On December 4, 2024, Vasco Knight@ASVS 2024 was held as scheduled at the Athenee, a Luxury Collection Hotel, Bangkok, Thailand. With the theme of "Innovation and Future", the conference brought together top experts in the field of vascular surgery from around the world, focusing on the latest treatment technologies of the aorta and abdominal aorta, the future development trend of China's medical technology, and related practical operations and innovative research and development.
Abnormal anatomy of the aortic arch (eg, abnormal left arterial arch anatomy, ALVA) and non-A-non-B aortic dissection (Non-A-Non-B dissection) are complex cases in vascular surgery and are often associated with the risk of posterior circulation insufficiency. To determine the methods and effects of dislodged TEVAR (percutaneous stent therapy) combined with CS bypass (carotid artery to subclavian artery bypass) and spinal artery transposition. The analysis included 4023 patients with TEVAR, and the data suggest that this approach has significant advantages in reducing phobic complications and focusing on treatment.

Introduction
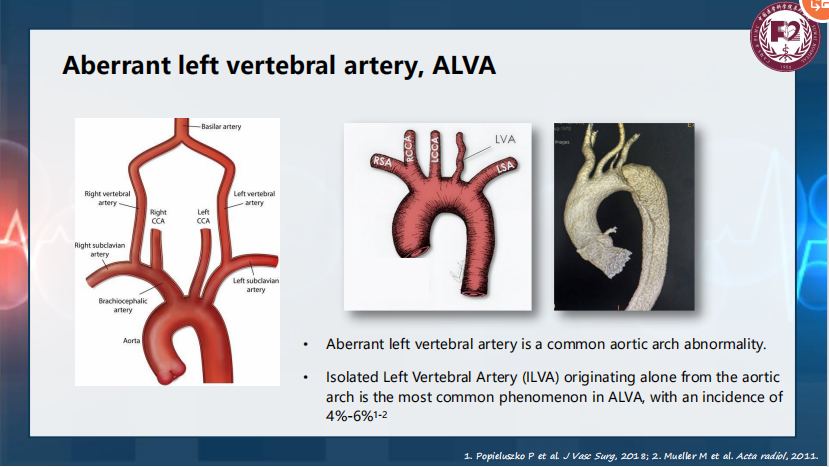
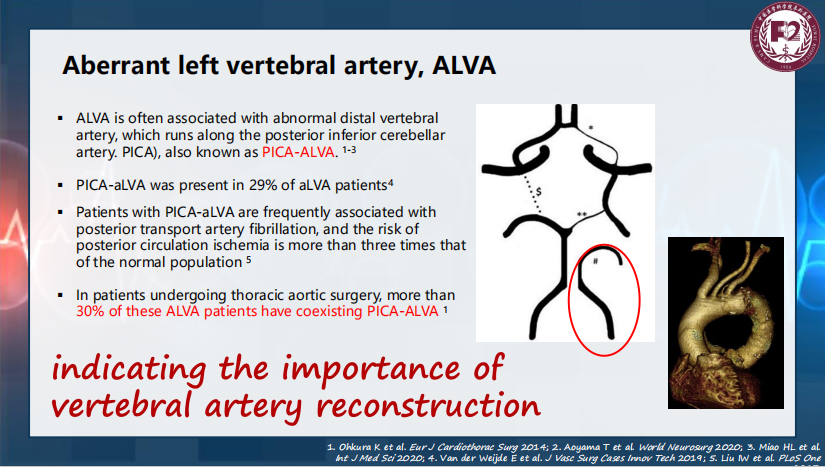
Abnormal left arterial arch (ALVA) is a common anatomical variable of the aortic arch, and isolated left arterial arch (ILVA) originates directly from the aortic arch and occurs in 4% to 6% of patients. Twenty-nine percent of these ALVA cases were combined with posterior inferior cerebellar artery-related (PICA-traditional TEVAR approach) has a technical reserve to manage these complex accidents, including disruption of blood flow due to stent coverage and high-risk complications. To overcome these problems, hybrid aortic repair (Hybrid) combines open surgery and internal stent techniques to provide an effective alternative for the treatment of complex aortic injuries.
