Although there are various techniques for endovascular reconstruction of multiple branches of the aortic arch, the treatment of multiple branch lesions of the arch is still a major clinical challenge, involving many problems such as the number of partial branch reconstructions of the aortic arch and whether there are variations. On November 14, 2023, during the International Congress of Vascular and Endovascular Angiology (VEITH symposium) at the Hilton Hotel, New York Center, USA, Professor Qingsheng Lu from the First Affiliated Hospital of Navy Military Medical University (Changhai Hospital, Shanghai) shared the advantages and early clinical experience of a new device for endovascular repair of aortic arch aneurysms.

Introduction of a novel supra-arch three-branch reconstruction device
A novel three-branch thoracic aortic stent graft developed by Professor Lu Qingsheng 's team for total endovascular reconstruction of three branches on the arch, including one main stent and two branch stents. There was a total of one external branch of the IA and two internal channels on the main stent, and the soft (Flexible) stent was used for LCCA and LSA reconstruction through the internal channel (Fig.)
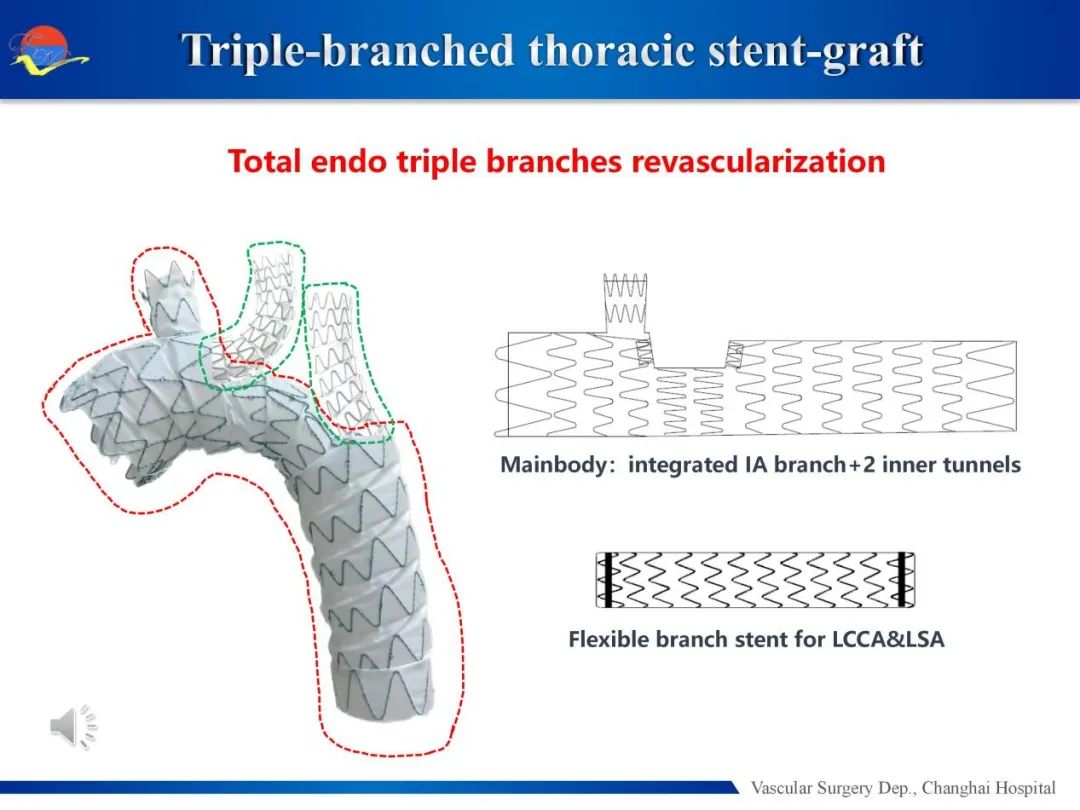
Figure 1. Schematic diagram of new three-branch thoracic aortic stent graft
Preliminary results of First-In-Human study conducted by Changhai Hospital
From December 2022 to August 2023, 11 total endoluminal aortic arch reconstructions were performed using this novel device at Changhai Hospital. Among them, there were 7 aneurysms and 4 dissections. The operative time was at least 70 minutes, with an average of 153 minutes. Technical success was 100% with no mortality or limitation of motion. No endoleak, stroke, paraplegia, branch occlusion, or RTAD occurred. Preliminary results are presented in Table 1.
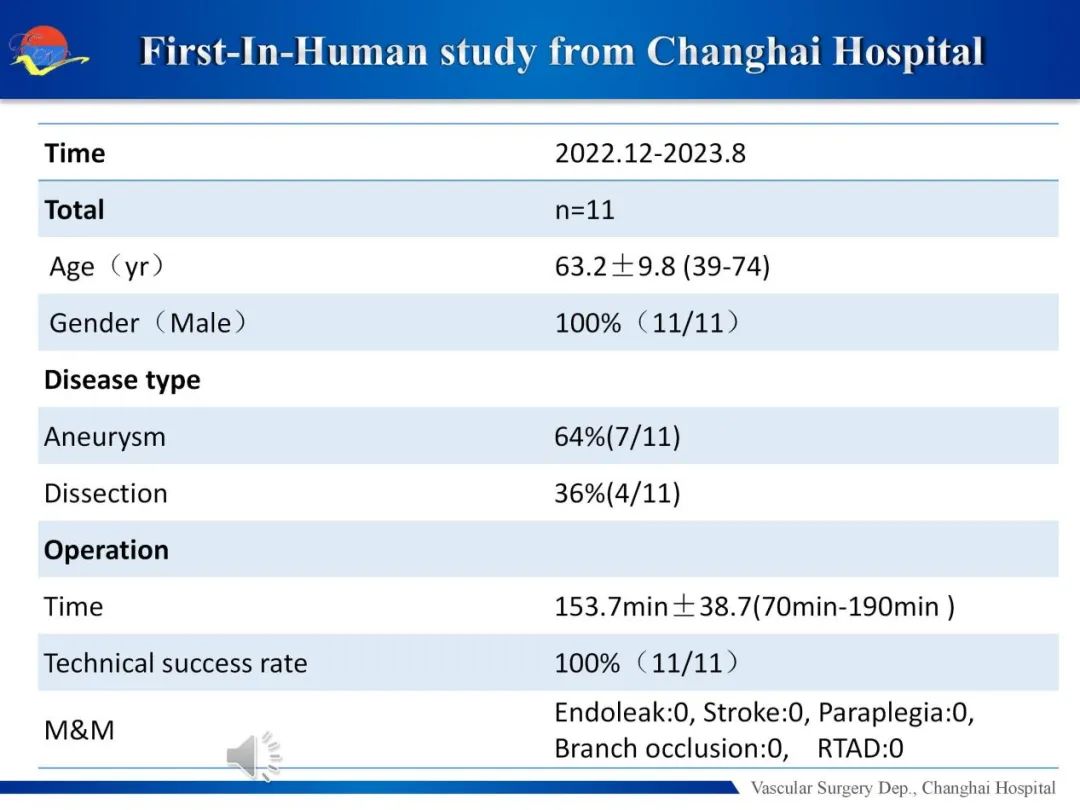
Table 1 Preliminary results of First-In-Human study
Typical case sharing
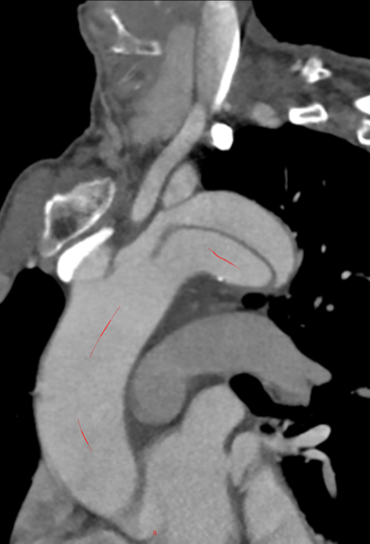
Professor Lu Qingsheng introduced the diagnosis and treatment process of a typical case of aortic arch aneurysm and dissection treated with three-branch stent:
1. patients with aortic arch aneurysm with dissection, aneurysm involving the three-branch artery, dissection from the aortic arch to the iliac artery.

