Presenter: Professor Oliver Schlager
Hospital: Division of Angiology, Medical University of Vienna
Abstract
This article analyzes key challenges in May-Thurner syndrome (MTS) management, emphasizing IVUS-guided decision-making and evidence-based application of Zilver Vena stent for iliofemoral obstruction. Data-driven strategies address venous outflow pathology.
Introduction
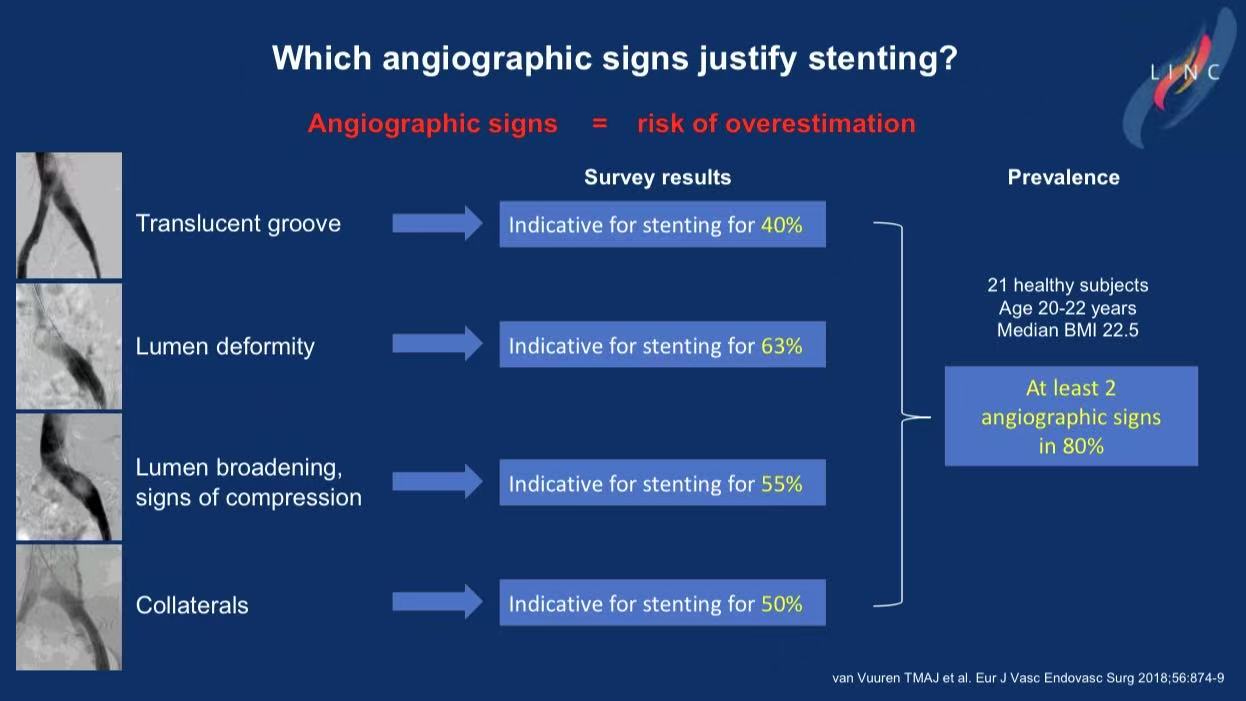
"Angiographic signs cause overtreatment: 63% of physicians misinterpret venous grooves in healthy youth as stenosis." (van Vuuren et al. 2018)
Prof. Schlager warns: MTS/NIVL diagnosis requires moving beyond traditional imaging—
31.4% of asymptomatic individuals have iliac compression (Murtha 2024)
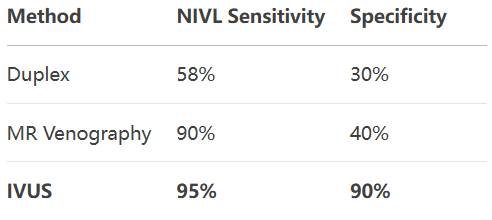
Duplex sensitivity for NIVL is only 58% (IVUS as gold standard)
Stenting demands strict criteria: >50% stenosis + symptoms
Research Insights: Three Critical Challenges
1.Diagnostic Pitfalls
High false-positive rate: 80% of healthy youth show "compression signs" (angiography)
Imaging accuracy comparison:
ESVS Guideline: IVUS-guided intervention (Class IIa)
2.Symptom-Stenosis Mismatch
37% of CEAP C5/C6 (venous ulcer) patients have MTS/NIVL
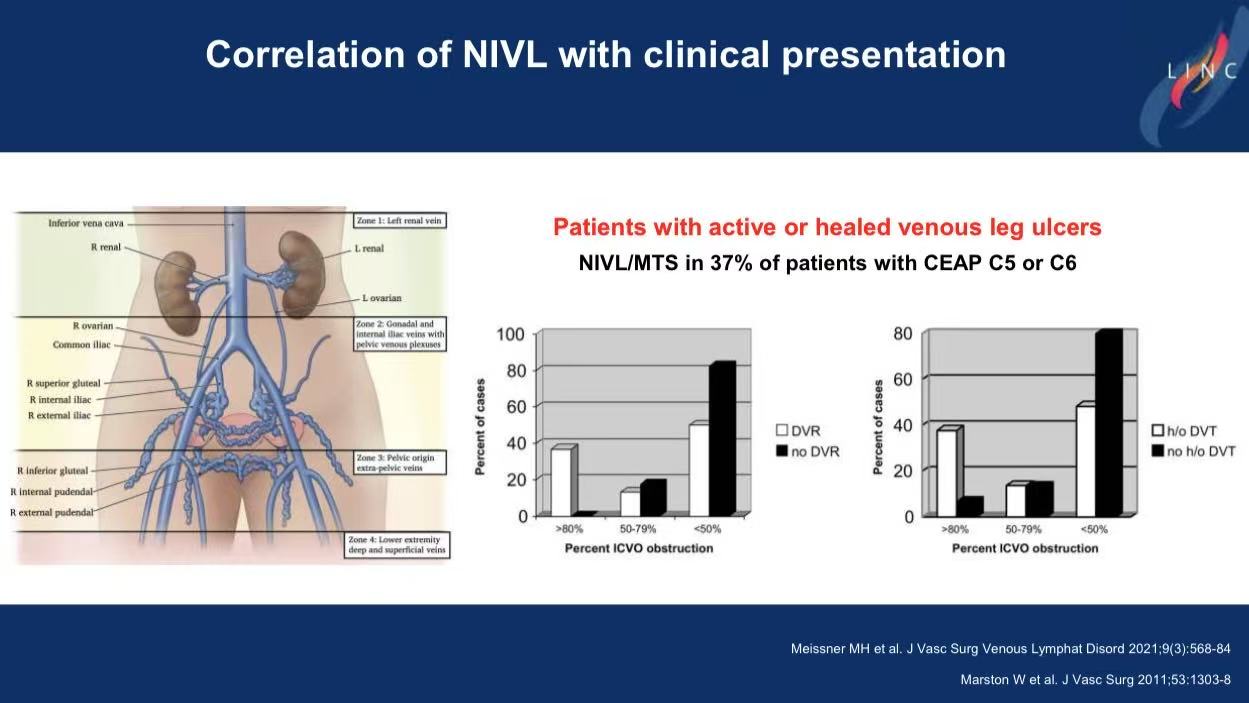
No significant correlation between stenosis severity and symptoms (p>0.05):
CEAP vs stenosis: r=0.4 (p=0.002)
