The 13th Central Plains Vascular Forum (CPEC2023) and CPEC International Experts Forum (World Experts@CPEC,WE@CPEC), the Annual Meeting of Vascular Surgery Management Branch of Henan Provincial Hospital Association, the Annual Meeting of Vascular Surgery Physicians Branch of Henan Provincial Physicians Association, the Nursing Forum of Central Plains Vascular Forum, the Annual Meeting of Central Plains Vascular Reduction Alliance (CPED), and the Annual Meeting of Henan Venous Union (Henan Venous Union), which are co-sponsored by Henan Provincial People's Hospital, Fuwai Hospital of Huazhong Province, Henan Provincial Physicians Association, Henan Provincial Hospital Association, Beijing Cihua Medical Development Foundation, and Beijing China Kanglian Public Welfare Foundation The 13th Central Plains Vascular Forum (CPEC2023) and CPEC International Expert Forum (World Experts@CPEC,WE@CPEC), 2023 Annual Meeting of Vascular Surgery Management Branch of Henan Provincial Hospital Association, Annual Meeting of Vascular Surgeon Branch of Henan Provincial Physicians' Association, Nursing Forum of Central Plains Vascular Forum, Central Plains Vascular Decompression Union (CPED) Annual Meeting and Henan Venous Union (HNPU) Annual Meeting were held on July 20-22, 2023, which is the first time that CPEC has been held in Henan Province.
In a special session on aorta, Prof. Zhai Shuiting of Henan Provincial People's Hospital shared "Diagnosis and Treatment of Primary Aortic Appendage Thrombosis", welcome to read.

PAMT Definition
Compared to common large artery diseases such as aortic coarctation and aortic aneurysm, primary aortic appendage thrombosis (PAMT) is a relatively uncommon clinical condition, with occasional appendage thrombosis seen in the ascending, descending, or abdominal aorta.
Primary aortic appendage thrombosis (PAMT) is a thrombus formation that attaches to the aortic wall in the absence of atheromatous lesions, atherosclerotic lesions of the aorta, any thrombosis of cardiac origin, or disease or any embolus of cardiac origin.
First proposed by Weissman and Tobin in 1958.
Epidemiology
The PAMT autopsy detection rate was 0.45%, which is higher than the actual clinical patient detection rate.
Most of the patients are asymptomatic and are often detected by the presence of some symptoms or signs of embolization of limb arteries and visceral arteries. The detection rate has increased in recent years with the development of imaging technology.
The prevalence of PAMT in men and women is 1:19.
The average age at diagnosis ranged from 40 to 56 years.
PAMT Etiology
The etiology and pathogenesis of the disease are currently unknown and may be related to autoimmune diseases, arterial wall tumors or neoplasms, closed aortic trauma, infections, or chemotherapy, as well as some endoluminal medical manipulations; inherited thrombotic disorders; primary thrombocythemia, erythrocytosis; antiphospholipid syndromes, hyperhomocysteinemia, familial fibrinogen disorders; and heparin-induced thrombocytopenia.
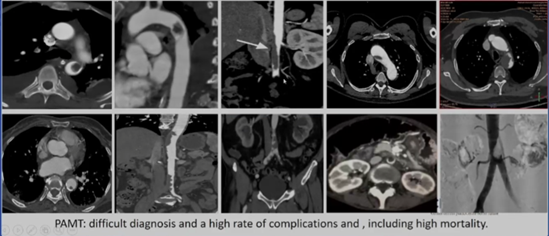
PAMT Disease Staging
Depending on the anatomical site where the thrombus occurs, it can be categorized into types I to IV:
Type I: ascending aorta and aortic arch appendage thrombus (distal to proximal left subclavian artery)
Ⅰa: thrombus mainly confined to the ascending aorta
Ⅰb: thrombus involving the aortic arch
Type II: thrombus in the appendage of the main coronary artery (from the distal left subclavian artery to the celiac artery)
IIa: descending thoracic aortic appendage thrombus above T8
IIb: thrombus located in the descending thoracic aorta below T8-L1 to the abdominal aorta above the celiac artery
Type III: thrombus located in the abdominal aorta below the celiac artery to above the lowest renal artery
Type IV: appendage thrombus below the lowest renal artery to the aortic bifurcation
Depending on the nature of the thrombus it can be categorized as S, P, or O:
Type S (sessile): eccentric or concentric thrombus, without floating component.
