On December 4, 2024, Vasco Knight@ASVS 2024 was held as scheduled at the Athenee, a Luxury Collection Hotel, Bangkok, Thailand. With the theme of "Innovation and Future", the conference brought together top experts in the field of vascular surgery from around the world, focusing on the latest treatment technologies of the aorta and abdominal aorta, the future development trend of China's medical technology, and related practical operations and innovative research and development.

Speakers & Hospitals
Speaker: Yuehong Zheng, M.D
Institution: Department of Vascular Surgery, Peking Union Medical College Hospital
summary
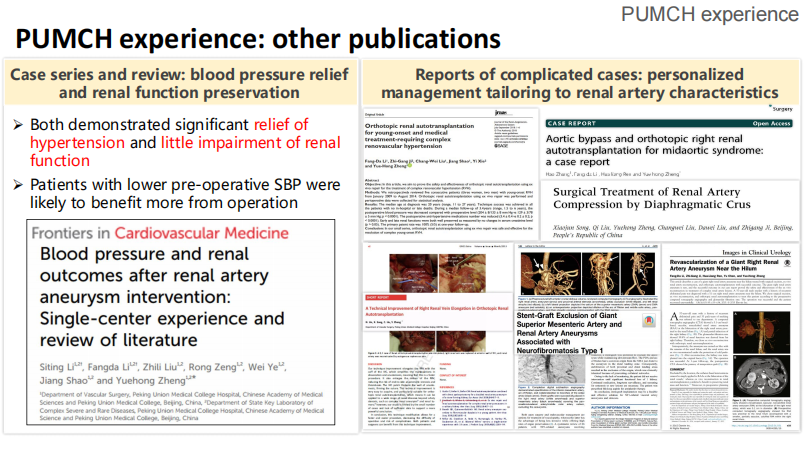
Renal artery aneurysm (RAA) is a rare but potentially fatal vascular disease whose management strategies are diverse due to anatomical complexity. In recent years, with the widespread application of endovascular repair technology and the introduction of PUMCH classification, the treatment strategy of RAA has been optimized. Based on the single-center experience of Peking Union Medical College Hospital, we discuss different treatment options for RAA, including endovascular repair and open surgery, and analyze the role of PUMCH classification in guiding surgical decisions.
introduction
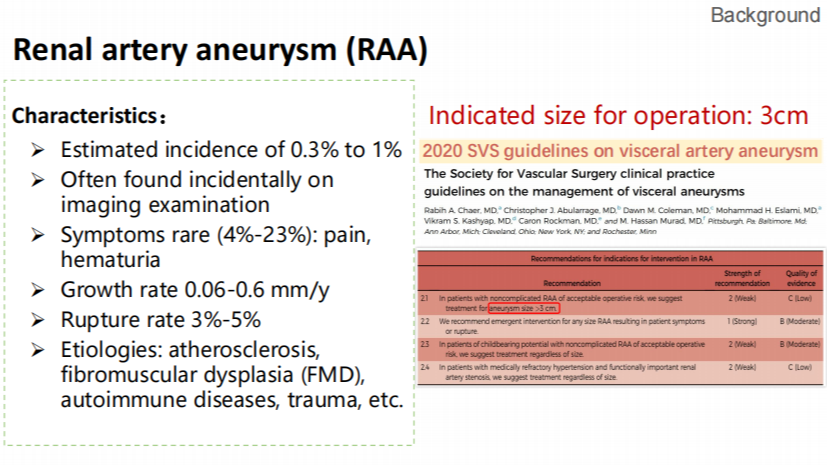
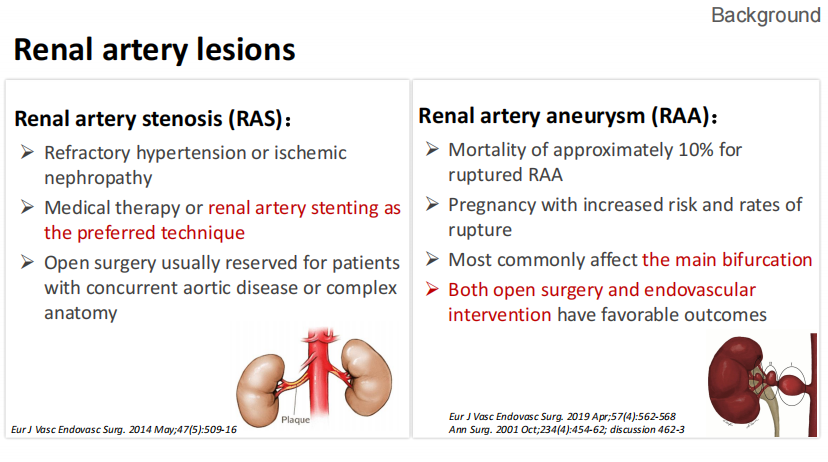
Renal artery aneurysms (RAAs) occur in about 0.3% to 1% and are usually detected incidentally on imaging tests. The proportion of symptomatic patients is low, but mortality after rupture can be as high as 10%. According to the 2020 SVS guidelines, RAAs with a diameter of more than 3 cm should be considered for surgical treatment. Endovascular repair is considered the treatment of choice due to its minimally invasive nature, but open surgery is still required in anatomically complex cases. The PUMCH classification provides more precise surgical guidance based on tumor location, neck morphology, and importance of innervating blood vessels.
