Author: Prof. Dr. Houman Jalaie
Institution: Department of Vascular and Endovascular Surgery, European Venous Center, University Hospital Aachen, Germany
Summary
This presentation discusses the pathophysiology, diagnostic methods, and timing for reintervention in cases of in-stent restenosis (ISR) in venous stents. Through various case studies, the author demonstrates how ultrasound and other imaging techniques are used for dynamic monitoring of ISR, determining reintervention strategies based on the patient’s symptoms and disease progression. The research emphasizes that reintervention should be guided by symptoms and disease progression, rather than imaging data alone.

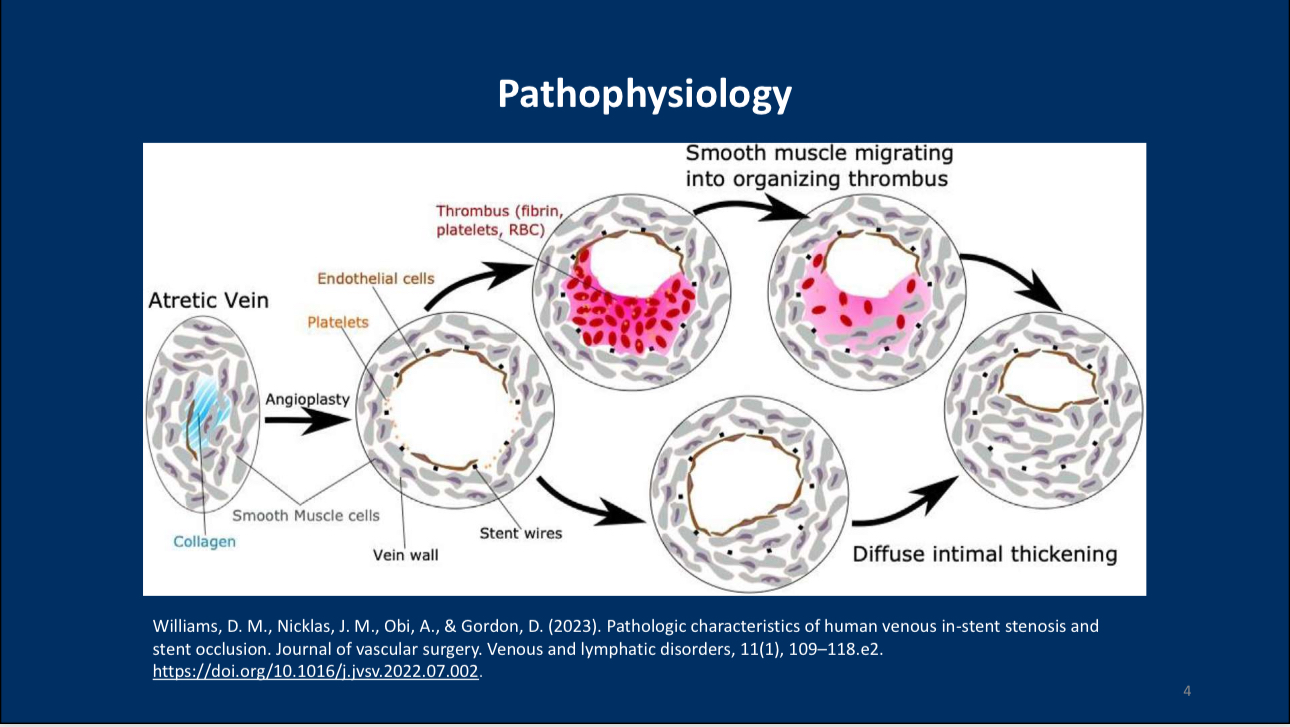
Pathophysiology
• Mechanisms of ISR Formation: Early ISR is typically dominated by fresh thrombi, while late ISR is characterized by neointima, smooth muscle cells, and fibrosis. These tissue changes lead to dense fibrous buildup around the stent, obstructing venous blood flow.

