
VEITH symposium is one of the most authoritative, large-scale and long-standing academic events in vascular surgery in the world. Thousands of top experts from vascular surgery, interventional radiology, interventional cardiac surgery, and other vascular surgery fields from around the world attend the VEITH symposium conference each year. Here brings together various research data updates from the world, very pioneering, prospective and controversial topic discussion, clinical technology sharing with great application value, the latest and cutting-edge medical devices and technology exploration, face-to-face communication opportunities for world-class authoritative vascular surgery experts, and so on.
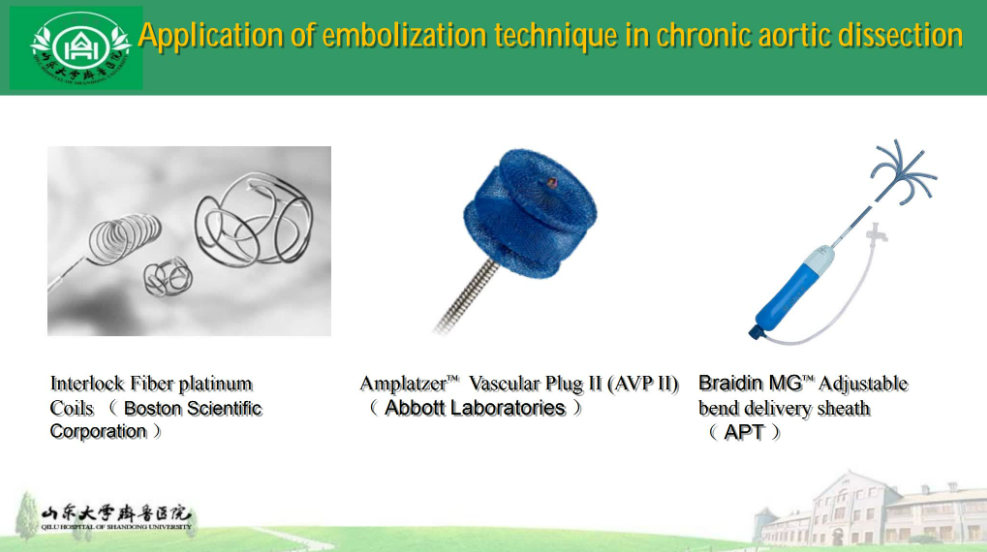
On November 14, 2023, during the International Congress of Vascular and Endovascular Angiology (VEITH symposium) held at the Hilton Hotel, New York Center, USA, Professor Jiang Jianjun from Qilu Hospital of Shandong University gave a wonderful speech on the topic of "Application of Embolization Technology in Chronic Aortic Dissection".

JIANG Jianjun
Qilu Hospital of Shandong University
Case 1
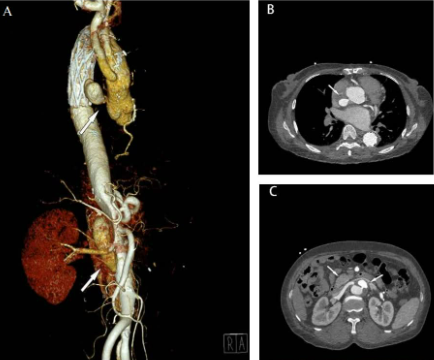
A 51-year-old woman underwent stented elephant trunk total aortic arch replacement for type A aortic dissection 2 years ago
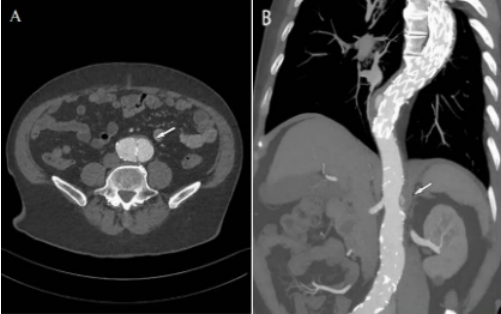
01、Preoperative assessment
1)Preoperative CTA reconstruction: aortic aneurysm following dissection at the origin of the ascending aorta and in the abdominal aorta extending from the celiac trunk to the left iliac artery (white arrows)
2)Preoperative transverse CTA: tear at the origin of the ascending aorta and dissected aortic aneurysm (white arrow)