Materials and methods
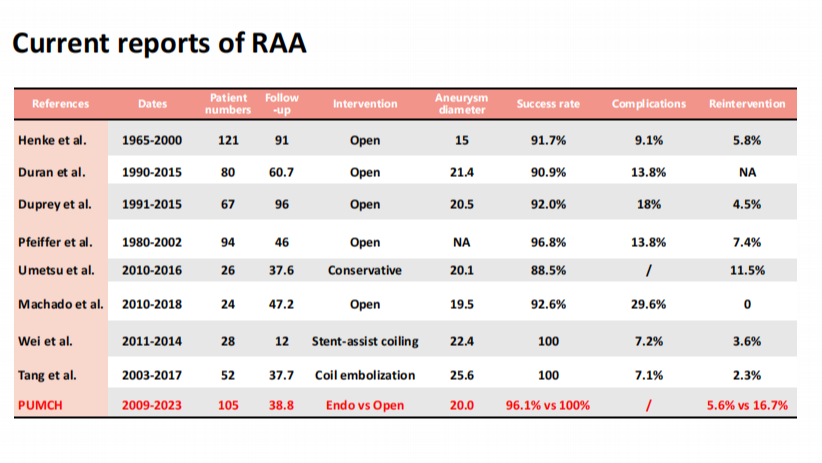
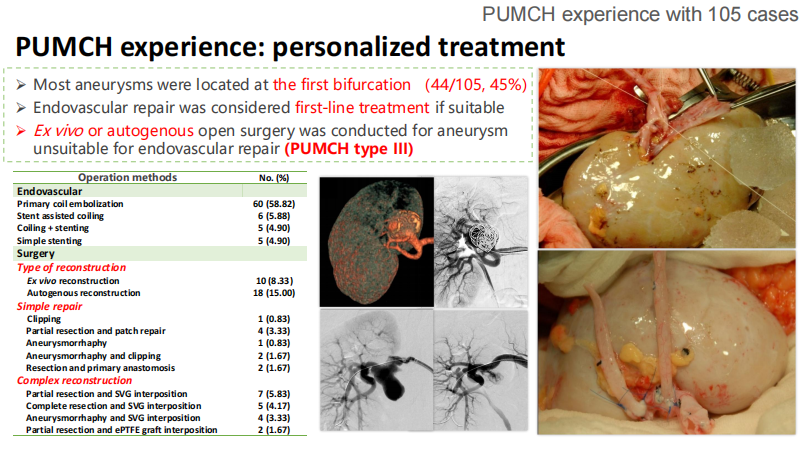
The study enrolled 105 patients with RAA who were treated at Peking Union Medical College Hospital between 2009 and 2023 with endovascular repair and open surgery.