Type P (pedunculated): pedunculated thrombus (walled thrombus attached to proximal aorta, distal free segment of variable length)
Type O(occlusion): complete thrombotic occlusion of the aorta.
Clinical manifestations of PAMT
The clinical presentation of PAMT is usually asymptomatic until embolization occurs.82% of PAMT is diagnosed after embolization. The most common site of embolization is the lower extremities, followed by the visceral arteries and the brain.The most common site of PAMT is the descending aorta (74%), especially at the junction of the aortic arch and the descending aorta, followed by the abdominal aorta (14%) and the ascending aorta (12%).PAMT evolves from death in 6% of cases.
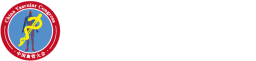
PAMT Diagnosis
Ultrasound (transthoracic echocardiography and transesophageal echocardiography) is commonly used in the clinic to screen for the presence and source of thrombus. If the source is not identified, a full aortic CTA is preferred.All patients presenting with acute arterial thrombosis should be thoroughly evaluated to determine the likely source of the embolism.
PAMT Treatment Strategy
There is no consensus on the ideal treatment for PAMT. In order to avoid potentially catastrophic consequences triggered by peripheral and/or visceral embolization, the following interventional techniques and therapeutic regimens are commonly used: anticoagulation, thrombolysis, thrombus aspiration, intraluminal septostomy, hybridization, open thrombus endothelial debridement, and graft replacement, with systemic anticoagulation being a widely used treatment.
Therapeutic Strategies for Type I PAMT
1、Anticoagulation and close imaging follow-up for small S-shaped thrombi.
2、Type Ib uses anticoagulation, systemic thrombolysis and thrombectomy.
3、For large non-S-type thrombi with a high risk of recurrent embolization, consider surgical retrieval of the thrombus or implantation of a stent by hybridization techniques.
Therapeutic Strategies for Type II PAMT
1、Compared with anticoagulation alone, endoluminal stenting is feasible, which reduces the risk of residual thrombus and recurrent embolism by isolating the adherent thrombus with a coated stent, and has fewer perioperative complications than surgical retrieval of the thrombus.
2、Stent oversize ≤5% without balloon dilatation.
3、Cover the thrombus for at least 2 cm to avoid extrusion of the thrombus, leading to recurrence of distal embolization.
4、Closed-loop stents reduce the risk of spinal cord ischemia.
Therapeutic strategies for type III PAMT
1、Type III treatment presents significant challenges because of the involvement of visceral vessels and the risk of visceral vessel embolization with unprotected transfemoral thrombolysis.
2、The thrombus can be removed under balloon protection, blocking the visceral artery to avoid dislodging the thrombus.
3、The aorta can also be incised through a posterior approach to retrieve the bolus.
Therapeutic Strategies for Type IV PAMT
1、Anticoagulation alone
2、CDT
3、aortic thrombectomy
4、stenting
Case Sharing
Case 1 For the ascending aortic appendage thrombus, caused the upper extremity vascular embolization time, if the thrombus dislodgement occurs again, there is a risk of stroke, so the choice of incision and thrombus extraction, intraoperative finding of the presence of aortic neoplasm, neoplasm on the appendage thrombus occurs, the pathology results show that the neoplasm bit fibrotic blood vessels, fat tissue proliferation, the line of the ascending aorta after the replacement of the therapeutic effect of the good.