VCS vs stenosis: r=0.1 (p=0.002)
3.Overtreatment Risks
Inconsistent thresholds across trials (VERNACULAR: unspecified vs VIRTUS: ≥50%)
Alert: 40% of physicians stent based solely on "translucent groove" sign (80% false-positive in healthy)
Solution: Zilver Vena Stent's Evidence Edge
1.Precision Indication
FDA approval requires >50% symptomatic stenosis
Prevents NIVL overtreatment (31.4% compression in asymptomatic)
2.Anatomy-Adaptive Design
Balanced flexibility-strength:
Conforms to Type I-III compression (lateral 70%/central 21%/partial occlusion 9%)
Fracture resistance for long-term patency (critical for inguinal ligament crossing)
Addresses warning: "Stent across ligament increases patency loss risk by 4.36-fold"
3.IVUS-Integrated Lifelong Care
Cook Medical commitment: "Investing in IVUS-guided training"
Aligns with Schlager's principle: Embed stents in comprehensive follow-up
40% post-stent patients retain venous claudication
CEAP C4-C6 cases require combined superficial/perforator intervention
Conclusion
1.Diagnostic Upgrade: Adopt IVUS as gold standard (95% sensitivity for NIVL)
2.Strict Selection: Stent only symptomatic >50% stenosis (CEAP≥C3)
3.Optimized Device: Zilver Vena’s anatomic compliance reduces complications
4.Holistic Management: Couple hemodynamic assessment + superficial vein intervention