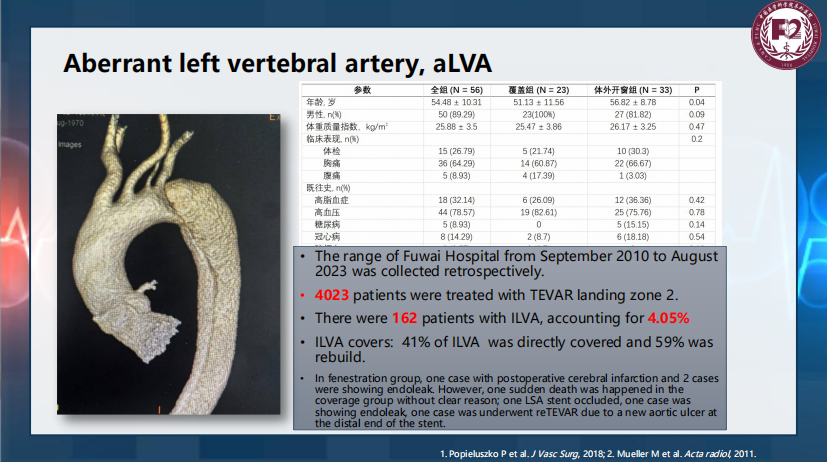
Data & Methodology Patient data
● A retrospective analysis was performed on 4023 patients treated with TEVAR in Fuwai Hospital from September 2010 to August 2023. Among them, 162 (4.05%) were ILVA patients.
● Among patients with ILVA, 41% of the disease was covered by direct stents and 59% underwent reconstruction.
● In PICA-ALVA, the risk of posterior circulation cardiovascular is three times higher than in the normal population.
Technical approach
● Disbranched TEVAR: including the CS bypass from the common carotid artery to the subclavian artery to ensure blood supply.
● Vertebral artery transposition: preserves posterior circulation, especially for patients with PICA-related injuries.
● Hybrid: Through the combination of open and stent technology, the surgical trauma and perioperative risk are reduced.
Case Study
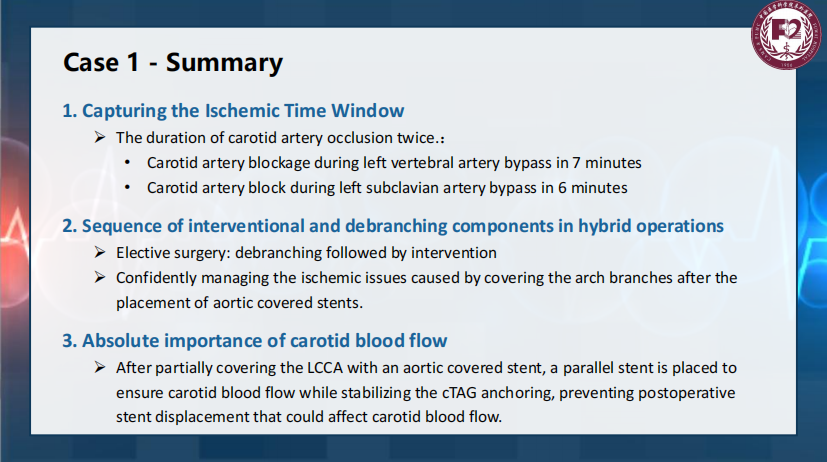
Case 1: A 41-year-old male with non-type A and non-B coarctation of the aorta with a single left artery
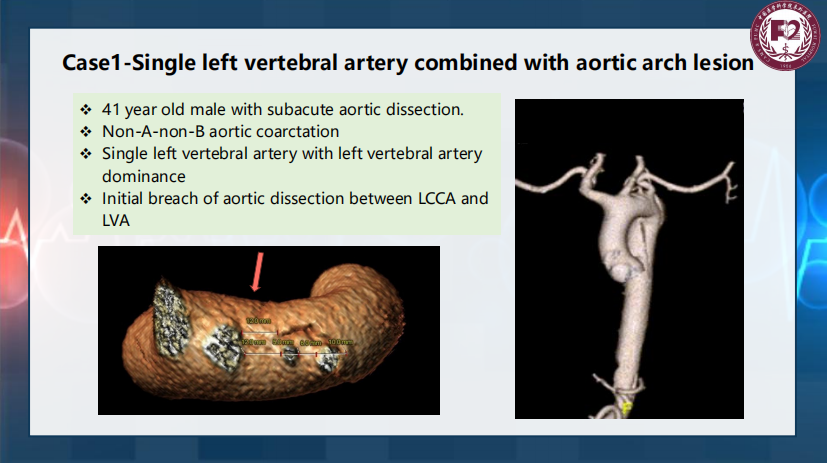
· History: subacute aortic dissection, left arterial mainstream.
