:0.59 (left), 0.95 (right).
Diagnosis:1, in-stent restenosis of the left lower extremity artery; 2, atherosclerotic occlusive disease of both lower extremities; 3, hypertension (very high risk); 4, atrial fibrillation; 5, cerebral infarction.
CTA:1, post-stenting changes in the left femoral artery with moderate-to-severe narrowing of the lumen, which was poorly displayed and could not be excluded from the occlusion; 2, limited mild narrowing of the proximal lumen of the right posterior tibial artery, incomplete occlusion of the proximal segment of the right anterior tibial artery to intermittent severe stenosis in the distal segment, which was comparable to that of the previous one; 3, occlusion of the right internal iliac artery.

Surgical plan:Under local anesthesia, left superficial femoral artery stent occlusion plaque rotary resection + overlay stent implantation + lower extremity artery balloon dilatation angioplasty + lower extremity artery drug-coated balloon dilatation angioplasty were performed.
Surgical procedure
Procedure (1):right femoral artery approach, tumble hill to left common iliac artery imaging showed good morphology of the left common iliac stent with smooth blood flow, and patency of the left iliac artery, external iliac, common femoral, and deep femoral arteries. Converting the 8F tumbling sheath, the guidewire catheter was lowered to the superficial femoral artery imaging showed severe stenosis of the proximal left superficial femoral artery with complete occlusion in the stent, and the popliteal artery was patent, with a delayed visualization.
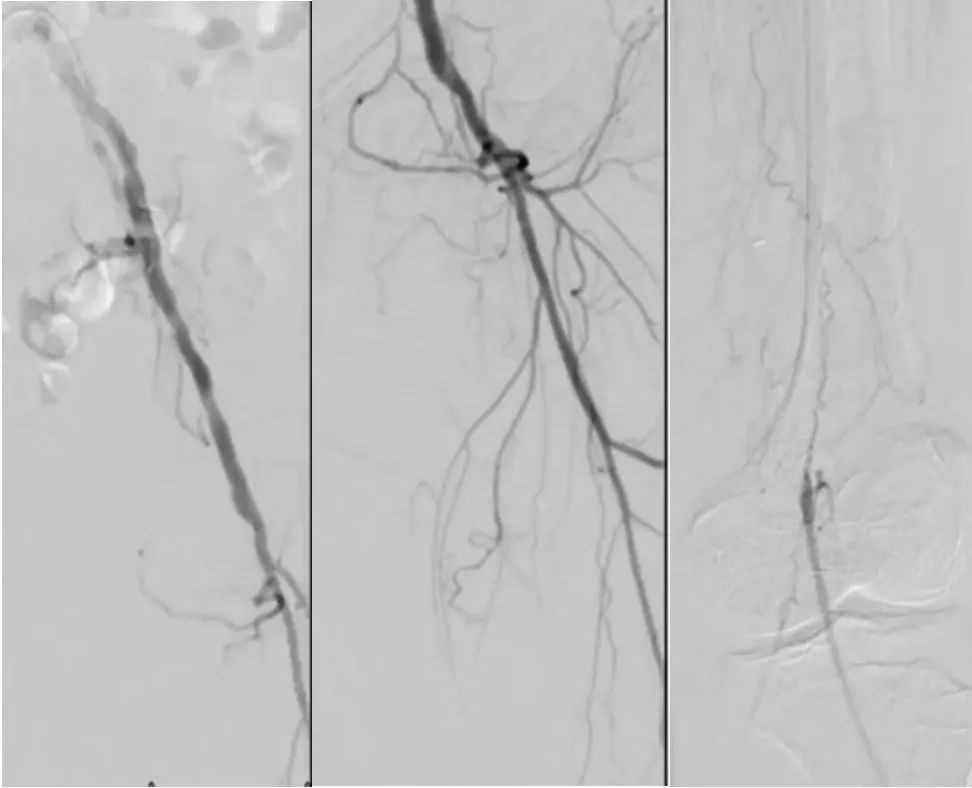
Procedure (2):Command-18 guidewire with 4F MP catheter was passed through the stent occluded segment to the lower part of superficial femoral artery in the true lumen; angiography showed that the blood flow of popliteal, anterior tibial, and peroneal arteries was smooth, and the posterior tibial artery was occluded throughout the whole process. A 2×200 mm Armada balloon was introduced to open the superficial femoral artery and the occluded segment in the stent.