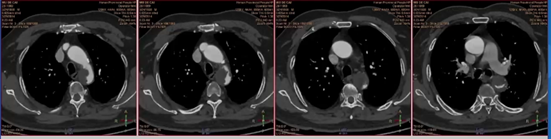
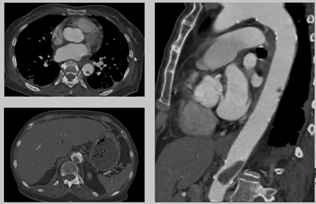
Case 1 preoperative CTA
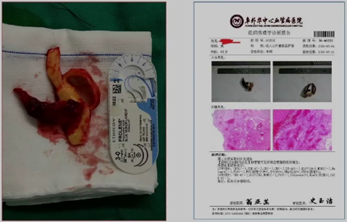
Intraoperative neoplastic organisms and their pathologic findings
Case 1 postoperative CTA
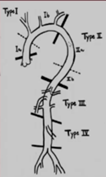
Case 2 was a type II PAMT, the thrombus was located in the descending aorta, and the cross-sectional view showed a large area of thrombus obstruction, which had a large impact on the left ventricular load, and TEVAR combined with stenting of the left common iliac artery was adopted, which had a good therapeutic effect.
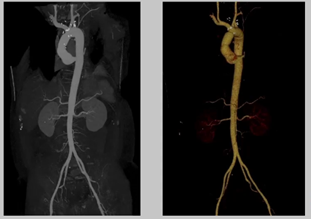
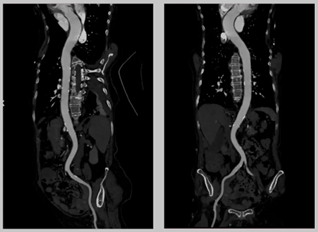
Case 2 preoperative CTA
Case 2 postoperative CTA
Case 3 was an 88-year-old woman with the presence of small, multi-segmented, floating thrombus, which was treated with antiplatelet anticoagulation only due to advanced age, and the thrombus was eliminated after two weeks with a favorable outcome.
Case 3 preoperative CTA
Case 3 Two weeks after antiplatelet anticoagulation therapy
Case IV was a 77-year-old woman with type III IV mixed PAMT, in which the renal artery and superior mesenteric aorta were protected with dilatation balloons, and abdominal aortic balloon dilatation and thrombolysis was performed. Postoperatively, the aortic thrombus was eliminated, and the visceral artery and aortic blood flow were satisfactory.
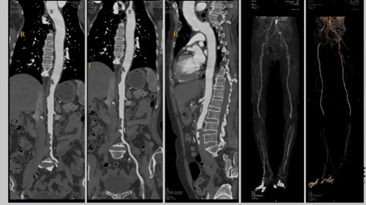
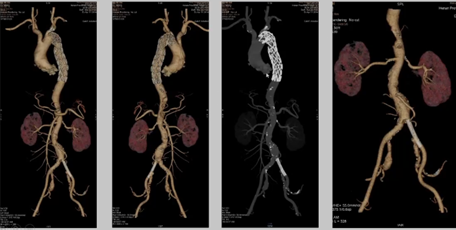
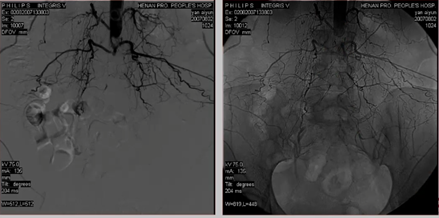
Case 4 preoperative CTA
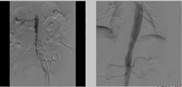
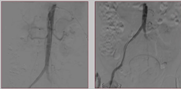
Case 4 intraoperative contrast

Case 4 postoperative CTA
Case 5 is type IV PAMT, the symptomatic manifestation is easily confused with aortoiliac artery occlusion, generally PAMT patients are acute symptoms, aortoiliac artery occlusion is chronic symptoms, can also be used catheterization to try to explore the texture of the lesion, if it is a thrombus, it can be thrombolysis through the CDT, the case thrombolysis after the effect is good.