3)Preoperative transverse CTA: laceration at the origin of the right renal artery, supplied by the true and false lumen (white arrows)
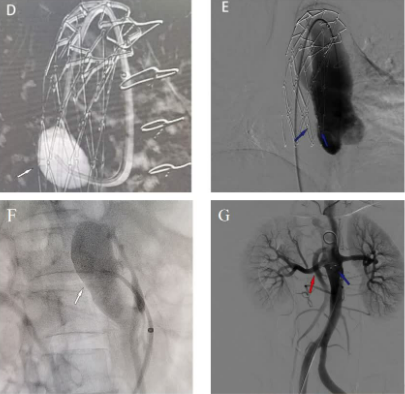
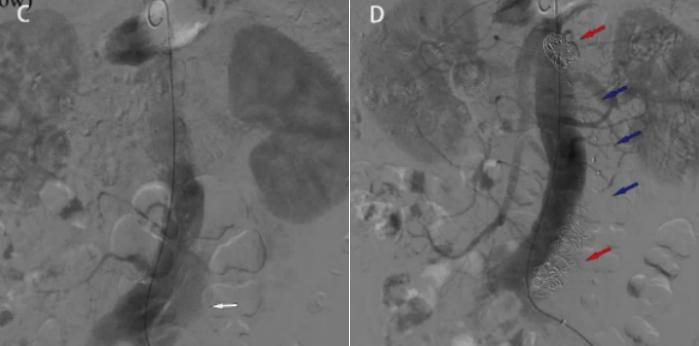
02、Surgical procedures
1) Passing the catheter through the tear in the ascending aorta, localizing and entering the aneurysm cavity (white arrow)
2) AVPII (4 mm 7 mm) was used to seal the ascending aortic tear, and the aortic aneurysm was no longer visible after dissection (blue arrow)
3) Guide catheter from true lumen through tear into false lumen (white arrow)
4) An AVPII (10 * 7 mm) occluder (blue arrow) was placed at the tear and a covered stent (7 x 25 mm GORE Viabahn) was placed in the right renal artery (red arrow)
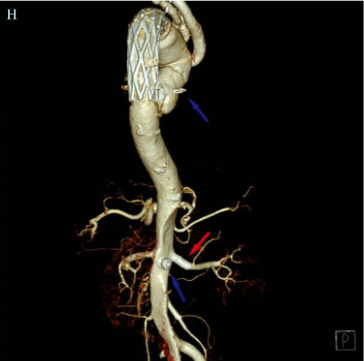
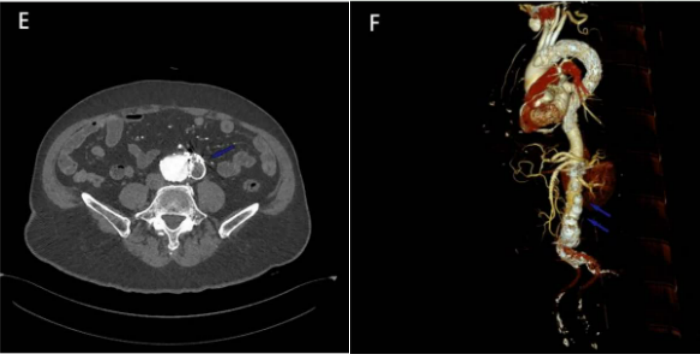
03、Follow-up Results
At 6-month follow-up, CTA reconstruction showed complete thrombosis of the ascending aortic aneurysm and abdominal aortic aneurysm
AVP high density image (blue arrow); renal artery covered stent (red arrow)
Case 2
A 62-year-old male received TEVAR 9 months ago for type B aortic dissection
01、Preoperative assessment
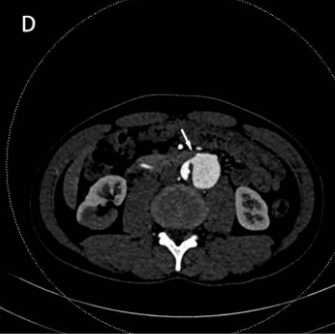
1) Preoperative transverse section CTA: after abdominal aortic aneurysm dissection, the maximum diameter is about 52 mm, extending to both iliac arteries (white arrows)
2) The neck of the dissecting aortic aneurysm lies in the horizontal plane of the celiac trunk artery (white arrows)
02、Surgical Protocol
To avoid those complicated endovascular techniques, we planned a two-stage procedure. The first stage is the reconstruction of the aneurysm neck into a healthy landing zone followed by the second stage of standard EVAR.