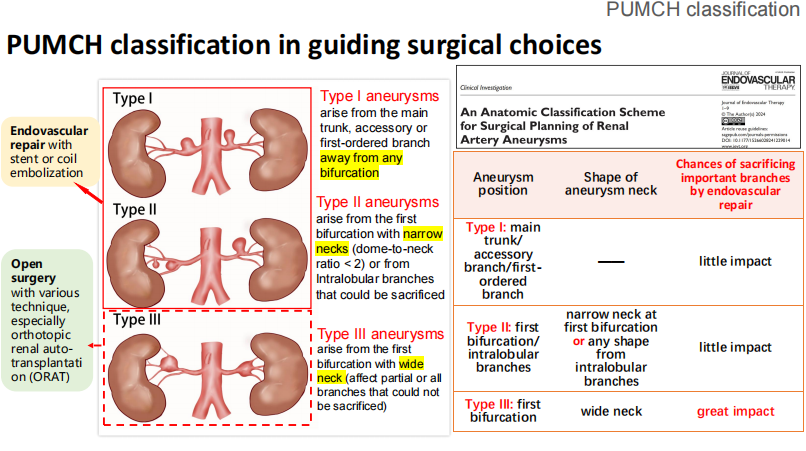
PUMCH Classification:
•Type I: The tumor is located in the trunk, accessory or primary branches, away from the bifurcation.
•Type II: The tumor is located at a primary bifurcation with a narrow neck, or in a sacrificial branch.
•Type III: The tumor is located at the primary bifurcation and has a wide neck, affecting the major branches.
Main evaluation indicators:
•Surgical success rate.
•Complication rate.
•Reintervention rate and long-term renal function.
Technology & Strategy
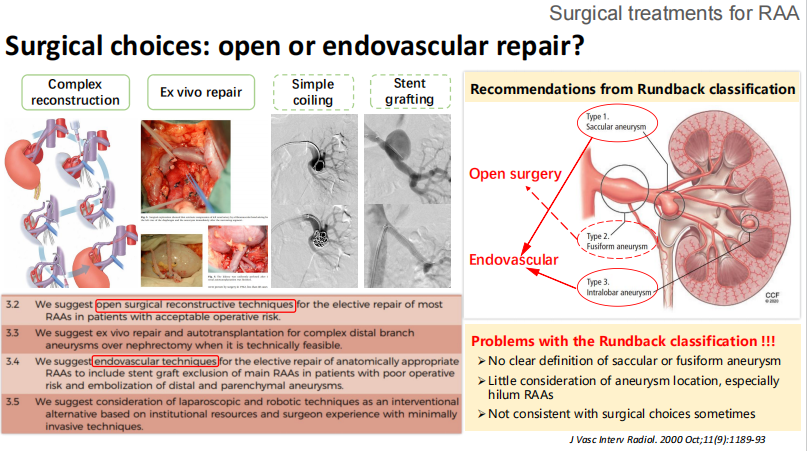
Endovascular Repair:
For type I and partial type II tumors with simple anatomy, endoluminal repair is preferred.
•Precise positioning and evaluation using stent or coil embolization techniques combined with intraoperative cone beam CTA (CBCTA).
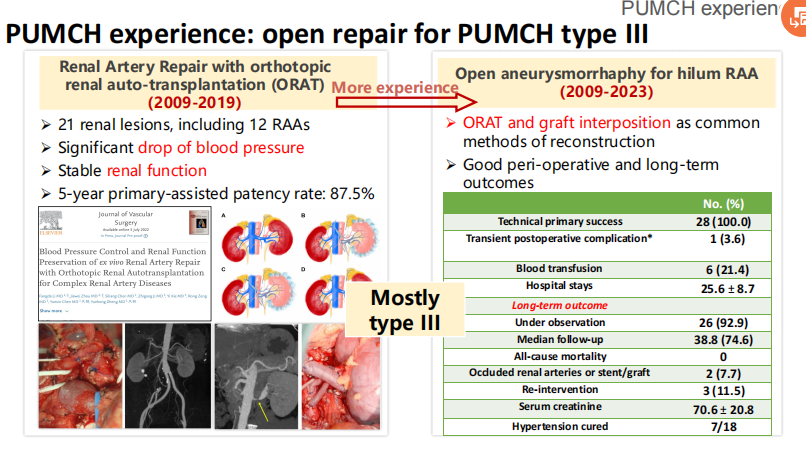
Open Repair:
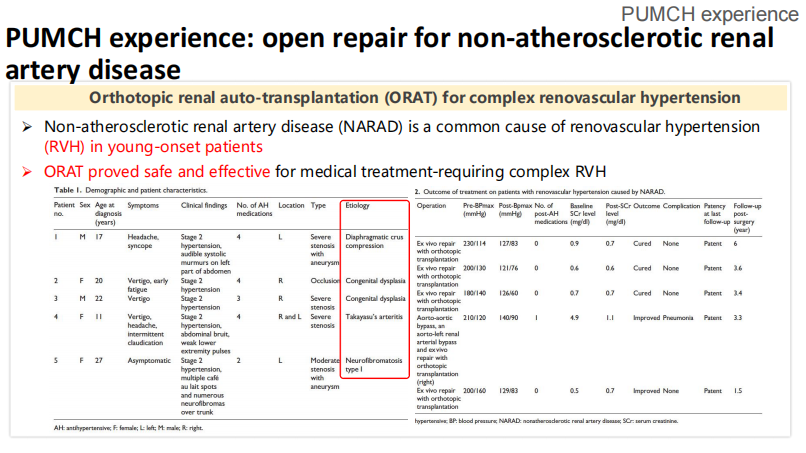
Open surgery is used for type III tumors or cases where endovascular repair is not available.
