
VEITH symposium is one of the most authoritative, large-scale and long-standing academic events in vascular surgery in the world. Thousands of top experts from vascular surgery, interventional radiology, interventional cardiac surgery, and other vascular surgery fields from around the world attend the VEITH symposium conference each year. Here brings together various research data updates from the world, very pioneering, prospective and controversial topic discussion, clinical technology sharing with great application value, the latest and cutting-edge medical devices and technology exploration, face-to-face communication opportunities for world-class authoritative vascular surgery experts, and so on.
The 50th Annual Symposium on Vascular and Endovascular Issues (VEITH 2023) was held at the Hilton Hotel, New York Center, USA on November 14-18, 2023. Our colleagues in vascular surgery actively attended the meeting and brought wonderful speeches. Here, we will sort out the key academic contents of VEITH 2023, and the following are the key views shared by domestic experts. Welcome to read.
Characteristics, advantages and early clinical results of C-S integrated three-branch aortic arch reconstruction system

SHU Chang
Fuwai Hospital CAMS & PUMC
1、Minimally invasive treatment is the development trend of aortic disease treatment, and the treatment of aortic disease is gradually transitioning from open surgery to hybrid and endovascular surgery.
2、Specific surgical selection of chimney, fenestration or branch stent technique should be individualized according to the anatomical and pathological characteristics of aortic lesions to develop treatment strategies.
3、Care should be taken to treat aortic arch lesions and aortic arch reconstruction should only be performed if necessary. Many studies of novel, non-customized stents for single-branch, two-branch, three-branch reconstruction on the arch are ongoing, but their safety and efficacy still need more data support.
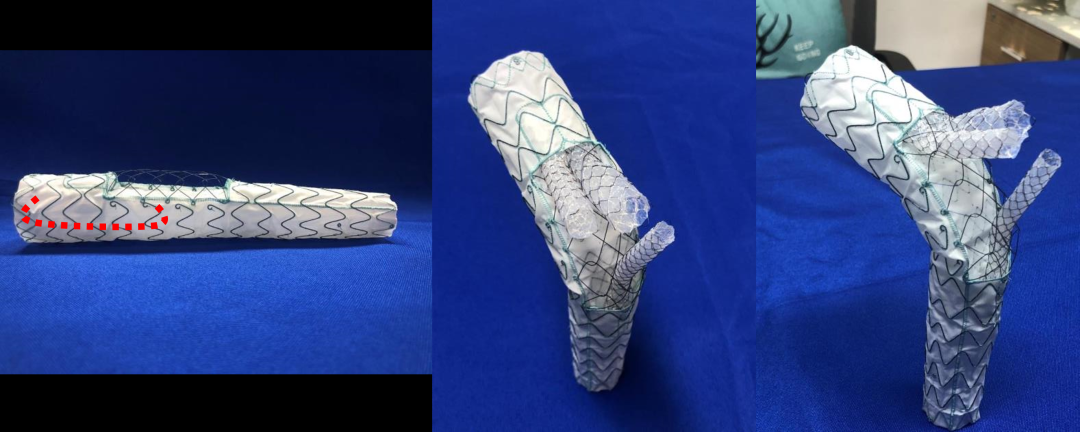
Structure of C-S Integrated Three-branch Aortic Arch System
How is carotid artery near occlusive disease defined? The best treatment for symptomatic and asymptomatic patients is conservative treatment, CEA or CAS?
Fu Guowei
Zhongshan Hospital, Fudan University
Professor Fu Weiguo 's team retrospectively analyzed the clinical data of 92 patients with CNO confirmed by DSA who underwent revascularization in a single center between January 2012 and December 2017, including 54 patients treated with CAS and 38 patients treated with CEA. Technical success was 98.1% (53/54) in the CAS group and 100% (38/38) in the CEA group. The incidence of new DWI lesions was 57.4% in the CAS group and 34.2% in the CEA group (P = 0.03). There were no ischemic strokes or TIAs in either group. Kaplane Meier survival curves showed 5-year survival rates of 85.8% in the CAS group and 82.7% in the CEA group (P = 0.61); Kaplan-Meier survival curves showed 5-year freedom from target lesion restenosis of 93.3% in the CAS group and 80.4% in the CEA group (P = 0.02).
