Presenter: Chinapath Vuthivanich
Affiliation: Vajira Hospital, Bangkok, Thailand
Abstract
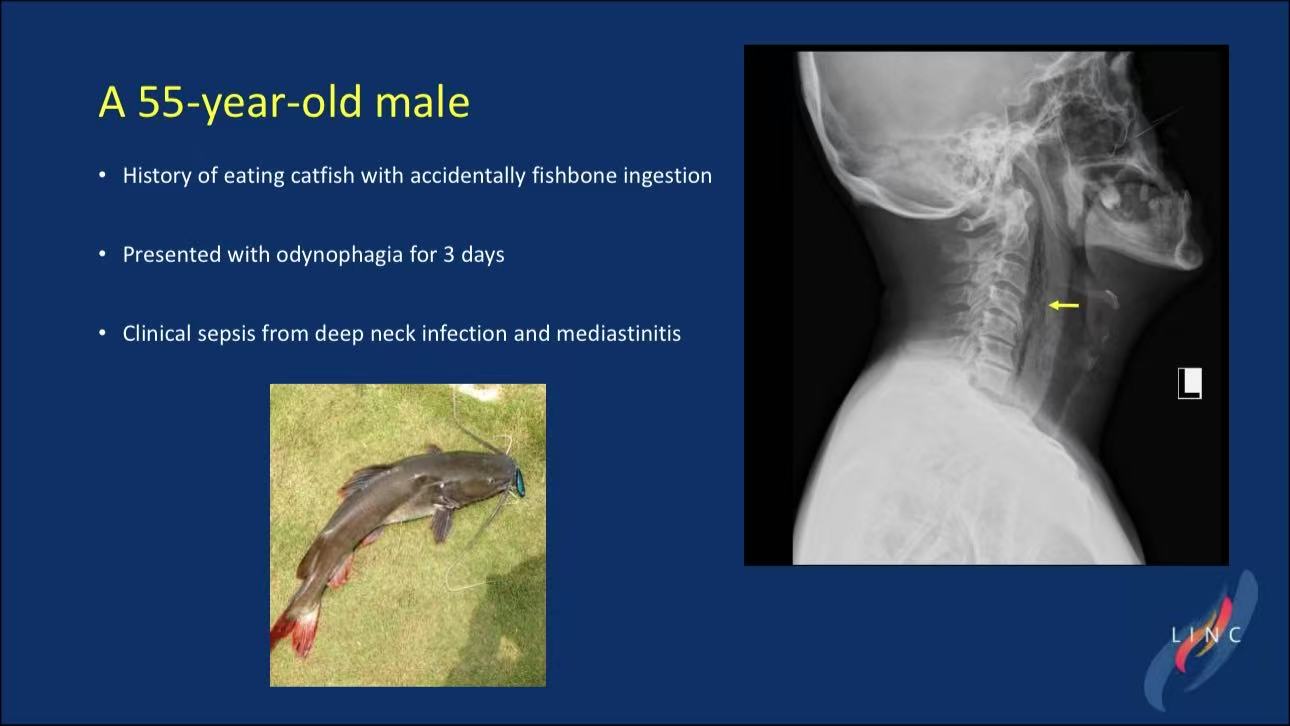
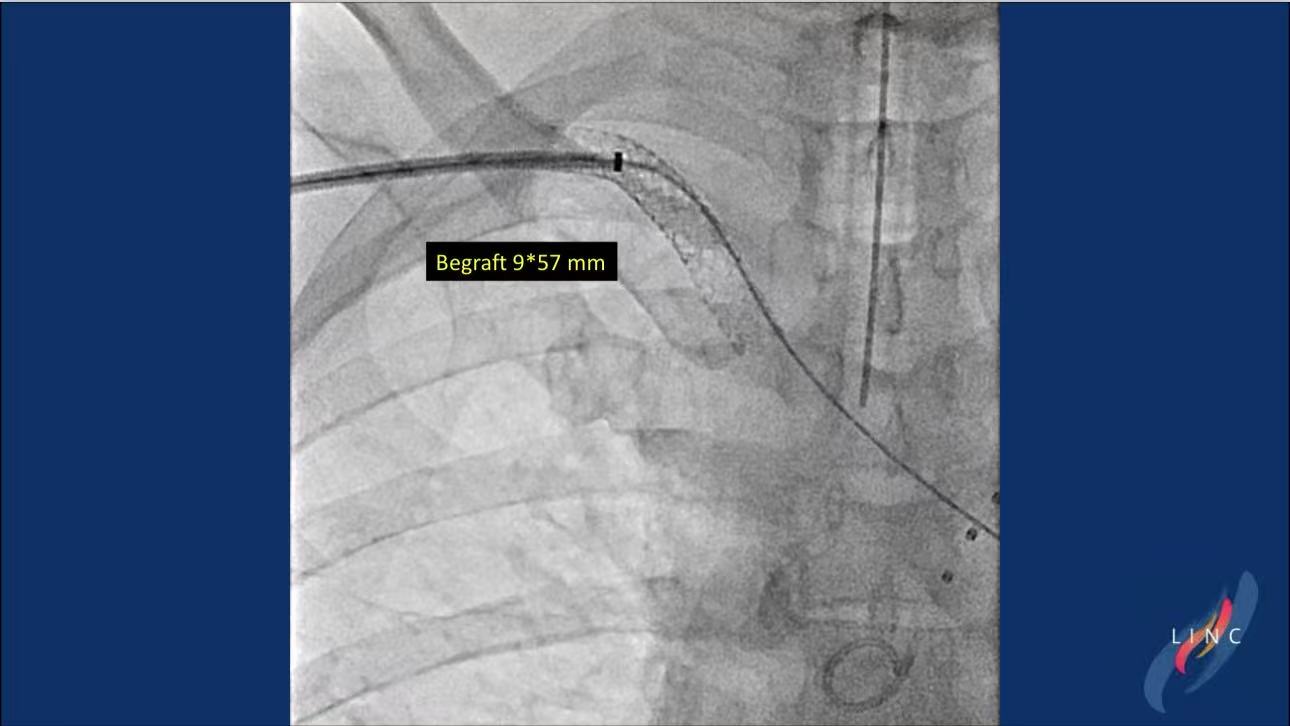
This article describes a 55-year-old male with subclavian artery pseudoaneurysm caused by fishbone penetration through the esophagus. Endovascular covered stenting (BeGraft 9×57mm) combined with surgical debridement achieved hemorrhage control and infection resolution.
Introduction
Esophageal foreign body-induced arterial injury requires urgent intervention. This case demonstrates the efficacy of a hybrid approach in life-threatening scenarios.
Case Study
The patient presented with mediastinitis and a pulsatile neck mass.
Key interventions:
Endovascular Therapy: BeGraft stent exclusion of the pseudoaneurysm.
Surgical Management: Neck exploration for fishbone removal and abscess drainage.

Postoperative Care: VATS for residual mediastinal infection.

Follow-up confirmed stent patency and clinical recovery.
Conclusions
1.Covered stents provide immediate hemorrhage control in traumatic fistulas.
2.Multidisciplinary collaboration optimizes outcomes in complex trauma.
3.Early imaging surveillance prevents delayed complications.