Commonly used techniques include tumor resection and autologous vein graft reconstruction, with ectopic kidney transplantation (ORAT) if necessary.
Individualized Treatment:
•Select the appropriate treatment strategy according to the patient's anatomical characteristics and PUMCH classification.
•Hybrid techniques are used in complex cases to balance trauma and efficacy.
Case sharing
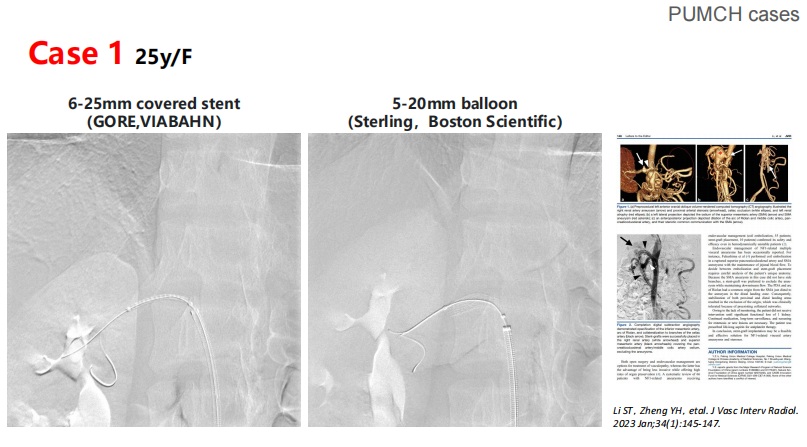
CASE 1: A 25-year-old female with PUMCH type I
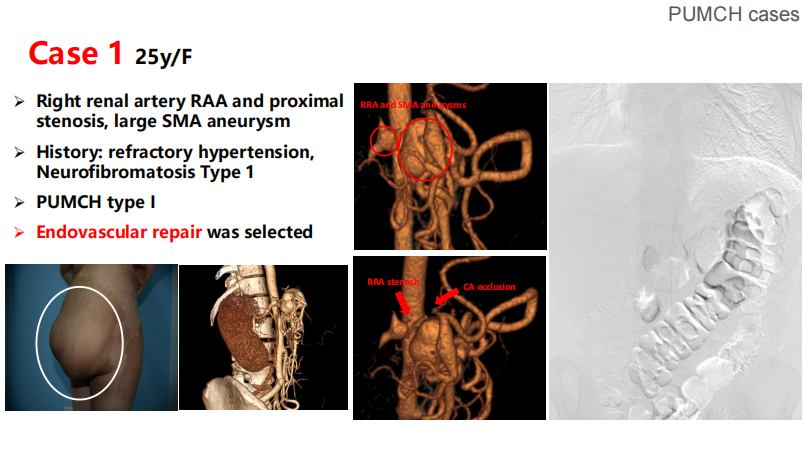
Diagnosis: right renal artery aneurysm with hypertension.
TREATMENT: ENDOLUMINAL REPAIR WITH A COVERED STENT (GORE VIABAHN) AND BALLOON DILATION.
Results: Postoperative imaging showed tumor occlusion without complications.