03、Surgical procedures
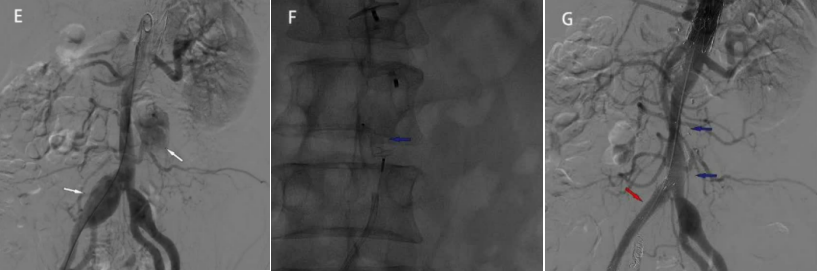
1) Intraoperatively, the contrast agent filled the false lumen of the abdominal aortic dissection (white arrow)
2), the false lumen of the abdominal aortic dissection was no longer visualized on angiography after placement of multiple AVPII (14 mm, 18 mm, 20 mm, and 22 mm) (blue arrow) and coils (red arrow).
04、Follow-up Results
1) Follow-up at 3 months after surgery showed complete thrombosis in the false lumen of abdominal aortic dissection with visible high-density AVP (blue arrow)
2) CTA reconstruction 3 months after surgery showed several AVPs (blue arrows) and complete thrombosis in the false lumen
No 2nd stage EVAR required
Case 3
A 38-year-old man underwent TEVAR 2 years ago for type B aortic dissection
01、Preoperative assessment
Preoperative CTA reconstruction showed postdissecting aortic aneurysm formation from the superior mesenteric artery to the right common iliac artery (maximum diameter approximately 52 mm) (white arrow)
02、Surgical Protocol
To avoid these complex endovascular techniques, we planned a two-stage procedure. The first stage was to reconstruct the aneurysm neck as a healthy landing zone, followed by the second stage to perform standard EVAR.
03、Surgical procedures
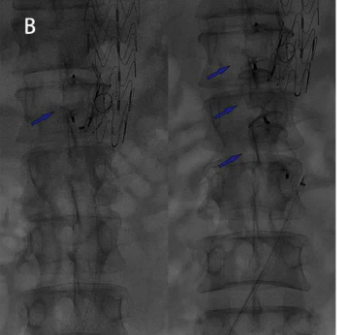
Multiple AVPII (16 mm, 20 mm, and 22 mm) were placed in the false lumen, respectively (blue arrows)
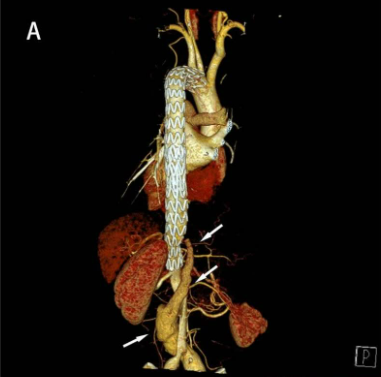
04、Follow-up Results
CTA reconstruction at 8 months showed:
1) Complete thrombosis in false lumen at renal artery level
2) The distal false lumen of the infrarenal abdominal aorta remained flowing and locally narrow. Under appropriate conditions, another embolization treatment may be possible.

05、Pre-operative Evaluation for Two Stage Procedures
Prior to the second stage of surgery, CTA showed a tear at the level of the infrarenal abdominal aorta with adequate flow in the false lumen (white arrows)
06、Two-stage surgical procedure
1) Intraoperatively, DSA showed adequate flow in the false lumen of infrarenal aortic dissection (white arrow) and aneurysmal dilatation of the right iliac artery (white arrow)
2) AVPII (8 mm − 6 mm) was placed in the infrarenal aortic region to seal the tear
3) One AVP (20 * 16 mm) was used to seal the false lumen and the other was used to seal the intimal tear (8 * 6 mm) (blue arrow) and a covered stent was inserted into the right iliac artery (10 * 80 mm flow) (red arrow)
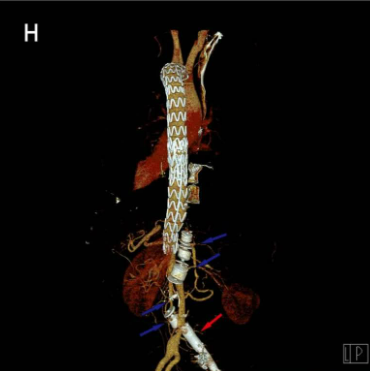
04、Follow-up Results
Follow-up CTA reconstruction at 6 months showed good thrombosis in the false lumen with multiple high-density AVP images (blue arrows) and patent right iliac artery stent flow (red arrows)
No further EVAR procedure required
Summary
Advantages:
· Relatively easy implementation
· It does not require a landing zone to avoid branch artery coverage
· Reduce aortic coverage and risk of SCI (spinal cord ischemia)
Disadvantages:
· Equipment displacement risk
· Further widening the risk of tears
· Potential for incomplete thrombosis and leakage


