Presenter: Sarrath Sutthipong
Affiliation: Bhumibol Adulyadej Hospital, Bangkok, Thailand
Abstract
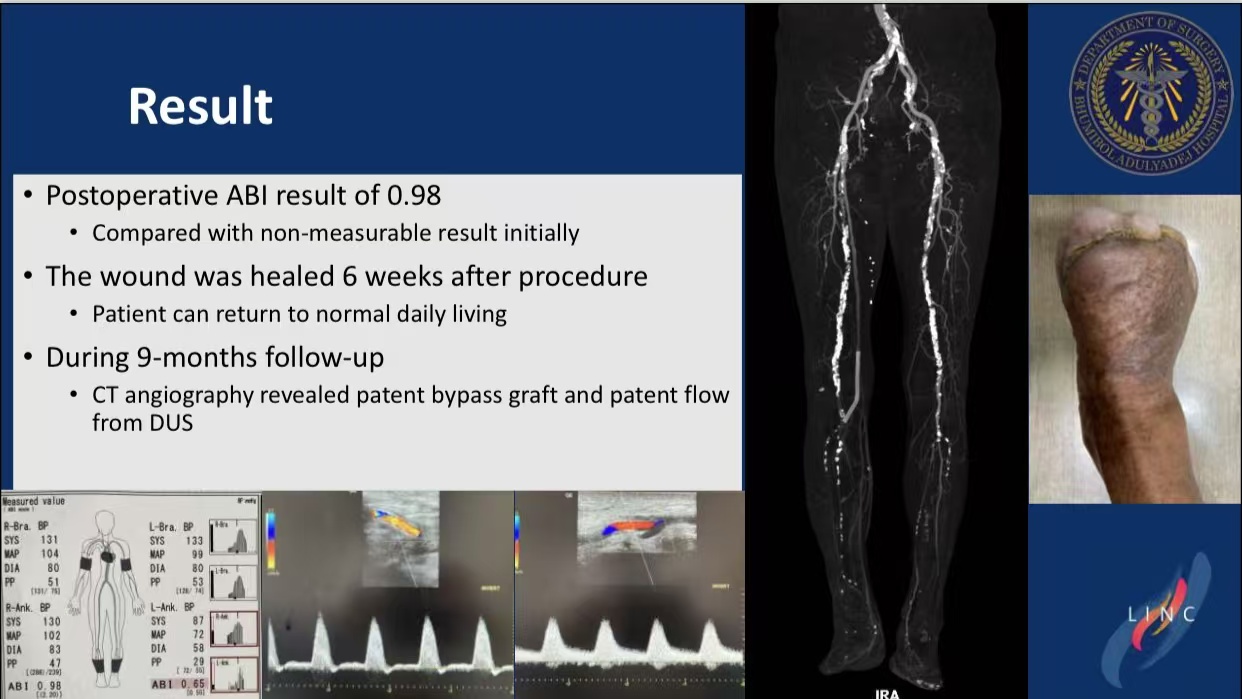
This article presents a 72-year-old male with chronic limb-threatening ischemia (CLTI) and thrombosis of a great saphenous vein (GSV) bypass graft. Percutaneous contralateral thrombectomy and stent deployment restored ankle-brachial index (ABI) to 0.98, achieving complete wound healing. This case validates endovascular therapy as an alternative to high-risk redo surgery.
Introduction
Bypass graft thrombosis poses amputation risks in CLTI. Endovascular techniques offer a minimally invasive salvage option, as demonstrated in this complex case.
Case Study
The patient had uncontrolled diabetes, CKD III, and septic shock due to extensive foot ulcers.
