On December 4, 2024, Vasco Knight@ASVS 2024 was held as scheduled at the Athenee, a Luxury Collection Hotel, Bangkok, Thailand. With the theme of "Innovation and Future", the conference brought together top experts in the field of vascular surgery from around the world, focusing on the latest treatment technologies of the aorta and abdominal aorta, the future development trend of China's medical technology, and related practical operations and innovative research and development.

Infectious primary abdominal aortic aneurysm (INAAA) is a rare but high-risk disease that is complex and challenging to manage. Open repair (OAR) and endoluminal repair (EVAR) are the main treatment options, but the short- and long-term efficacy of both is controversial. This article reviews the epidemiological features of INAAA, standardized strategies for antibiotic therapy, and compares the outcomes of OAR with EVAR with multicenter data. The study found that there was no significant difference in short-term mortality between the two methods, but there were significant differences in the reintervention patterns of IRCs and non-IRCs in long-term follow-up, which provided an important reference for clinical decision-making.
Introduction
The incidence of infectious primary abdominal aortic aneurysm (INAAA) in Asian populations is significantly higher than that in Europe and the United States, which may be related to genetic predisposition and environmental factors. Due to its complex pathological features, conventional treatment often involves high-dose antibiotics combined with open surgery. However, the widespread use of endovascular repair techniques in recent years has provided a less invasive alternative for some high-risk patients. The objective of this study is to compare the early and late effects of OAR and EVAR in the treatment of INAAA.
Materials and methods
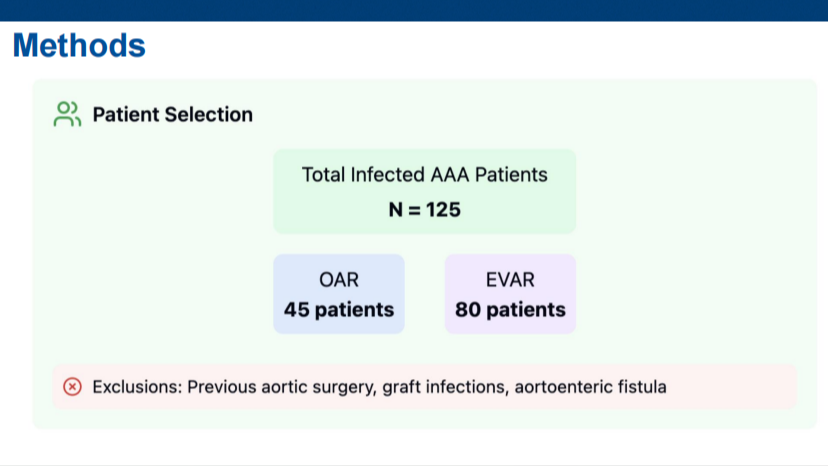
The study included 125 patients treated with INAAA between 2020 and 2023 and were based on data from a multicenter retrospective analysis.
Study subgroups:
1.Open repair (OAR): 45 cases.
2. Endovascular repair (EVAR): 80 cases.
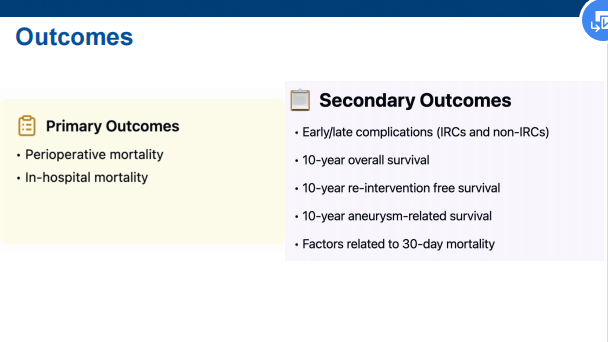
Main evaluation indicators:
1.30-day mortality.
2. Infection-related complications (IRCs).
3. Long-term survival rate.
Statistical analysis:
1.Cox regression model was used to analyze the factors related to 30-day mortality.