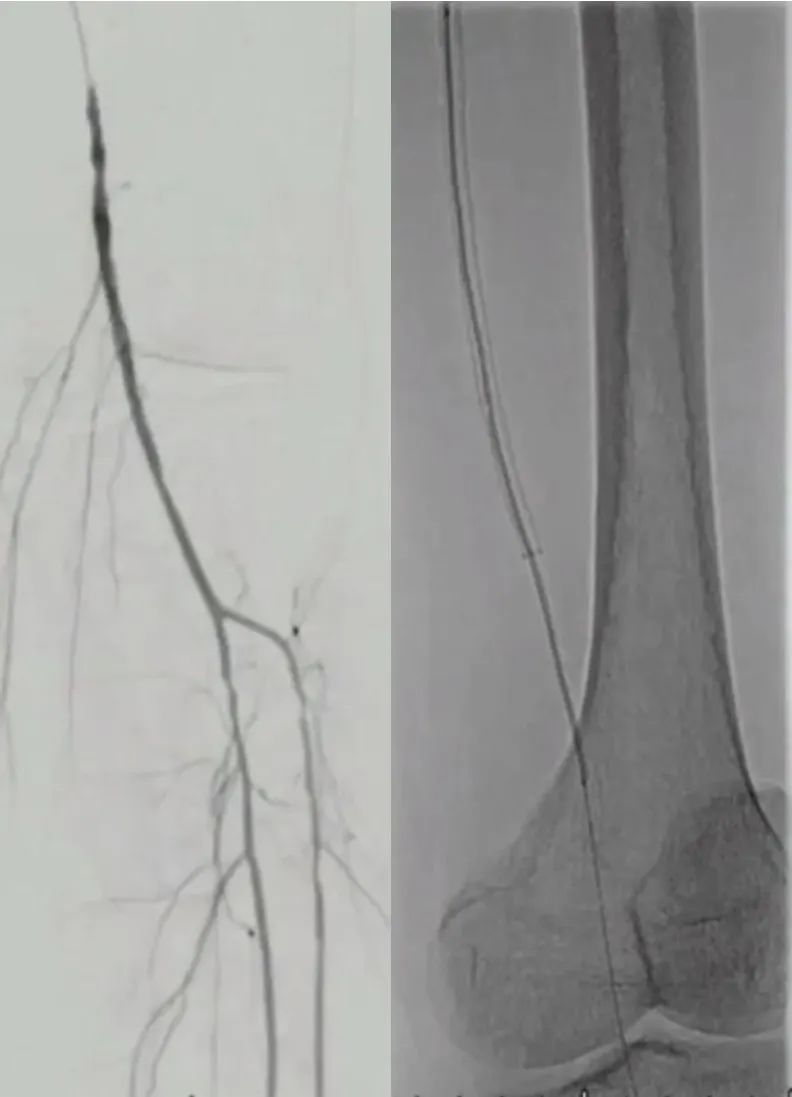
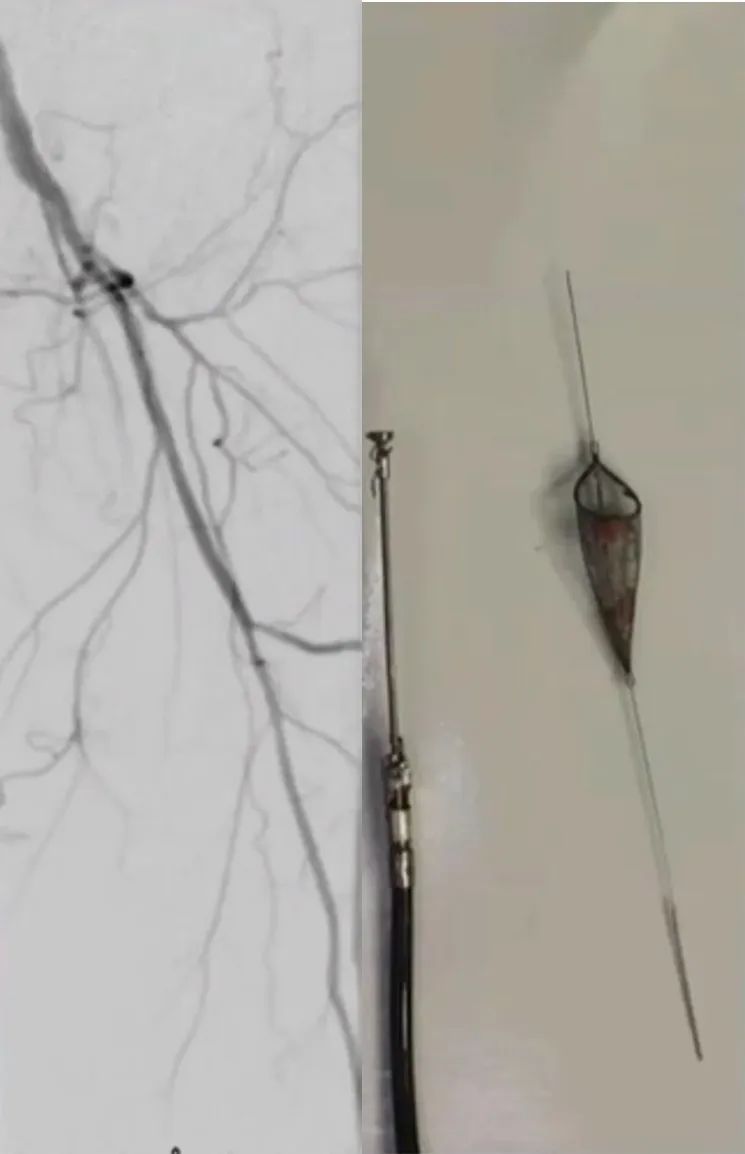
Procedure (3):A Spider umbrella was placed in the distal popliteal artery, and the TurboHawk peripheral plaque excision system was introduced to cut out a