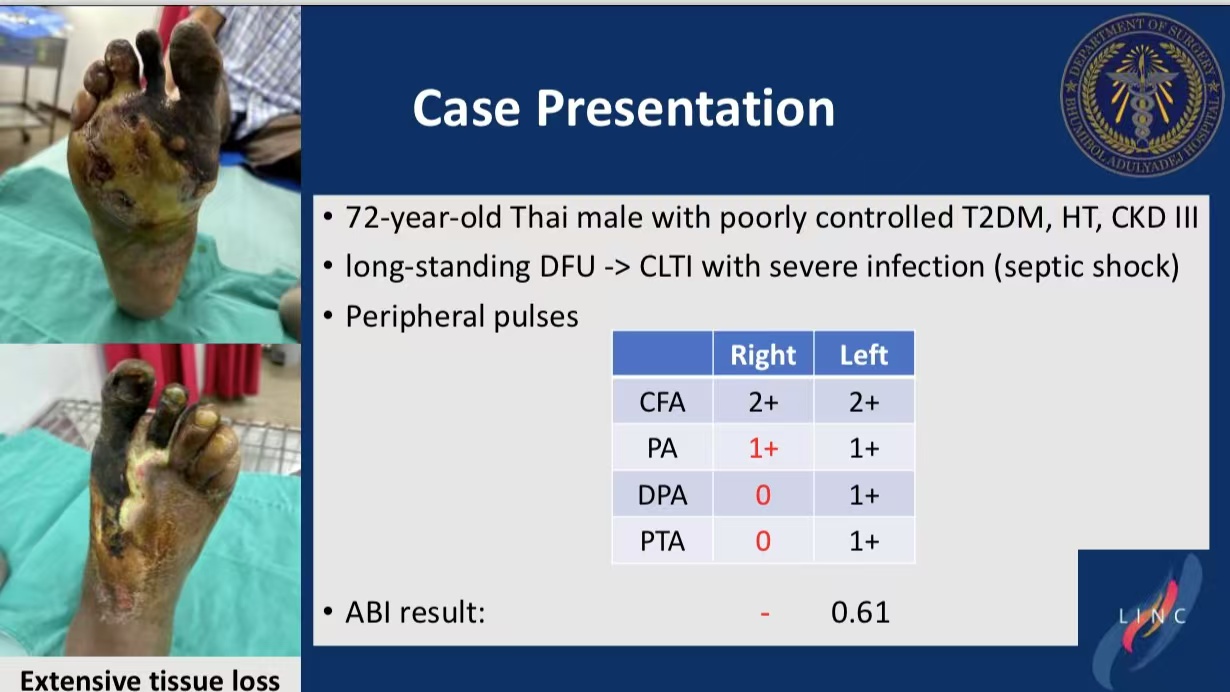
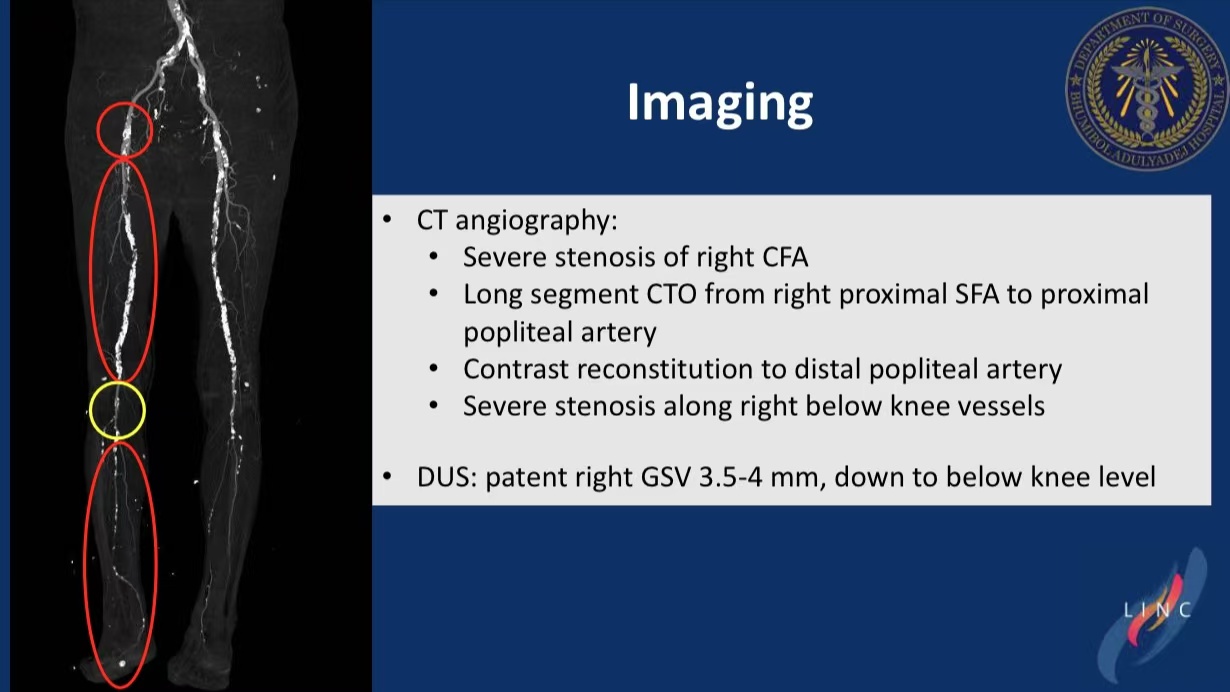
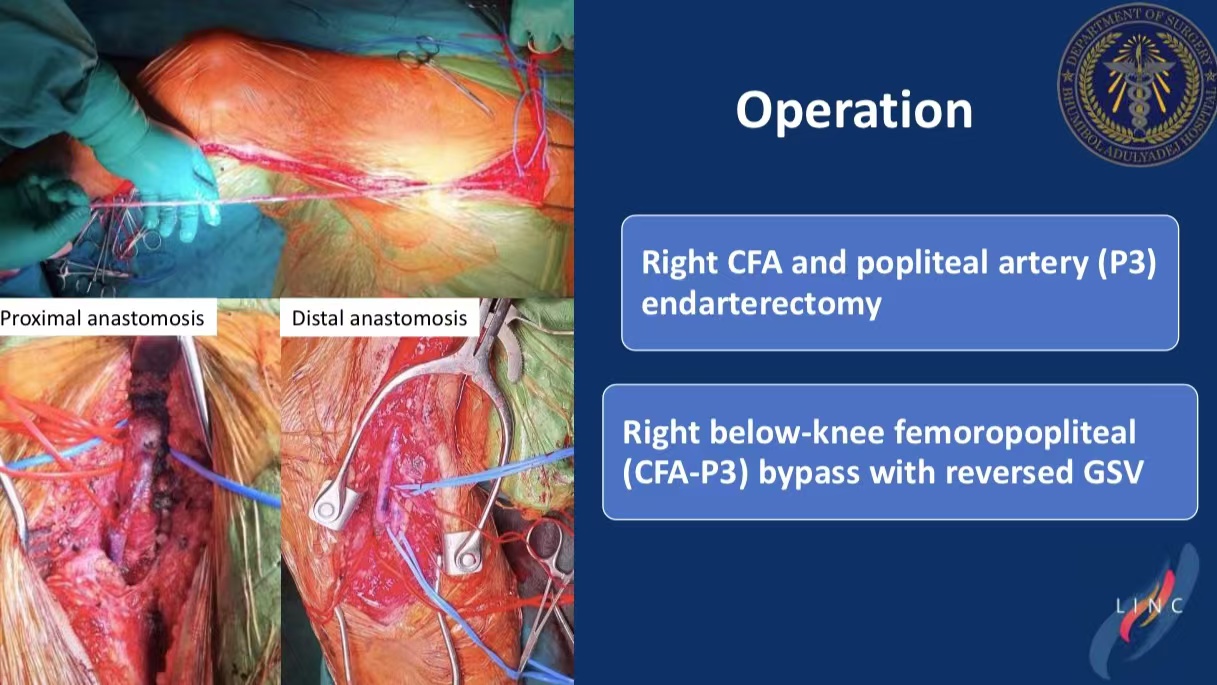