2. Compare reintervention models (IRCs versus non-IRCs).
Technology & Strategy
01 Standardization of antibiotic therapy
1.The positive rate of blood culture before treatment was 78.4%. Antibiotic regimens are individualized according to the bacterial species, and the duration of treatment is 6 to 12 weeks.
2. During the follow-up period, 47% of patients had their antibiotic doses adjusted due to recurrence of infection.
02 Open Repair (OAR) technology
1.Open repair remains the preferred choice for patients with complex anatomy or extensive infection.
2. Autologous venous grafts or anti-infection artificial blood vessels are often used in surgery to reduce the risk of graft infection.
03 Optimization of Endovascular Repair (EVAR) technology
1.For patients with suitable anatomical conditions, EVAR has become the first choice due to its advantages of small trauma and fast recovery.
2. Customized stent grafts improve the success rate of treatment, but put forward higher requirements for infection control.
Results & Analysis Short-term results
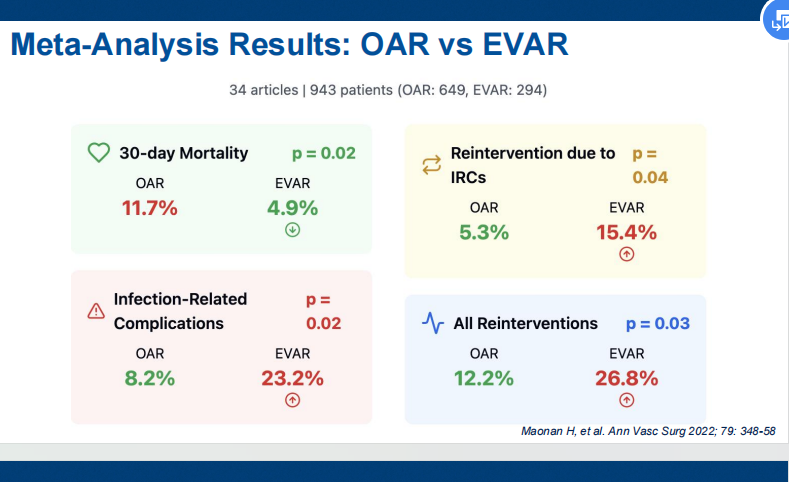
1.0-day mortality: OAR was 11.1%, EVAR was 8.8%, and the difference was not statistically significant (p=0.668).
2. Infection-related complications (IRCs): The incidence of OAR group was significantly lower than that of EVAR group (p<0.05).
Long-term follow-up results
1.10-year survival rate: 68.4% in the OAR group and 61.3% in the EVAR group.
2. Reintervention mode: The reintervention rate due to endoleak or stent-related infection in the EVAR group was significantly higher than that in the OAR group (p<0.01).
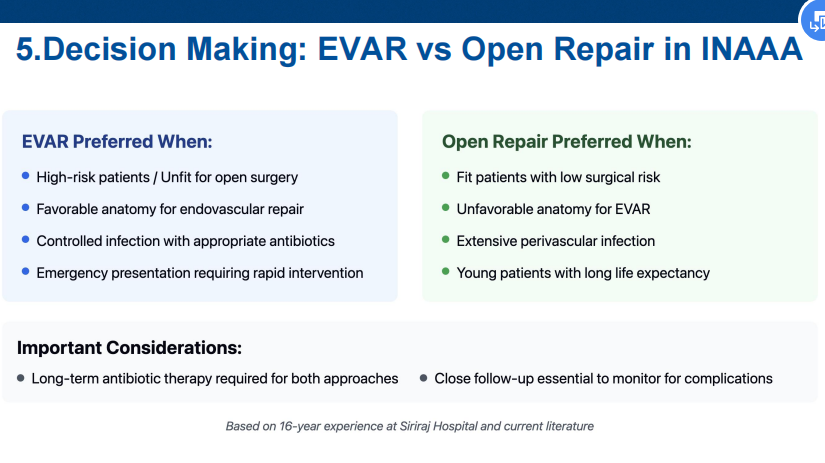
Decision-making factors
1.Anatomical conditions, overall patient status (e.g., comorbidities) are key to the choice of OAR or EVAR.