Case 5 preoperative imaging

Case 5 Thrombolysis 2 days, 6 days after imaging
Summary
1、If a distal embolic event has occurred, the source of the embolus needs to be sought, and in the case of PAMT, the etiology needs to be actively sought.
2、There is still no unified expert consensus on the treatment of PAMT.
3、For PAMT, early and aggressive anticoagulation is beneficial in preventing recurrence, reducing complications and optimizing prognosis.
4、Individualized treatment plan should be considered comprehensively according to the location of PAMT, anatomical features, thrombus typing, clinical manifestations and comorbidities (whether it caused severe embolic time).
Expert Profiles

Prof. Zhai Shuiting
Henan Provincial People's Hospital
Director of Vascular Surgery and Large Vessel Surgery, Henan Provincial People's Hospital & Huazhong Fu Wai Hospital. Chief Physician, Master's Degree Tutor.
Chairman, Vascular Surgery Branch, Henan Provincial Physicians Association; and
Chairman, Vascular Surgery Management Branch, Henan Hospital Association; Member, Vascular Surgery Group, Chinese Medical Association.
Member of Vascular Surgery Group of Chinese Medical Association.
Member of Interventional Group of Chinese Medical Association Radiology Branch.
Member of Vascular Surgery Group of Chinese Medical Association; Member of Interventional Group of Chinese Medical Association; Member of Vascular Surgery Group of Chinese Medical Association.
Member of the Interventionalists Branch, Chinese Physicians Association.
Vice Chairman of Abdominal Aortic Group, Vascular Surgery Branch, Chinese Medical Doctors' Association.
Executive Director of China Interventional Medicine Industry Technology Innovation Alliance.
Corresponding Editor of the Editorial Board of the Chinese Journal of Radiology; Editorial Board Member of the Chinese Journal of Vascular Surgery; Standing Editorial Board Member of the Chinese Journal of Vascular Surgery; Editorial Board Member of the Chinese Journal of Interventional Imaging and Therapeutics.
Expert of Health Care Consultation for Cadres of Henan Provincial Health Care Committee
In 1992, he went to Japan to study interventional and DSA technology.
In 2005, he went to France to study interventional therapy.
In 2012, he went to Albany Medical Center in Albany, New York, USA to receive Endovascular Surgery Fellowship from the American College of Vascular Surgery.
In 2012, he founded the Department of Vascular Surgery of Henan Provincial People's Hospital.
Founded the Department of Vascular Surgery and Department of Large Vessel Surgery, Fu Wai Huazhong Hospital for Cardiovascular Diseases in 2017.
Specialty: endovascular treatment and hybridization of aortic and other peripheral vascular diseases. He is the first in Henan Province to carry out vascular endoluminal therapy and hybridization therapy for aortic coarctation and abdominal aortic aneurysm. Transjugular Intrahepatic Porto-Venous Shunt (TIPS), Carotid Artery Stenosis Stenting (CAS), Intravascular Rotary Cutting, Excimer Laser Treatment for Lower Extremity Atherosclerotic Occlusive Disease, etc. have filled the gaps in the province. He is the first one who invented the "Trans-Entero-Superior Mesenteric Vein Extrahepatic Portal Shunt (TEPS)" to treat portal cavernous degeneration at home and abroad. He has been invited to the United States, Germany, etc. to participate in international academic conferences and give academic lectures.
He has published more than 120 papers and edited 3 monographs. She has won the first prize of Provincial Scientific and Technological Achievements, the first prize of Henan Medical Science and Technology Award, and the third prize of Henan Science and Technology Progress Award: she has presided over and participated in more than 20 scientific research projects, and has obtained 6 national utility model patents.
文章来源:血管资讯