Diagnosis and Intervention Criteria
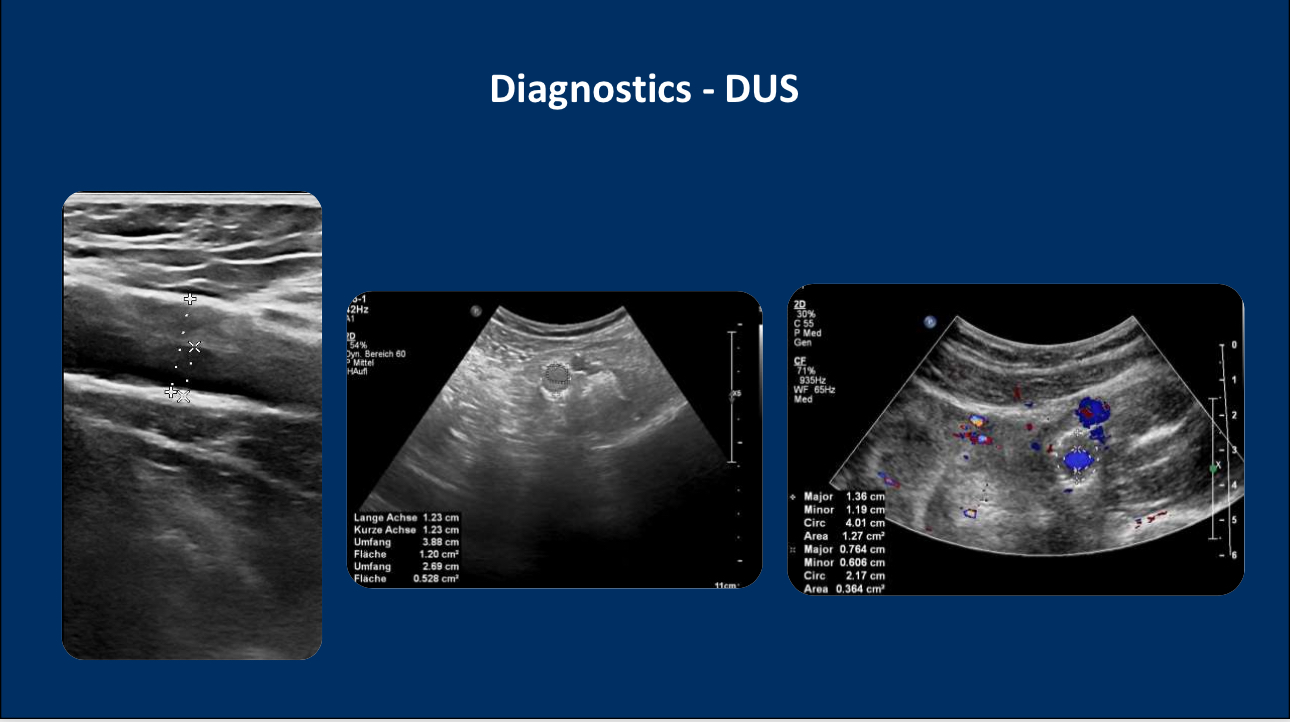
• Application of Ultrasound Diagnosis: Doppler ultrasound (DUS) is a fundamental tool for detecting ISR changes, accurately monitoring blood flow within the stent and the dynamic progression of luminal narrowing.
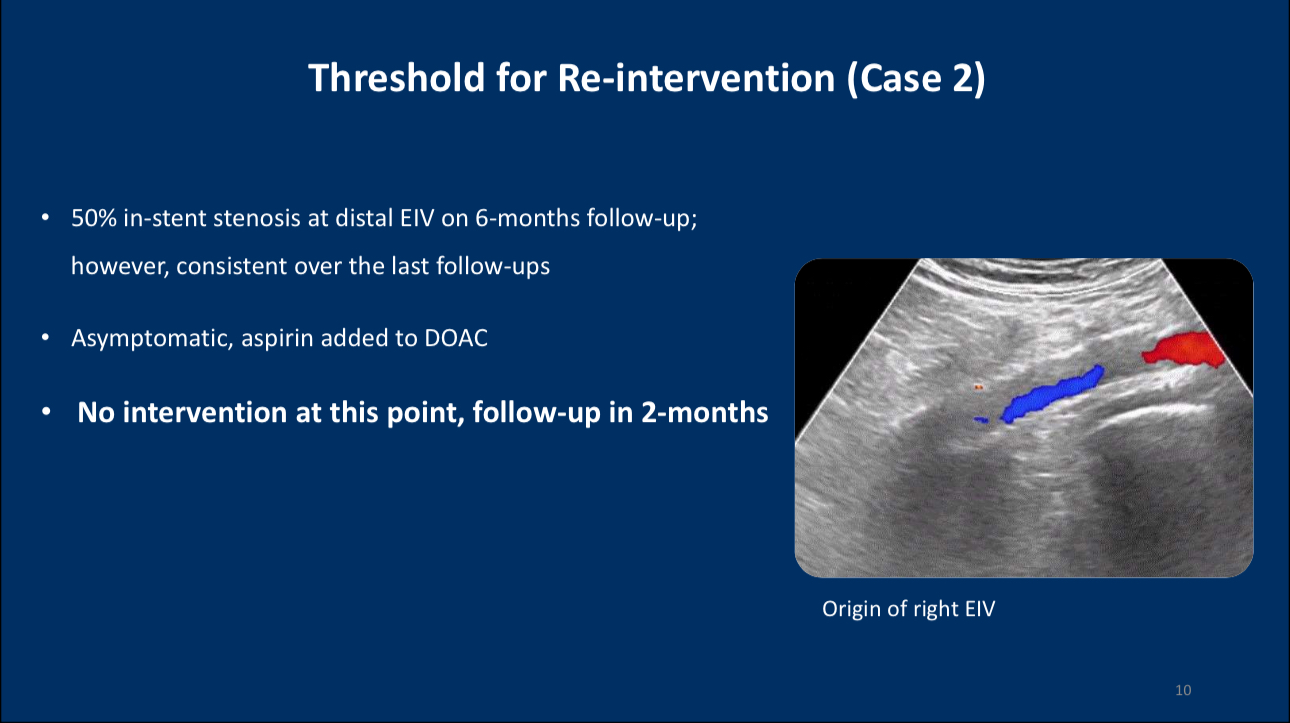
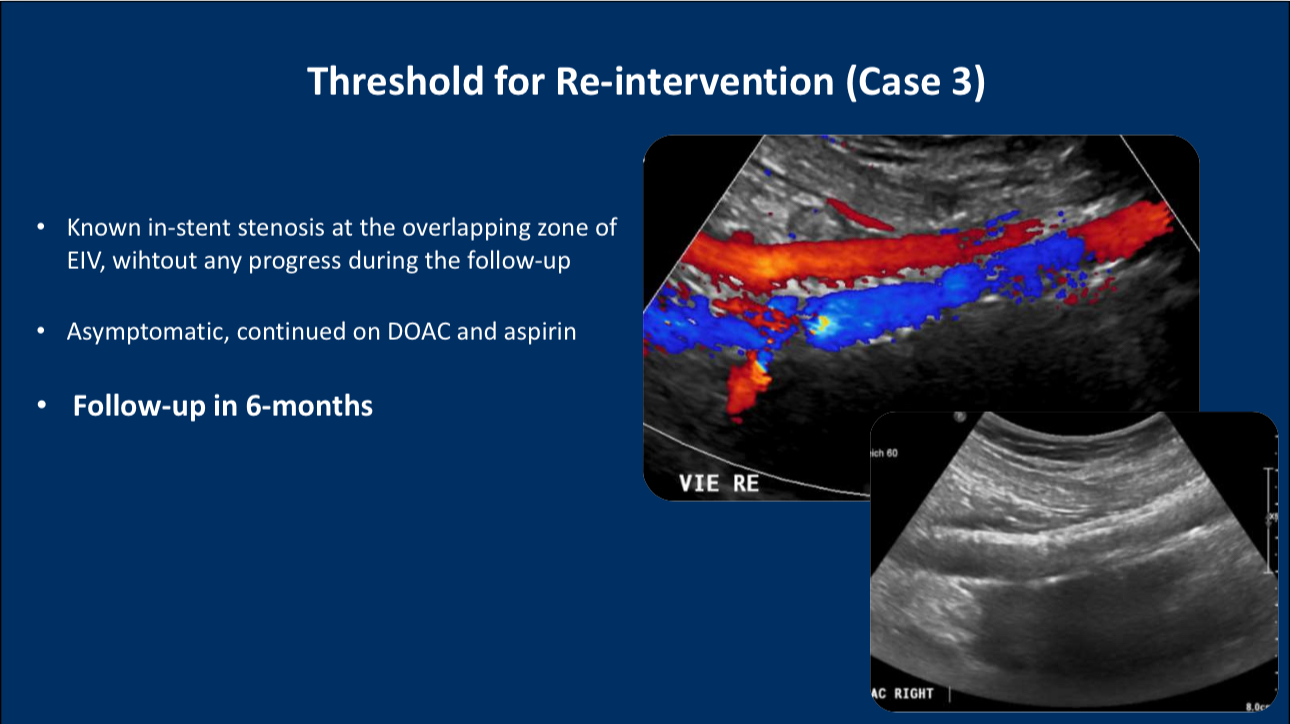
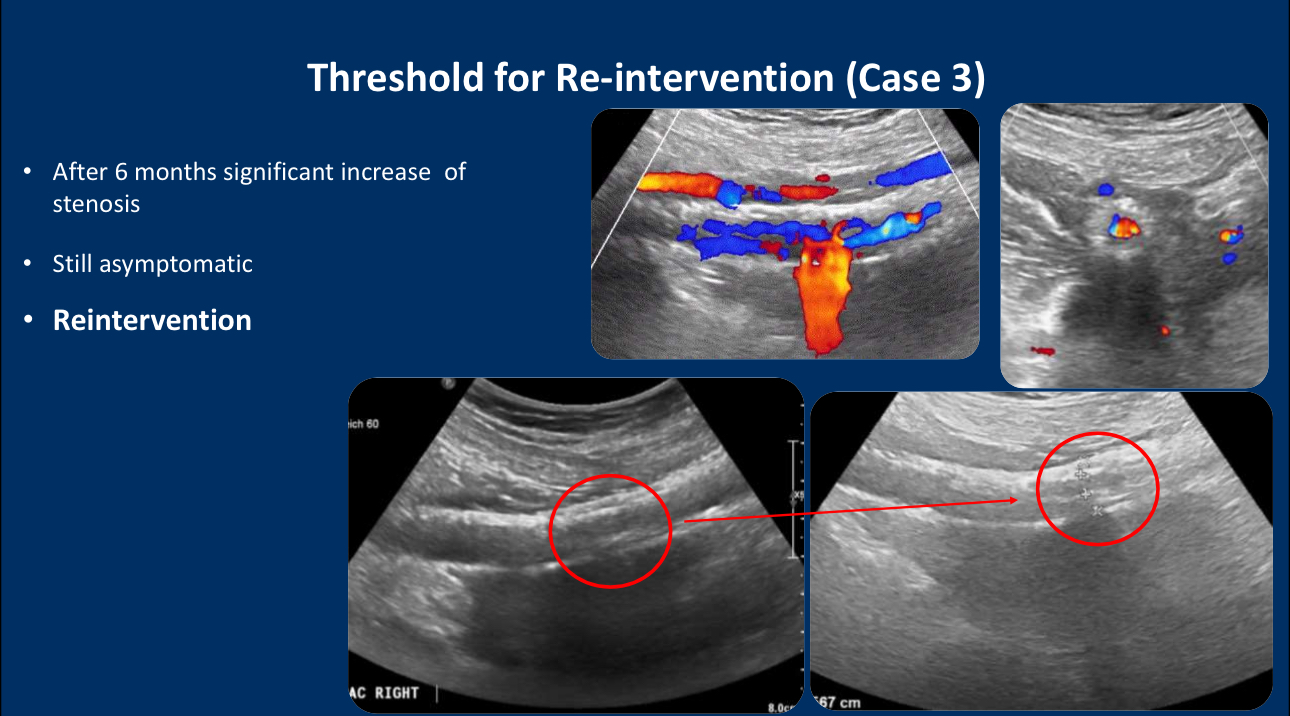
•Timing of Reintervention: Reintervention should not be based solely on the degree of stenosis observed in imaging but should consider the patient’s symptoms and disease progression. For instance, asymptomatic cases with stable stenosis may warrant regular follow-up, whereas early reintervention should be considered for cases with progressive disease and symptom onset.