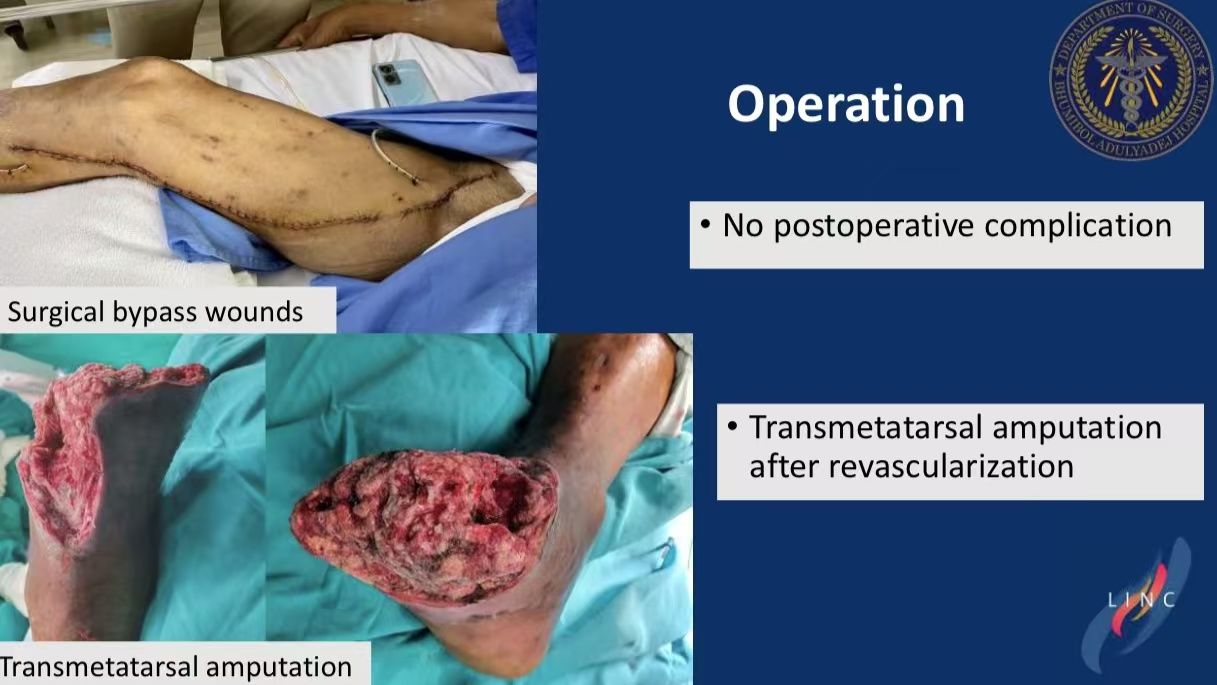
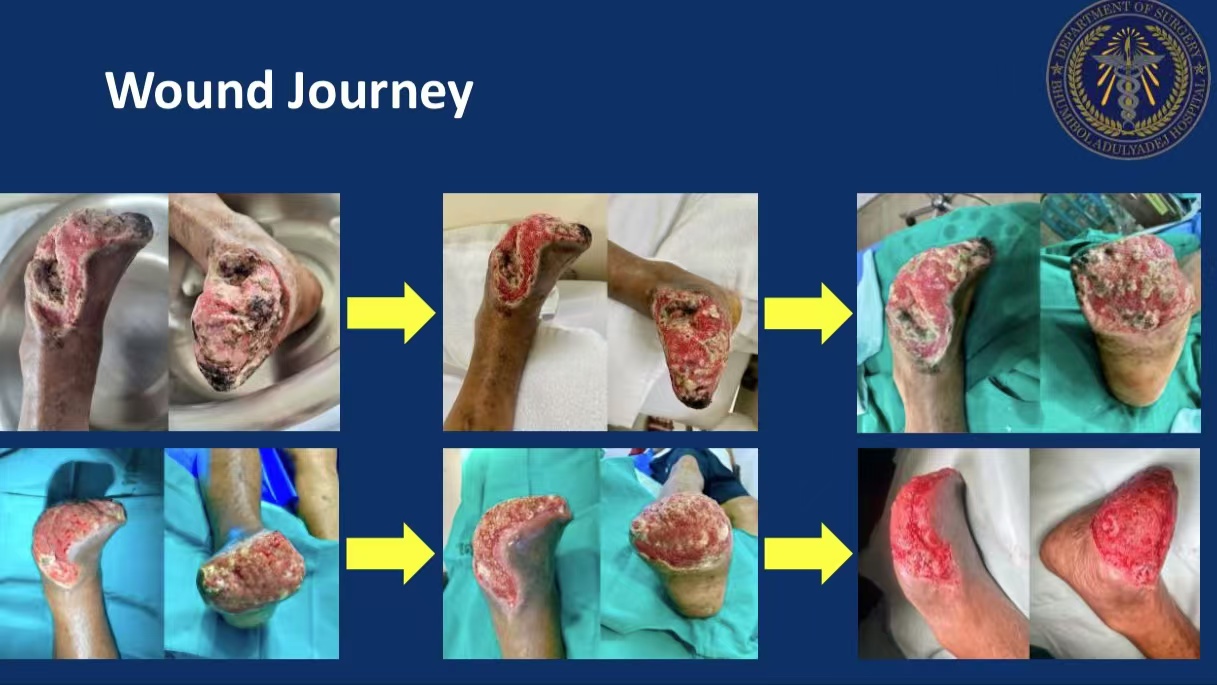
Imaging revealed right CFA stenosis and SFA-popliteal CTO. Initial surgical