
Systemic hemodynamics is dependent on several parameters, including cardiac function, valve function, aortic compliance, and peripheral vascular resistance. The aortic arch, although a very small part of the total aorta, accounts for 50% of total arterial compliance. Therefore, aortic arch anatomical alterations may have a profound effect on systemic arterial compliance. At the 50th International Vascular and Endoluminal Vascular Congress (VEITH 2023), November 14-18, U.S. local time, Professor Jean Bismuth from the University of South Florida shared the changes in aortic valve and aortic morphology after ascending aortic and arch graft implantation.
Potential Effects of TEVAR on Cardiac Function

The aorta contains a large number of elastic fibers that cushion the shock of cardiac blood flow during cardiac contraction, storing about 50% of the left ventricular per-beat volume during systole. Atherosclerosis of the aorta is detrimental to its contraction and expansion, and the degree of sclerosis is influenced by factors such as age, hypertension, diabetes mellitus, abdominal visceral fat, and smoking. Decreased aortic compliance leads to left ventricular hypertrophy. Left ventricular hypertrophy and atherosclerosis lead to left ventricular hypodiastolic function.
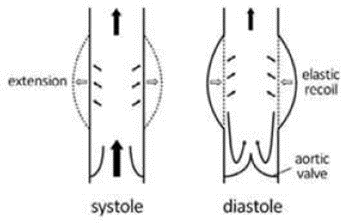
Pulse wave velocity (PWV) is a measure of blood flow velocity that can be used to assess arterial vascular compliance and reflect the degree of atherosclerosis. Higher PWV indicates decreased aortic vascular elasticity and increased atherosclerosis. When PWV increases, during systole, retrograde waves from peripheral vascular resistance reach the ascending aorta, resulting in increased systolic and decreased diastolic blood pressure. This in turn causes an increase in pulse pressure and systemic afterload, leading to cardiovascular events and long-term diastolic insufficiency.
A retrospective analysis that included 89 patients with arch aneurysms who underwent surgical treatment showed that all implants caused an increase in PWV, with stent grafts having the most significant increasing effect. Not only that, the longer the stent graft, the more pronounced the increase in PWV. β-Blockers decreased PWV postoperatively.
A study that included 40 patients treated with EVAR was followed up for 1 year after surgery. The results suggested that 13/22 patients had a reduced ET within 1 year postoperatively, and left ventricular mass index (LVMI) and left atrial volume index were significantly higher postoperatively.
Aortic valve and aortic lesions
The physical properties of the ascending aorta (AA), as a cushioning vessel for left ventricular ejection, play a determining role in left ventricular ejection afterload. Dilatation of the ascending aorta is a common aortic disorder with a prevalence of approximately 20% to 25% in patients with aortic stenosis, which is similar to the prevalence of dilatation of the ascending aorta in patients undergoing TAVR (22%).
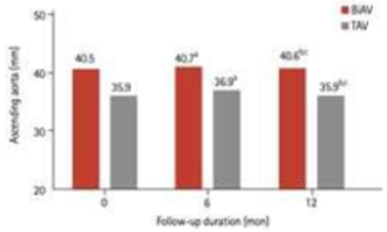
Before TAVR, patients with severe aortic stenosis (AS) combined with a bileaflet aortic valve (BiAV) had a significantly larger diameter of the ascending aorta than patients with severe AS combined with a TAV. At 12 months after TAVR, ascending aortic dimensions in patients with severe AS combined with BiAV remained stable without further dilatation. The available studies do not support concerns about progression of ascending aortic lesions in patients with BiAV. Overall, TAVR prevented further progression of aortic dilatation in BiAV and TAV and may correct hemodynamic disturbances.
CT measurements showed significantly higher leaflet calcification volume and aortic root angulation in the dilated ascending aorta group (P < 0.001). Dilated ascending aorta was diagnosed in almost one-fourth of the patients treated with TAVR. The risk of intraoperative adverse aortic events was lower in patients undergoing TAVR for ascending aortic dilatation.Neither in-hospital mortality nor midterm survival after TAVR was affected by ascending aortic dilatation.
Summary
Aortic compliance is altered after aortic stent-grafting, which in turn has a significant long-term impact on cardiac function; and there may be differences between devices based on the mechanical properties of the stent.At 1 year after TAVR, follow-up with EKG-gated CTA suggests that AA diameters remain relatively stable. Further studies are needed to assess the evolution of AA in medium- and long-term follow-up and to identify patients at risk of combined aortic dilatation.