Case Studies
• Case 1: Asymptomatic In-Stent Stenosis: In one patient, in-stent stenosis remained stable at 50% during a 6-month follow-up, with no symptoms. The recommendation was to continue oral anticoagulation therapy and schedule regular follow-up every two months.
• Case 2: Symptomatic In-Stent Stenosis: Another patient exhibited significant stenosis progression and symptoms after 6 months of follow-up in the left iliac vein. High-pressure balloon angioplasty was performed, and post-operative ultrasound showed restored blood flow.
Conclusion
1. Decisions for reintervention should be based on patient symptoms and disease progression rather than relying solely on imaging data.
2. Ultrasound is highly accurate in monitoring in-stent stenosis changes and should be the primary tool used during follow-up.
3. For high-risk post-thrombotic patients, anticoagulation therapy can prevent ISR; however, in cases of early thrombus formation, adding antiplatelet therapy may be an effective strategy.
References
1. Williams, D. M., Nicklas, J. M., Obi, A., & Gordon, D. (2023). Pathologic characteristics of human venous in-stent stenosis and stent occlusion. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 11(1), 109–118.e2. https://doi.org/10.1016/j.jvsv.2022.07.002
Contact Us
• Email: endovascluar@simtomax.cn
More international information available at:
• Facebook: Vasco Knight
• Instagram: knight_vasco
Let’s safeguard health together and showcase your brilliance to the world!