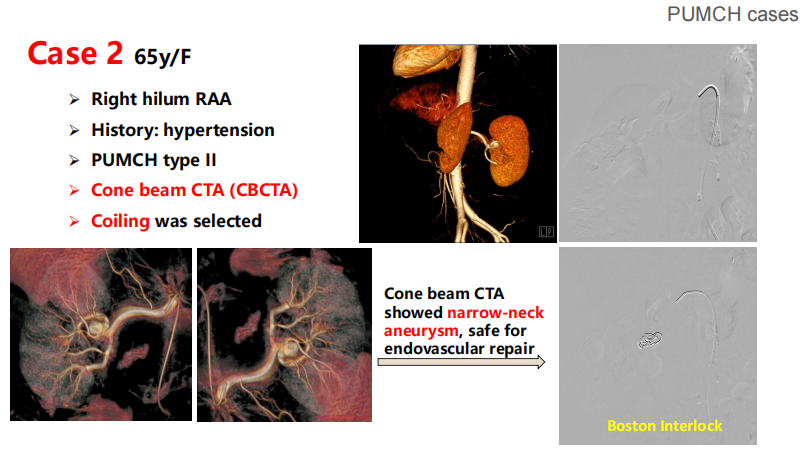
Case 2: A 65-year-old female with PUMCH type II
Diagnosis: narrow carotid artery aneurysm at the right hilum.
Treatment: Endovascular repair by coil embolization technique.
Results: Postoperative follow-up showed that blood pressure was well controlled, and there was no need for further intervention.
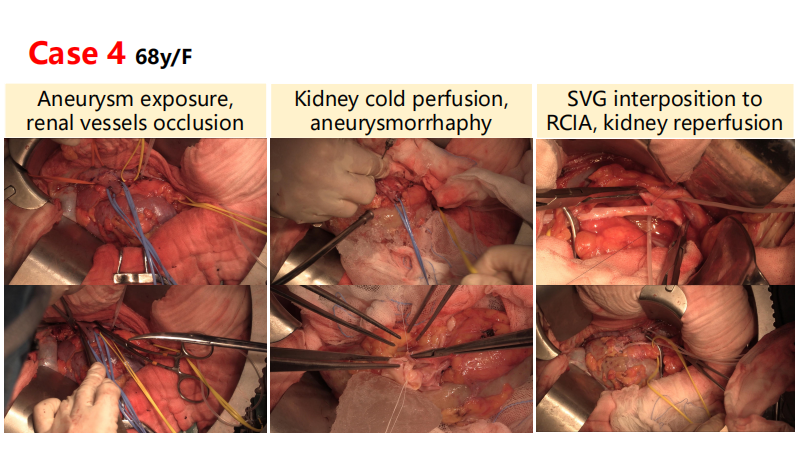
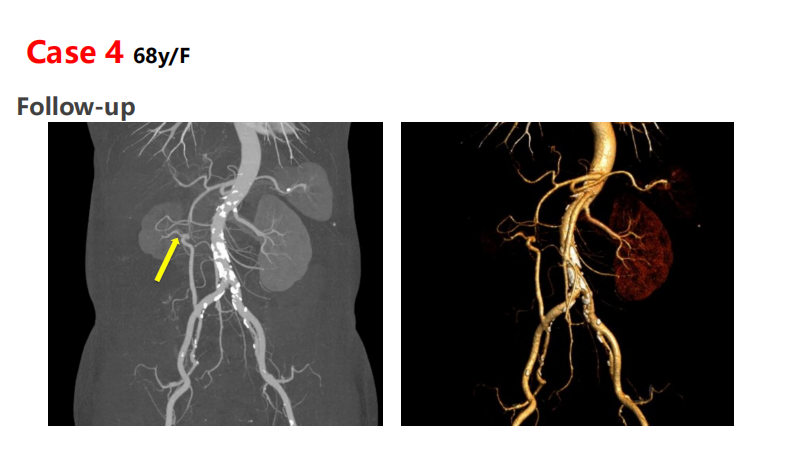
Case 3: 68-year-old female, PUMCH type III
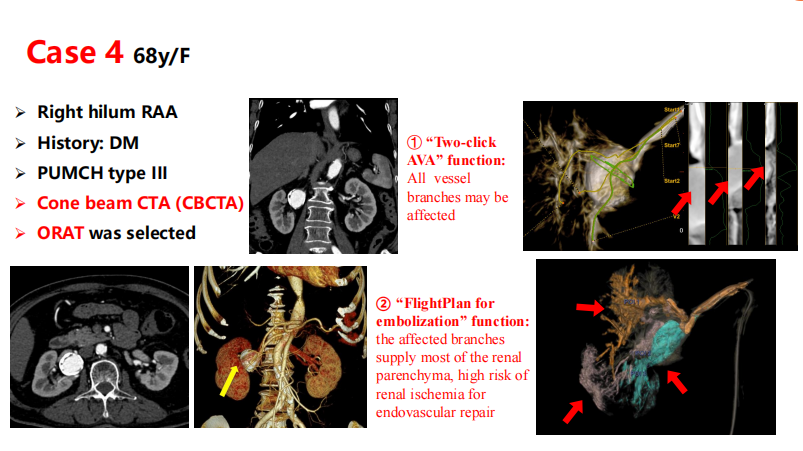
Diagnosis: hilar wide carotid aneurysm, affecting major branches.