large amount of endovascular plaque by rotary dissection of the intima and plaque of the stenosed and occluded segment of the artery in segments starting from the beginning of the superficial femoral artery up to the patellar level.
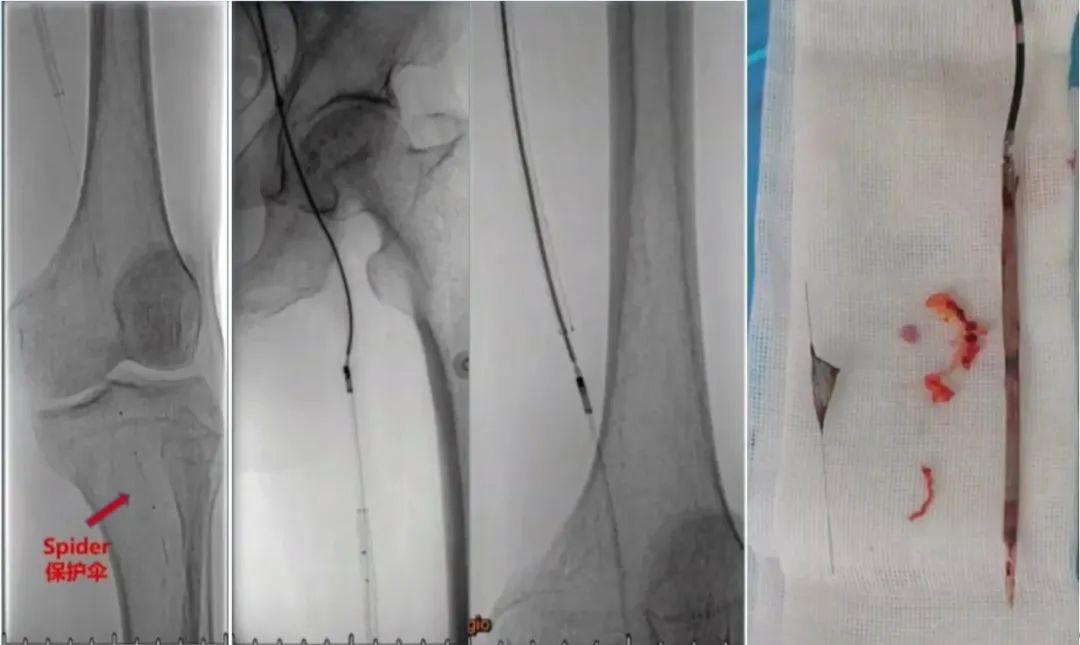
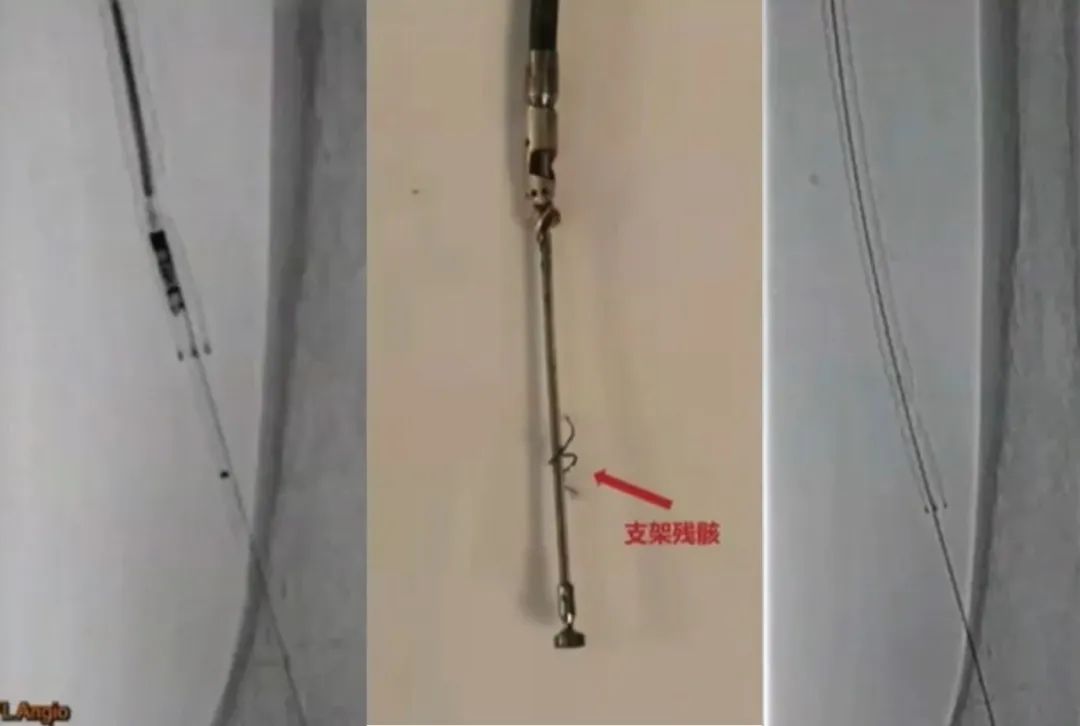
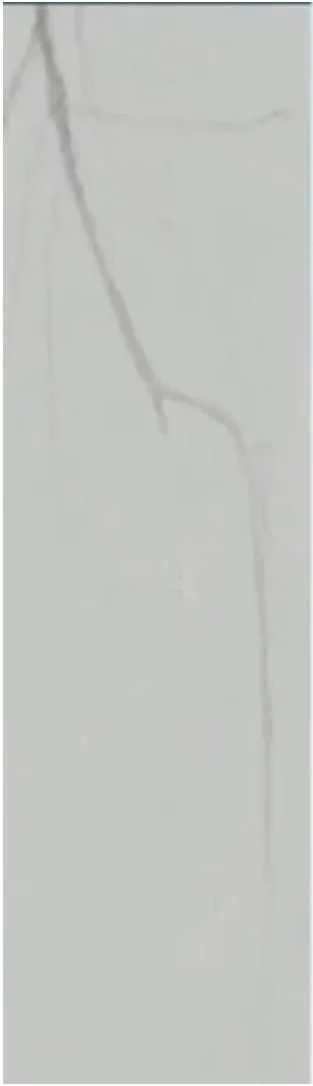
Procedure (4):During re-spinning, the spinning system cuts and wraps around the stent, causing the stent to break and deform.