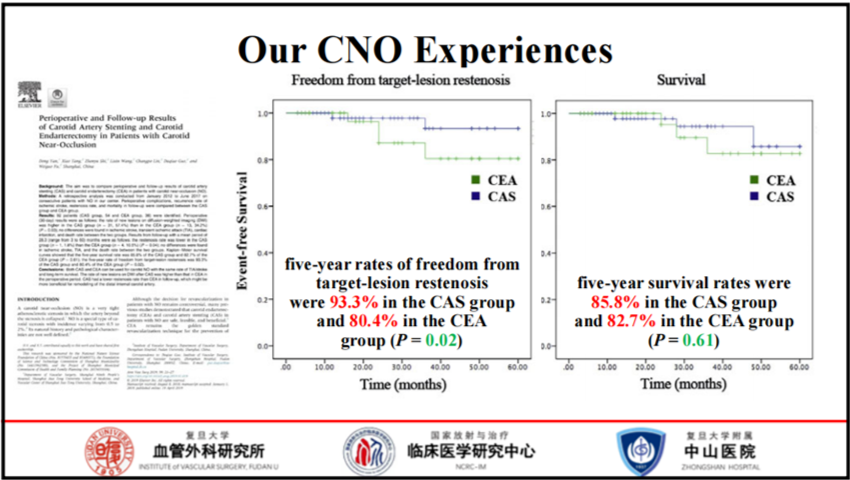
Several CNO-related meta-analyses have been published in recent years. CNO meta-analysis showed higher stroke rates in CNO patients treated with optimal medical therapy (BMT) alone, suggesting that surgery may result in better outcomes than BMT alone. BMT-treated CNO patients had nearly three times the incidence of stroke compared to CEA and CAS. The restenosis rate was higher in the CEA group than in the CAS group.
CNO is associated with the risk of recurrent stroke, but the pathophysiology and course of CNO still need further investigation. Current evidence suggests that CEA or CAS combined with BMT may be superior to BMT alone modalities in symptomatic and completely collapsed CNO patients. CNO with or without complete collapse can be treated with stent implantation with minimal risk and acceptable success rates. Homogenous stenosis throughout the distal ICA recovered spontaneously after recanalization. However, untreated tandem lesions can affect the recovery of the distal ICA and therefore require follow-up.
New Branch Reconstruction Device Family for Near Renal AAA, TAAA and Aortic Arch Repair: Principles of Operation and Excellent Results

Guo Wei
The First Medical Center of PLA General Hospital
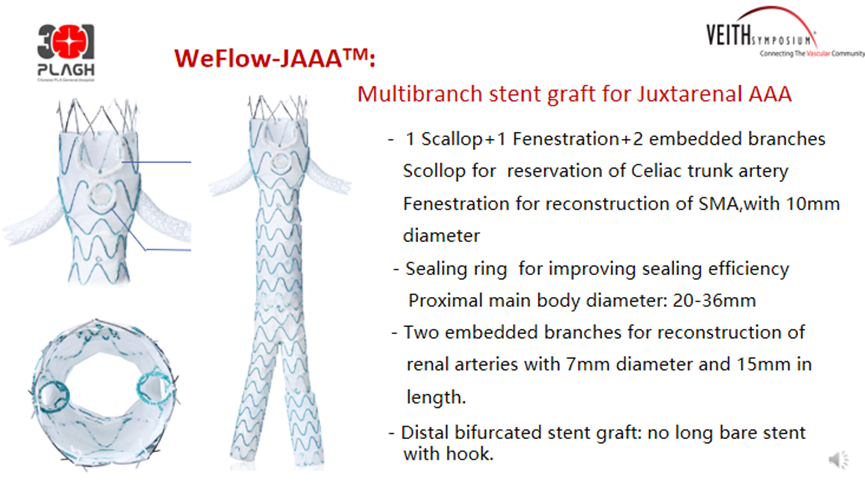
The WeFlow-JAAA ™ AAA Stent System is designed primarily for the treatment of juxtarenal abdominal aortic aneurysms. The structure includes one notch, one fenestra and two embedded branches for the reconstruction of CA, SMA and RA, respectively. Slots and window edges have sealing rings designed to prevent endoleak.