Treatment: Open surgery with the ORAT technique to reconstruct the renal artery.
Results: After 38 months of follow-up, renal function was stable.
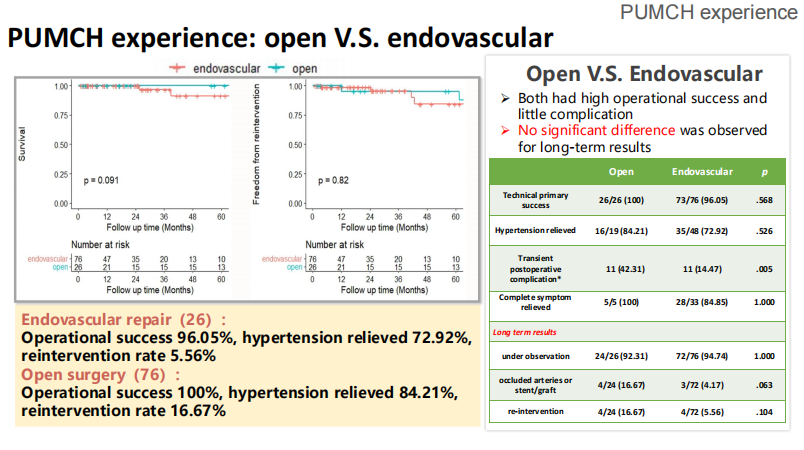
Results & Analysis
Surgical success rate:
•Endovascular repair: 96.05%.
•Open surgery: 100%.
Complication:
The postoperative complication rate of open surgery (42.31%) was significantly higher than that of endovascular repair (14.47%, P<0.01).<>
Long-term follow-up:
There was no significant difference in long-term renal function and reintervention rate between the two groups (P>0.05).
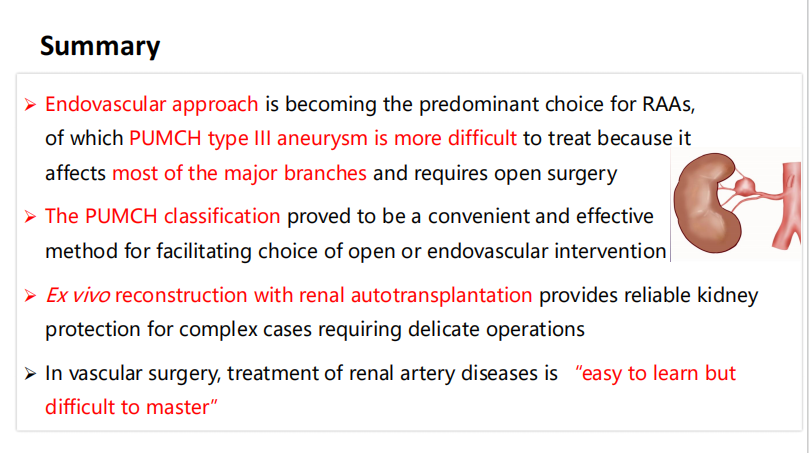
Summary and outlook
Precision treatment strategy: The PUMCH classification provides clear guidance for treatment decisions for renal aneurysms, and endovascular repair is suitable for the vast majority of type I and II aneurysms, while type III aneurysms require open surgery.
Multidisciplinary collaboration: Through the collaboration of imaging, vascular surgery, and anesthesia teams, the success rate of complex cases is further improved.
Future Research Directions:
•Develop more efficient endovascular devices to reduce the difficulty of treatment of type III tumors.
•Conduct large-scale, multi-center studies to validate the broad applicability of the PUMCH classification.
Conclusion
The treatment of renal aneurysm should be individualized based on the anatomical characteristics of patients and the classification of PUMCH. The widespread use of endovascular repair techniques has significantly improved the treatment effect, but it is still necessary to combine open surgery in complex cases. Future technological advancements and classification optimization will further drive this area.