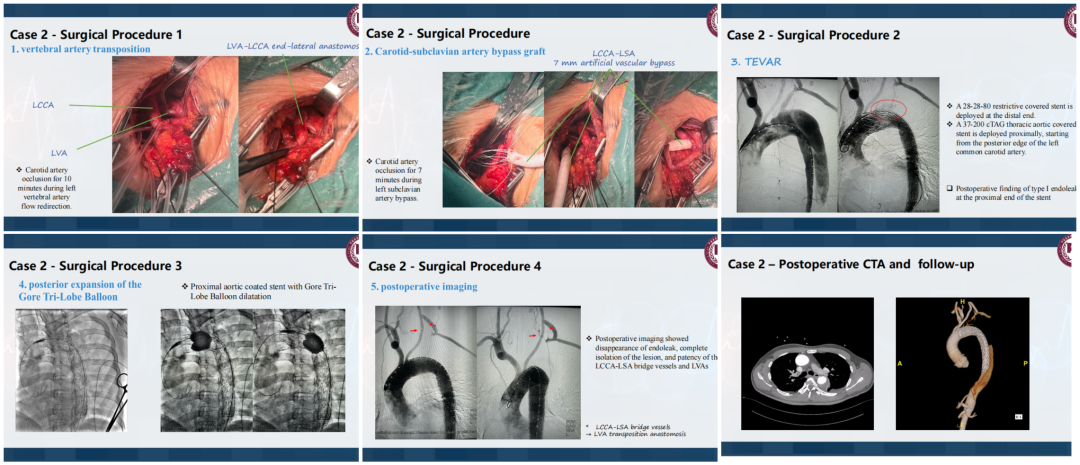
· Surgical plan: Left carotid artery transposition, left subclavian artery bypass grafting and left common carotid artery vascular stent placement were performed.
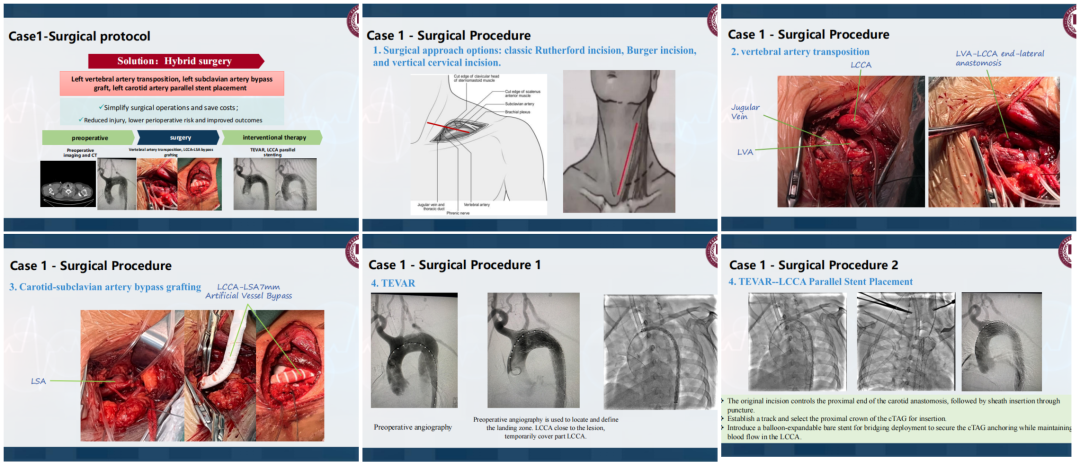
· Results: The surgical operation was simplified, and the risk and cost of complications were reduced. The patient recovered well and imaging showed patency of the blood vessels.