The FIM study for this product showed no Type I and Type III endoleaks at 90-day follow-up. On this basis, Professor Guo Wei 's team carried out a national multicenter clinical study, the GREAT study, in order to evaluate the efficacy of this product in the treatment of J-AAA, and plans to include 106 patients in 20 centers in China. The GREAT study was officially launched on 23 February 2022, and 106 patients have been enrolled and completed the procedure so far. Inclusion criteria Aneurysm to SMA length > = 4 mm and landing zone angulation < 60 °. Primary safety endpoint: 1 patient died within 30 days. Primary efficacy endpoint: Immediate postoperative technical success rate 98.82%. Thirty patients completed the 6-month follow-up without endoleak, 96.7% had patent target vessels, and the reintervention rate was 9.6%. Twelve patients completed the 12-month follow-up without endoleak, and 100% of target vessels were patent without reintervention.
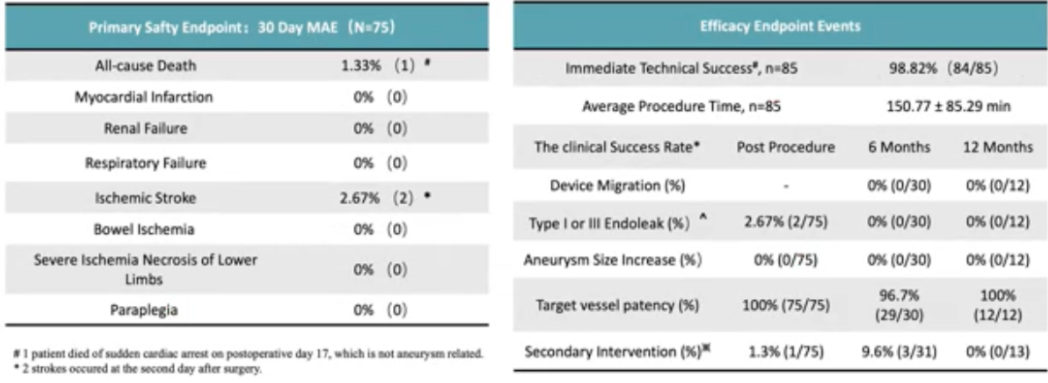
GREAT Study Safety and Efficacy Endpoints
WeFlow-Tbranch ™ is designed for reconstruction of LSA and preliminary results at 1-year follow-up demonstrate its safety and efficacy. WeFlow-BiBranch ™ is designed specifically for reconstruction of IA and LCCA and can be combined with LCCA-LSA bypass surgery if necessary. WeFlow-TriBranch ™ is designed for total endoluminal aortic arch replacement. G-Branch ™ is designed for reconstruction of four branch vessels of TAAA/PAAA. WeFlow-JAAA ™ is designed for the reconstruction of the renal arteries and SMA to address the endovascular treatment of JAAA. In the future, more cases and longer follow-up periods are needed to provide more evidence for each product.