bypass with transmetatarsal amputation failed due to graft thrombosis.
Intervention:
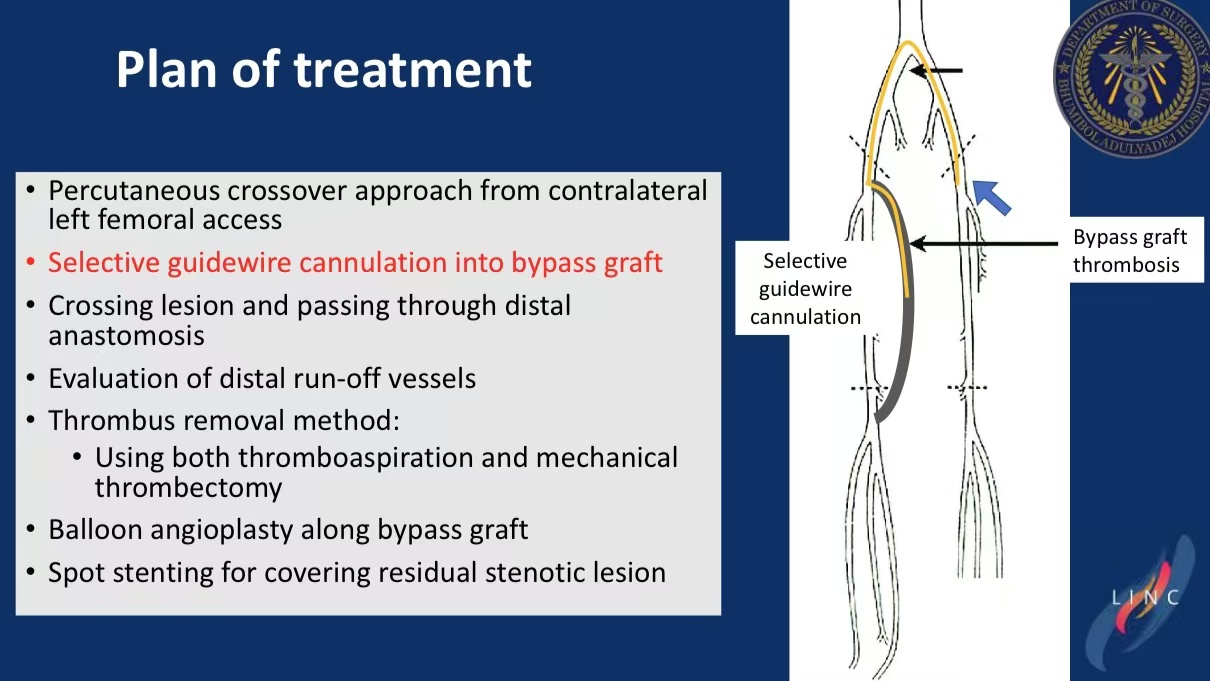