Procedure (5):Imaging showed residual moderate-to-severe stenosis in the upper superficial femoral artery and proximal to the stent, which was slow to develop, with no development in the middle or distal portion of the stent. The Spider umbrella was withdrawn, and interception of dislodged plaque within the umbrella was seen.
Procedure (6):A 4×200 mm Armada balloon was introduced to dilate the stenosed occluded segment of the superficial femoral artery.
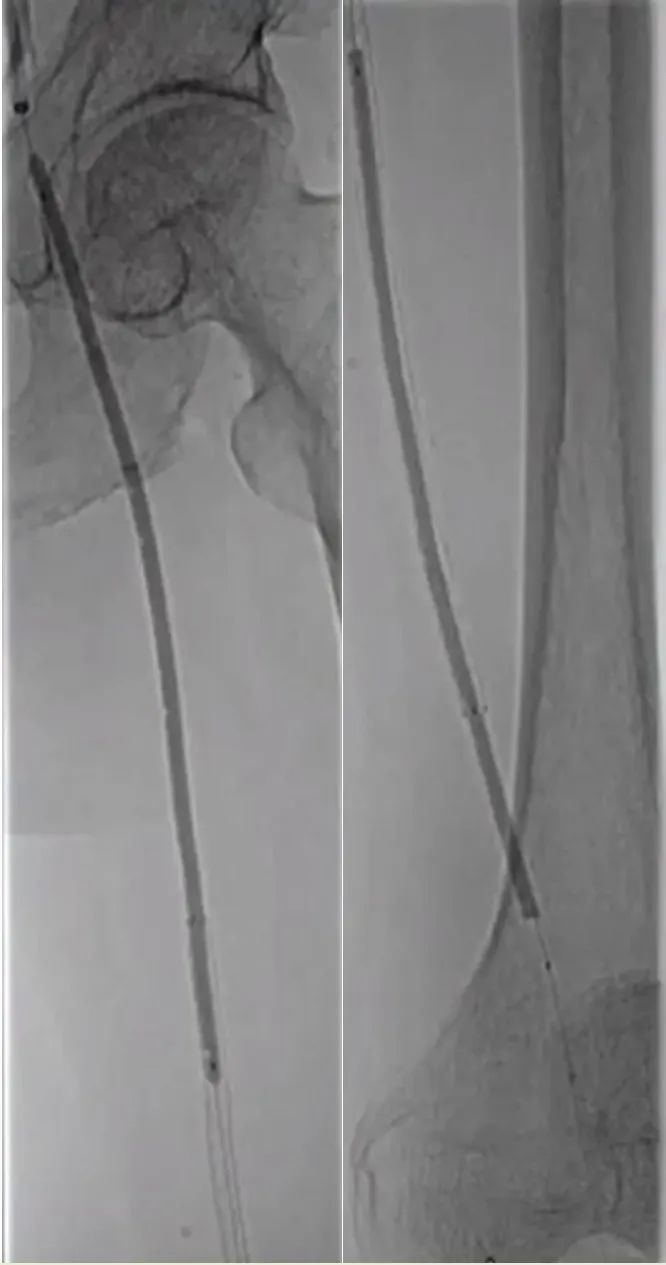
Surgical procedure (7):implantation of a 5×150 mm Viabhan stent to cover the original stent break, followed by posterior dilatation using a 4×200 mm Armada balloon; dilatation of the superficial femoral artery opening to the upper segment of the superficial femoral artery stent using a 5×220 mm Reewarm DCB.

Surgical procedure (8):The imaging showed slow visualization of superficial femoral artery and popliteal artery, smooth blood flow of anterior tibial artery, and no visualization beyond the opening of peroneal artery, and embolization of peroneal artery was considered.
Procedure (9):The peroneal artery was dilated using a 2×200 mm Armada balloon and a 2.5×40 mm Pacific balloon.

Procedure (10):superficial femoral and popliteal artery blood flow, anterior tibial artery and peroneal artery blood flow is smooth, flow velocity increases, and plantar blood perfusion improves significantly.