Fibrin glue filling techniques should be routinely used in EVAR to prevent endoleaks based on the results of multicenter trials

Lu Qingsheng
First Affiliated Hospital of Navy Military Medical University
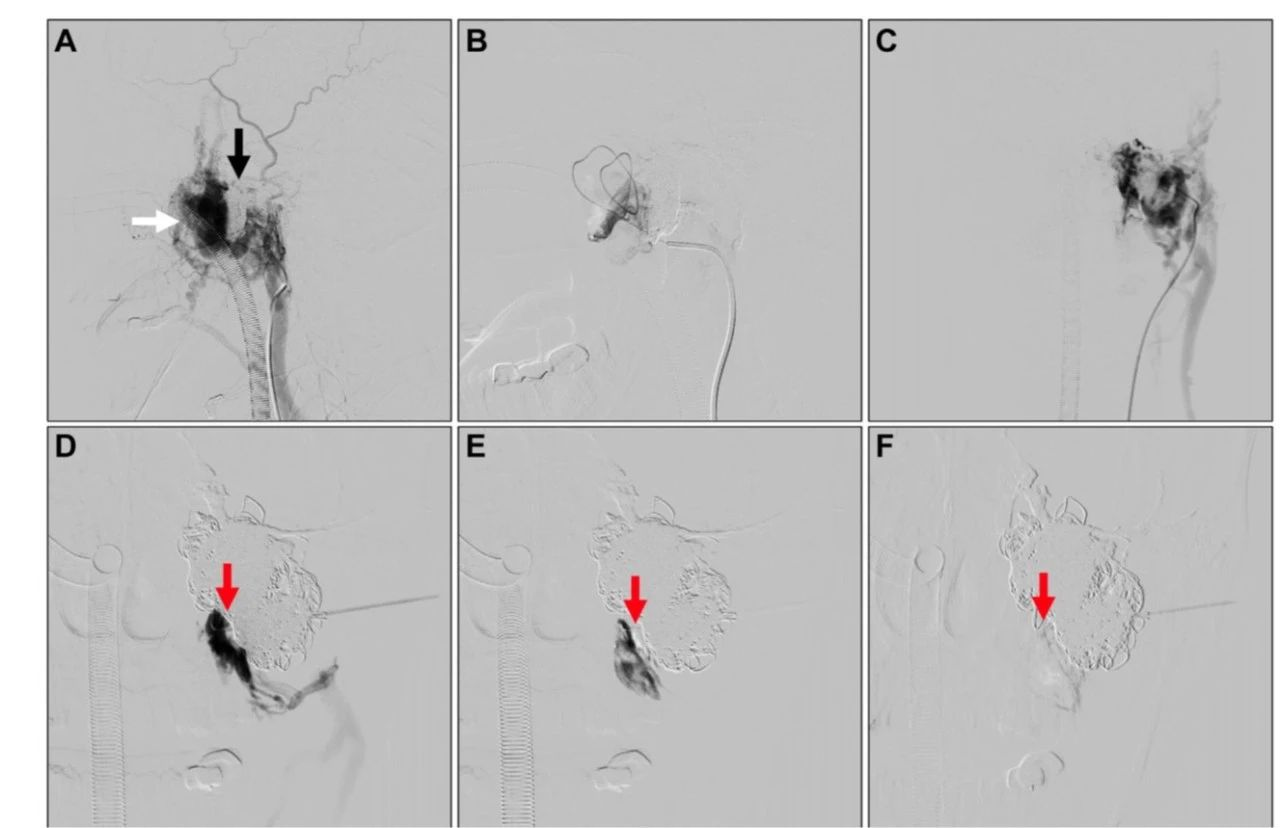
Professor Lu Qingsheng 's team conducted a trial to investigate the long-term efficacy of fibrin sealant filling the sac after EVAR for challenging abdominal aortic aneurysms, and retrospectively analyzed the challenging anatomy of the AAA proximal neck (short neck or neck angulation) who underwent traditional EVAR and received fibrin glue sac filling to solve type IA endoleak in AAA patients from December 2006 to July 2010 in Changhai Hospital. Intravascular pressure was measured with a preset catheter before and after fibrin glue filling to observe the immediate effect. The long-term outcome was assessed by annual aortic CT angiography for 7 to 10 years according to the occurrence of endoleak, maximum aneurysm diameter, all-cause mortality, and other serious complications, with a mean follow-up time of 89.1 months.
The results showed that the mean maximum aneurysm diameter was significantly reduced (53.23 ± 10.9 mm vs. 59.86 ± 11.77 mm). Maximum aneurysm diameter decreased in 76 patients and was stable in 22 (91.6%, 98/107). There was no recurrence of type I or type II endoleaks. Four patients underwent repeated endovascular treatment after distal iliac artery dilatation. Preliminary demonstrated the long-term efficacy of fibrin glue filling the sac after EVAR for challenging abdominal aortic aneurysms.