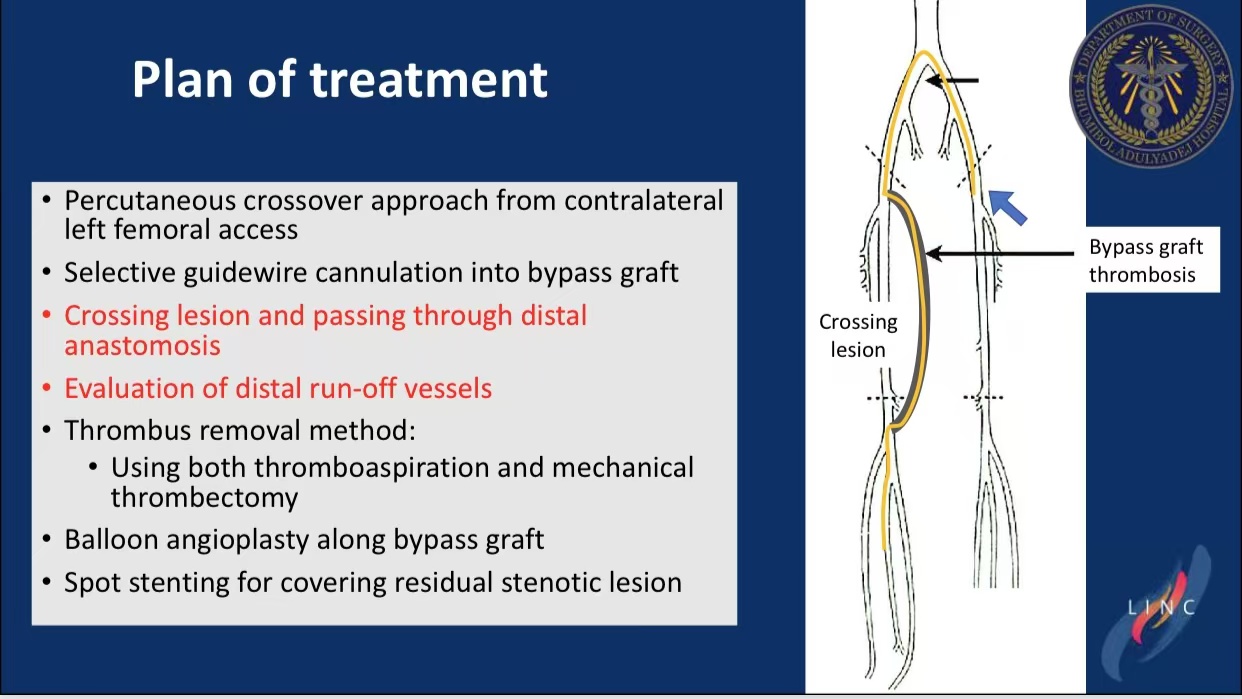
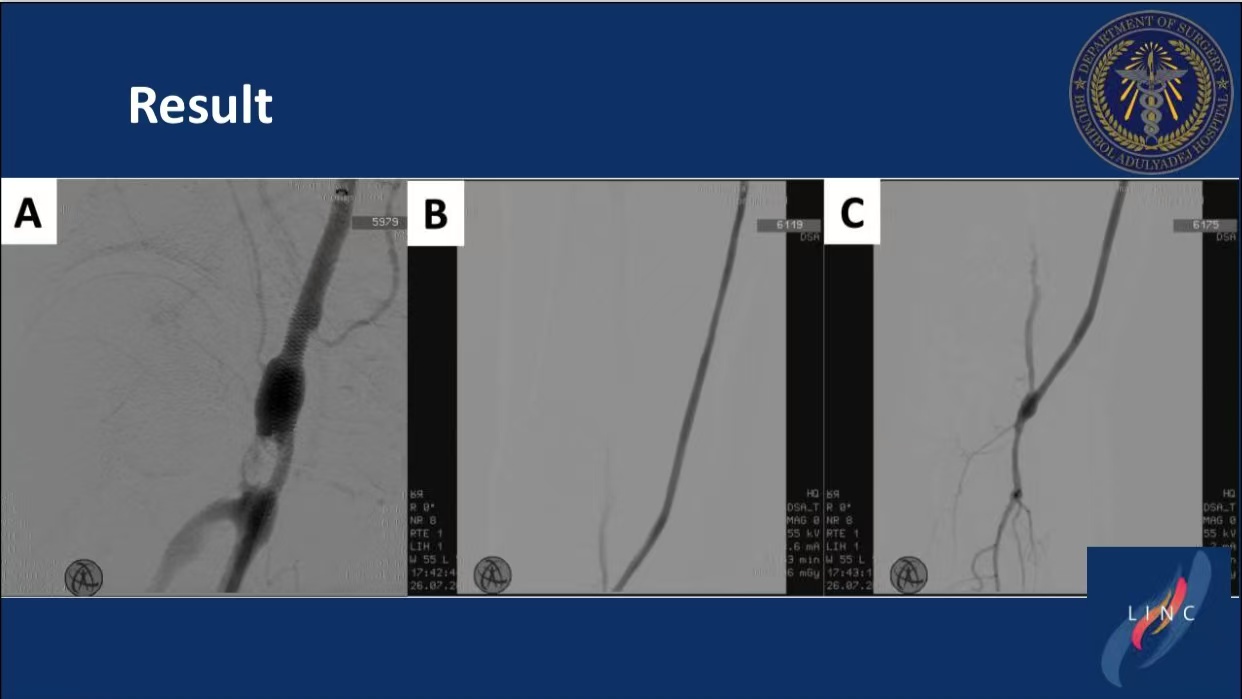
Contralateral Access: Left femoral approach with selective graft cannulation.