2. Angiography shows that catheter access from the innominate artery to the femoral artery is established during the procedure. Introduce the stent body system over the arch with the extra stiff guidewire. The sheath was removed and a single branch was pulled into the innominate artery.

3. Quickly release the main stent after the crimped 4F catheter establishes the LSA access into the main body system.


4. From the left common carotid artery, establish a pathway to the first internal channel. The soft branch stent delivery system is then placed into the first channel, called the anterograde internal channel, and the other soft branch stent delivery system is then placed into the second channel, called the retrograde internal channel, through a guidewire already established in the LSA pathway.


5. First place the left common carotid branch stent, followed by the LSA branch stent. Both stents overlapped in the channel region greater than 10 mm.


6. Postoperative angiography showed no endoleak and the branch vessels were unobstructed. Examination of the cerebral arteries also revealed no embolism.
7. Follow-up at 6 months after operation showed no endoleak. The false lumens were thrombosed and branches were patent.

Challenging Case Sharing
Of the 11 cases enrolled in the First-In-Human study, some challenging cases were completed in addition to conventional cases.
Case 1: Mural thrombus
In a patient with type III aortic arch aneurysm, there was a large amount of mural thrombus in the aneurysm, which may lead to cerebral infarction and embolism at other sites once the mural thrombus detached during surgery.


This tribranched stent system smoothly passed through the aortic arch without affecting its release and branch position. Treatment worked well. There was no stroke or embolism.

Case 2: True Lumen Stenosis
Dissection in the aortic arch, characterized by narrowing of the true lumen in the aortic arch region. This impacts the release of the main body stent and the search for branch channels.
It has an integrated extra-innominate branch and recessed area with the main body stent, leaving room for catheterization and accommodation of separate branch stents. The operation was simple and the results were good.
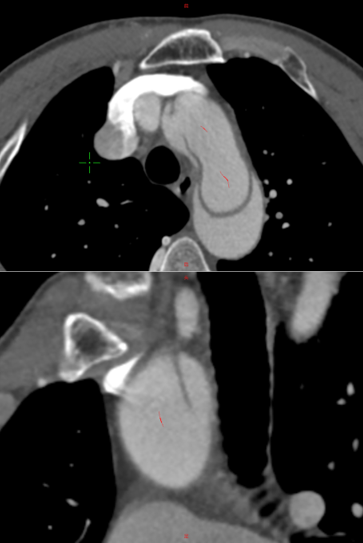
Case 3: Anatomical Variations
A patient with an aortic arch aneurysm presented with a right aortic arch, and the application of a novel tribranched endograft faced challenges.

The release method is the same as normal surgery, but the direction is opposite and needs to be adjusted. In particular, the direction of branching tests the ability and convenience of the device to adapt to different anatomical structures.


As can be seen from the final angiographic results, all branches were oriented to match the patient 's anatomy, particularly the innominate artery, with a lateral angle of nearly 90 ° and no endoleak. Follow-up showed that all branches were patent without tortuosity or tortuosity. No strokes or endoleaks.


Summary
The novel triple-branched stent graft can be used not only for endovascular repair of aortic arch aneurysms, but also for endovascular repair of aortic dissections. The unique design of integrated external branches combined with internal branches makes them more stable, avoids potential endoleaks, and reduces the incidence of stroke. The novel tribranched stent graft has special stent design and release methods that allow it to challenge some anatomically difficult cases. Preliminary results with this device are encouraging, but multicenter studies are still needed to further assess its efficacy and safety.