Fibrin glue filling is a simple and effective treatment. It can be used to prevent the occurrence of any type of endoleak in all EVAR procedures and improve treatment outcomes. After fibrin glue filling, thrombus can form in all aneurysm sacs immediately, and no endoleak of any type occurs after EVAR to prevent AAA rupture or exudation after EVAR and reduce peritoneal compartment syndrome. Professor Lu Qingsheng suggested using fibrin glue filling technique to prevent endoleak during all EVAR procedures.
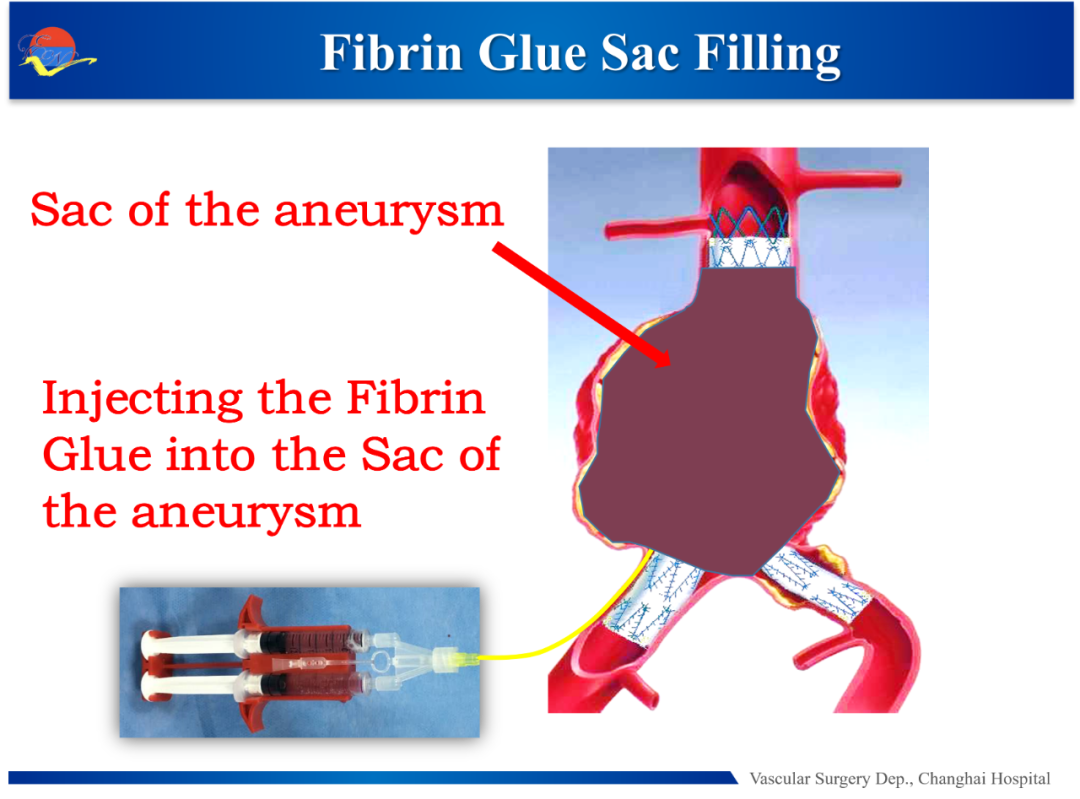
Schematic representation of fibrin glue to prevent endoleak
Percutaneous Embolization of Congenital Cervical Arteriovenous Fistula Using AVPs Device

Lu Shaoying
The First Affiliated Hospital of Xi'an Jiaotong University
The latest study by the Shanghai Ninth Hospital team published in the journal JVS-VLD evaluated the efficacy of coil-assisted ethanol embolization in the treatment of refractory head and neck arteriovenous malformations (HNAVMs) that recurred after Onyx glue treatment. Thirty-six patients with recurrent HNAVMs after Onyx glue embolization from October 2007 to October 2017 were included, 92.2% of whom received coils as an adjunct to surgery, and the final results showed that patients treated with Onyx had a 58.3% increase in recurrence-free survival at 5 years after coil-assisted ethanol embolization.
Comparison of efficacy after coil assisted ethanol embolization
AVPs device is a safe and effective method for the treatment of cervical congenital arteriovenous fistulas.