2. EVAR is indicated for elderly or critically ill patients who do not tolerate open surgery. Case analysis
Case 1: 75-year-old male, high-risk case of infection
● Background: History reveals chronic bacterial aneurysm with abdominal pain.
● Treatment: Open repair with a long course of antibiotics after surgery.
● Results: There was no recurrence 2 years after surgery, and the quality of life was significantly improved.
Case 2: 82-year-old female, elderly patient with comorbidities
● Background: Severe cardiopulmonary insufficiency is assessed as a contraindication to OAR.
● Treatment: EVAR technology was used in combination with antibiotics for 6 months.
● Results: IRCs occurred once within 5 years of postoperative follow-up, and the stent recovered well after stent repair.
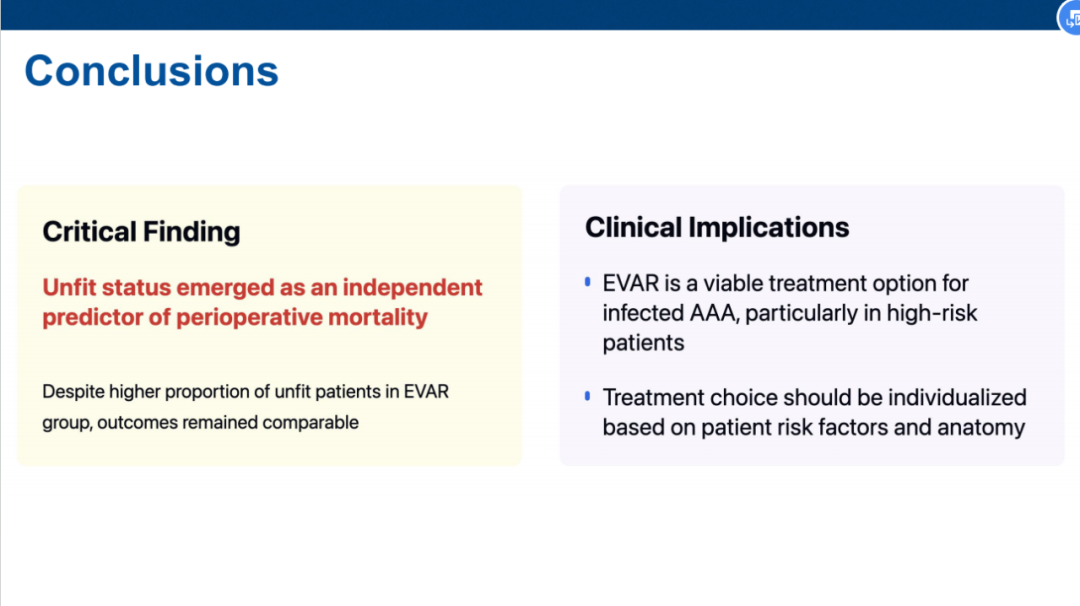
Precise treatment decisions
1.OAR and EVAR have their own advantages, and should be selected based on the specific anatomical and clinical conditions of the patient.
2. High-risk patients should pay special attention to infection-related complications when receiving EVAR treatment.
Long-term monitoring and follow-up
1. Patients undergoing EVAR should have regular imaging examinations to monitor endoleak and stent stability.
2. Strict antibiotic management is key to reducing the recurrence rate of infection.
Future research directions
1. Optimize stent design to reduce the risk of infection after EVAR.
2. Large-scale prospective studies were conducted to further validate the long-term effects of OAR and EVAR in different populations.
conclusion
The treatment of infectious primary abdominal aortic aneurysm needs to take into account the patient's characteristics and technical feasibility. Open repair and endoluminal repair are complementary in different scenarios, providing a variety of solutions for the management of complex cases. Future research should focus on optimizing technologies and improving standards to further improve treatment outcomes and patient survival.