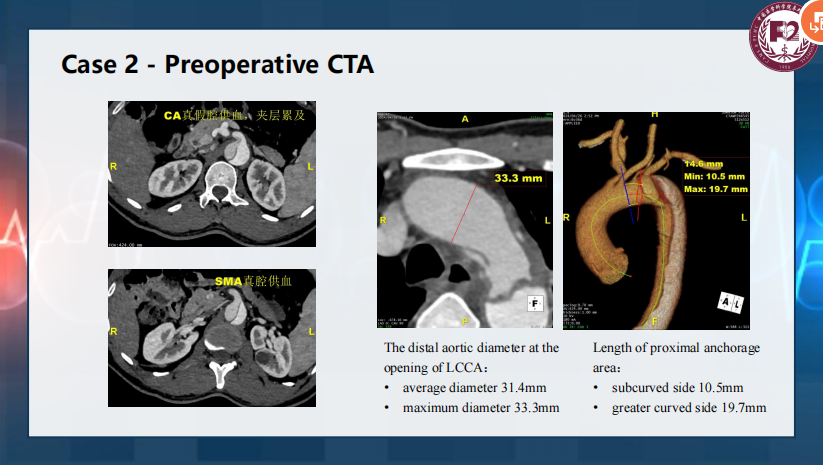
Case 2: A 47-year-old male with acute aortic dissection (Non-A-Non-B) with a single left artery dissection
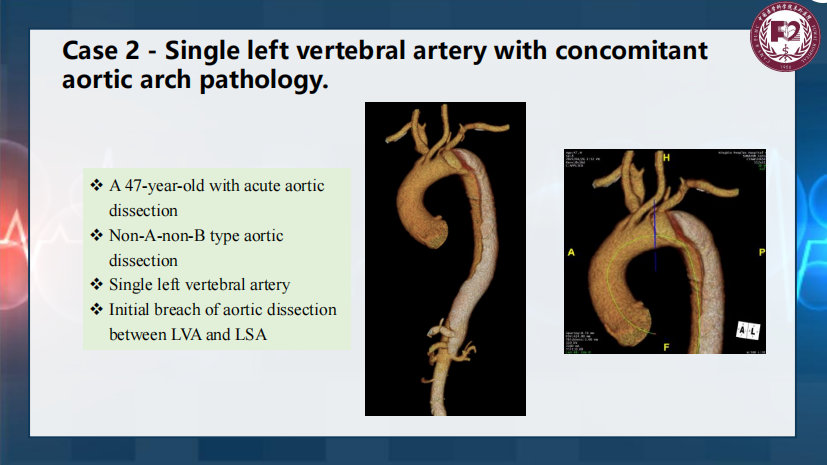
· Preoperative CTA: the proximal diameter of the left common carotid artery was 31.4 mm, and the proximal connector was defined in length from 10.5 mm (concave) to 19.7 mm (convex).
· Treatment: Treatment by LCCA-LSA artificial vascular bypass and TEVAR stent. Stent paraleakage (type I) disappeared through Gore's balloon dilatation, and the imaging showed that the lesion was isolated and the bridging vessel was patency.
Discuss
Technological advantages
● Blood flow guarantee: CS bypass and arterial transposition are performed to ensure the blood flow supply to the aortic coronary artery and posterior circulation.
● Less trauma: Compared with traditional open surgery, fusion technology reduces surgical trauma and improves the patient's perioperative safety. Challenges and limitations ● High technical difficulty: Skilled surgical techniques and accurate preoperative evaluation are required.
● Long-term pleading: Stents and bypass grafts urgently require regular vascular monitoring for patency and complications.
Data support
● 98.2% of the vascular patency of hybrid surgery after 1 year of hybrid surgery, while 4.6% of patients were reinvolved in traditional in situ fenestration.
● Hybridization significantly reduced complications, especially endoleak.

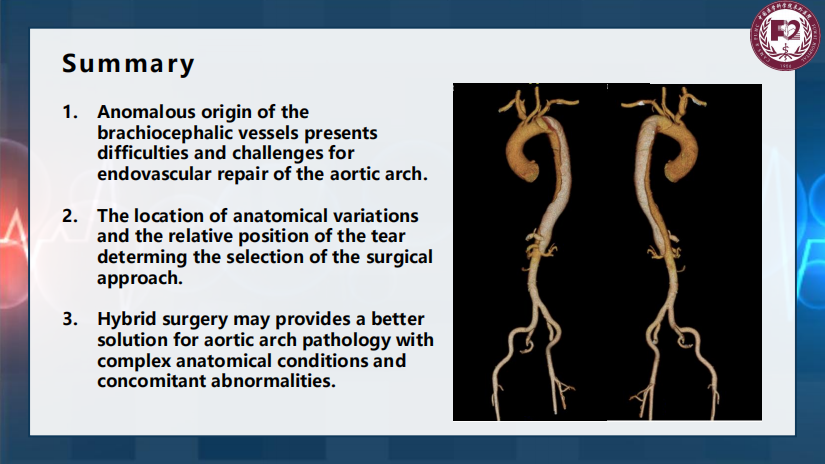
conclusion
TEVAR combined with CS bypass and coronary artery transposition is a safe and effective treatment strategy, especially for complex aortic arch disease with non-type A and non-B aortic dissection and concomitant ALVA. Clinical data suggest that this method should further optimize the surgical design and explore more personalized treatment options in future studies.