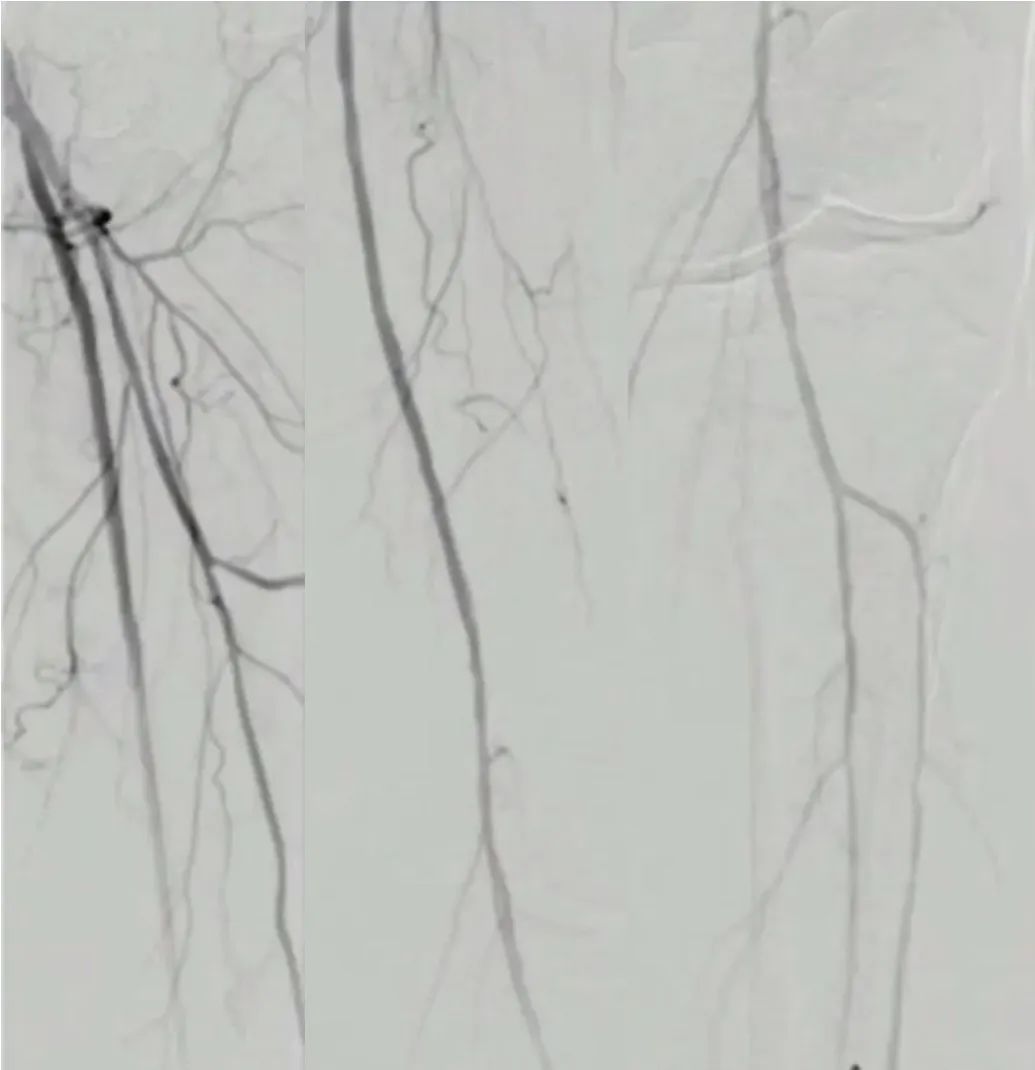
Postoperatively, he was treated with antiplatelet, anticoagulation and vasodilation. The patient complained that the pain, coldness and numbness of the left lower limb were relieved, and he could move down to the ground, with significant improvement in motor function and pain relief.The ABI was significantly improved, and the left side was raised to 0.88.
He was discharged from the hospital 2 days after the operation and discharged with medication:Bayrettol tablets, 2.5 mg BID; bacitracin enteric-coated tablets, 0.1 g QD; beraprost tablets, 40 ug BID; and Lipitor tablets, 20 mg QN.
Summary
The DAART technique is less invasive, improves the outcome of DCB in calcified lesions, and is in line with the "Leaving Nothing Behind" concept, which has been confirmed by the RCT study in complex femoropopliteal artery lesions. The success of this case demonstrates the value of DAART in ISR lesions.
文章来源:《门诊》