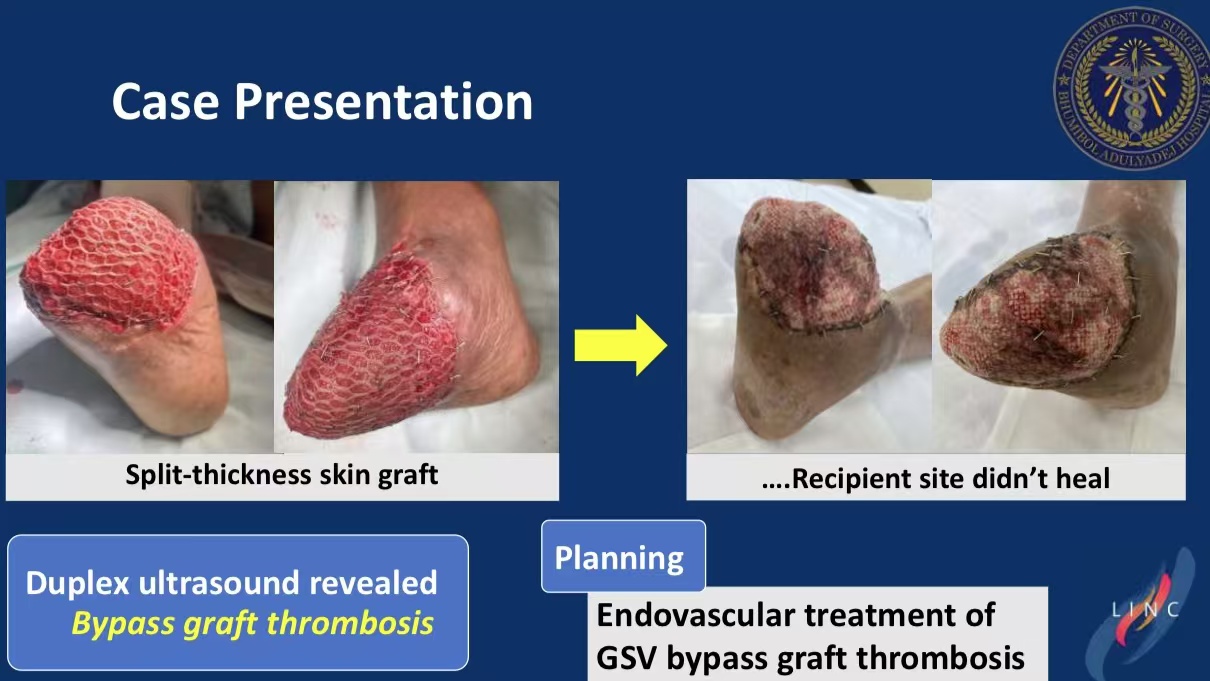
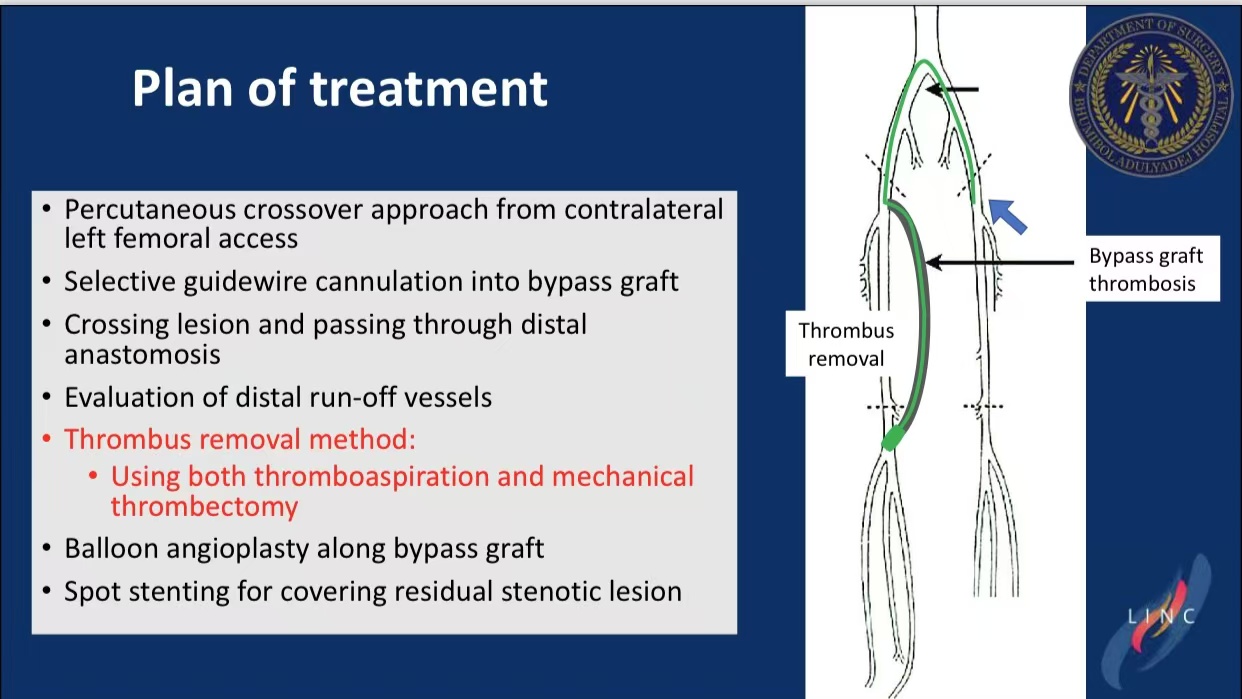
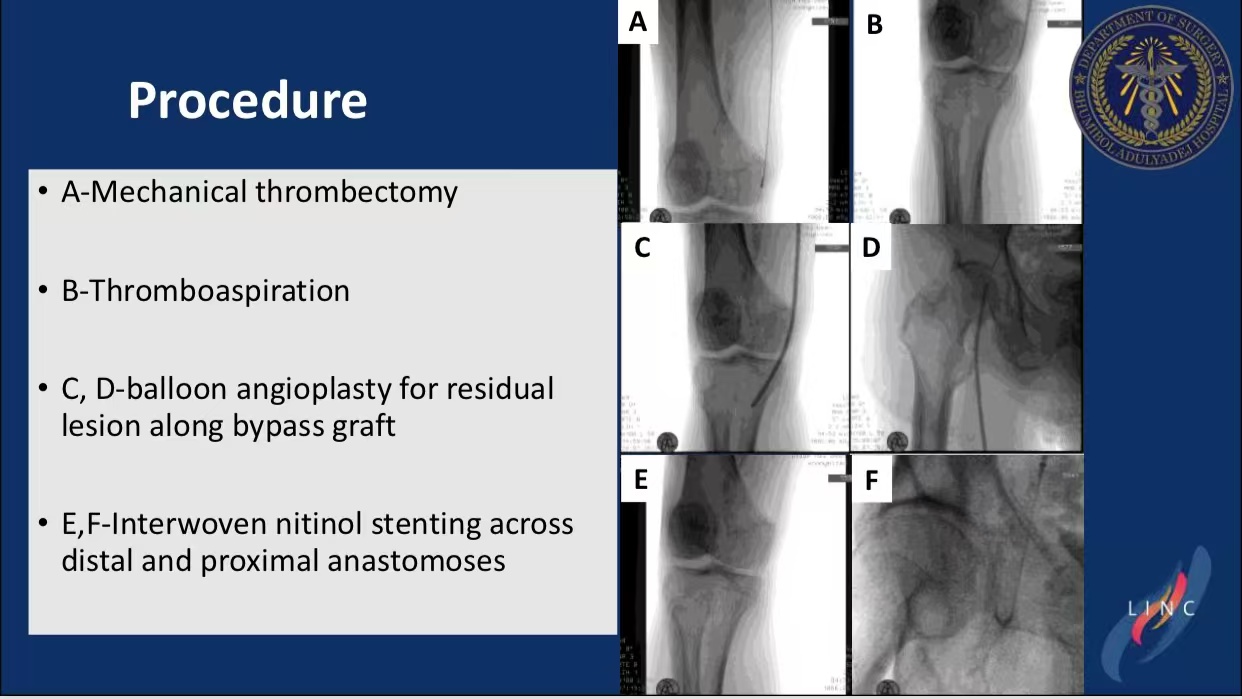
Thrombus Removal: Penumbra Indigo aspiration combined with mechanical thrombectomy.
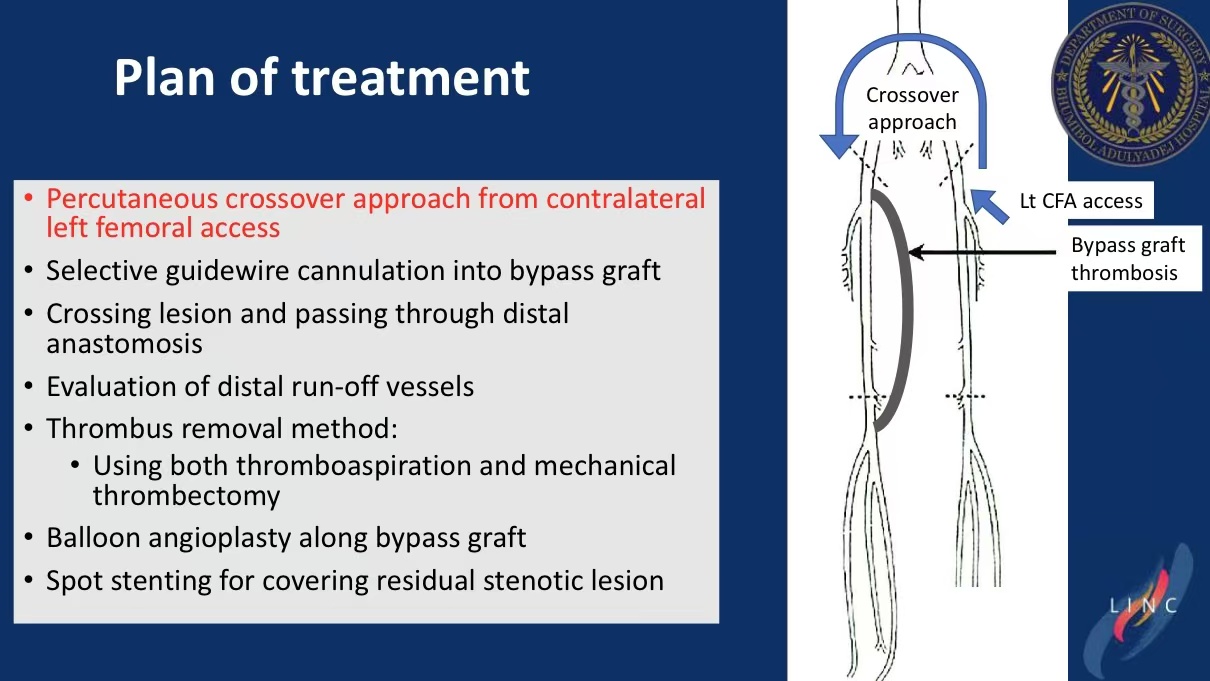
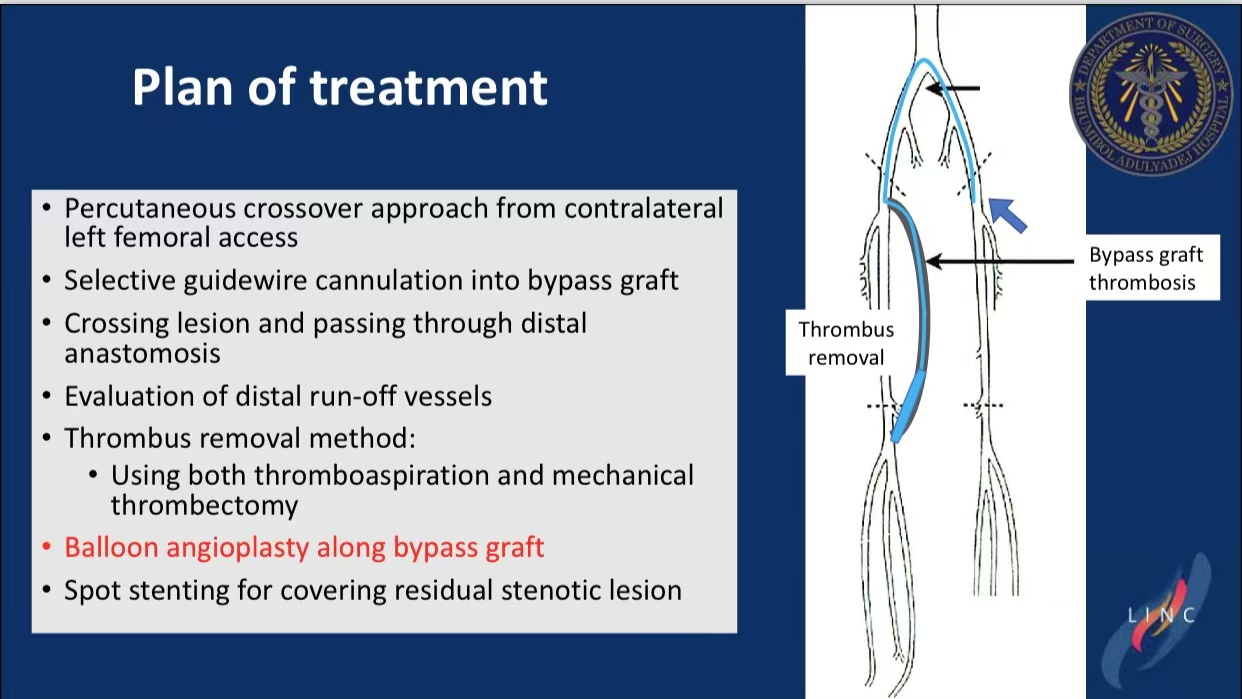
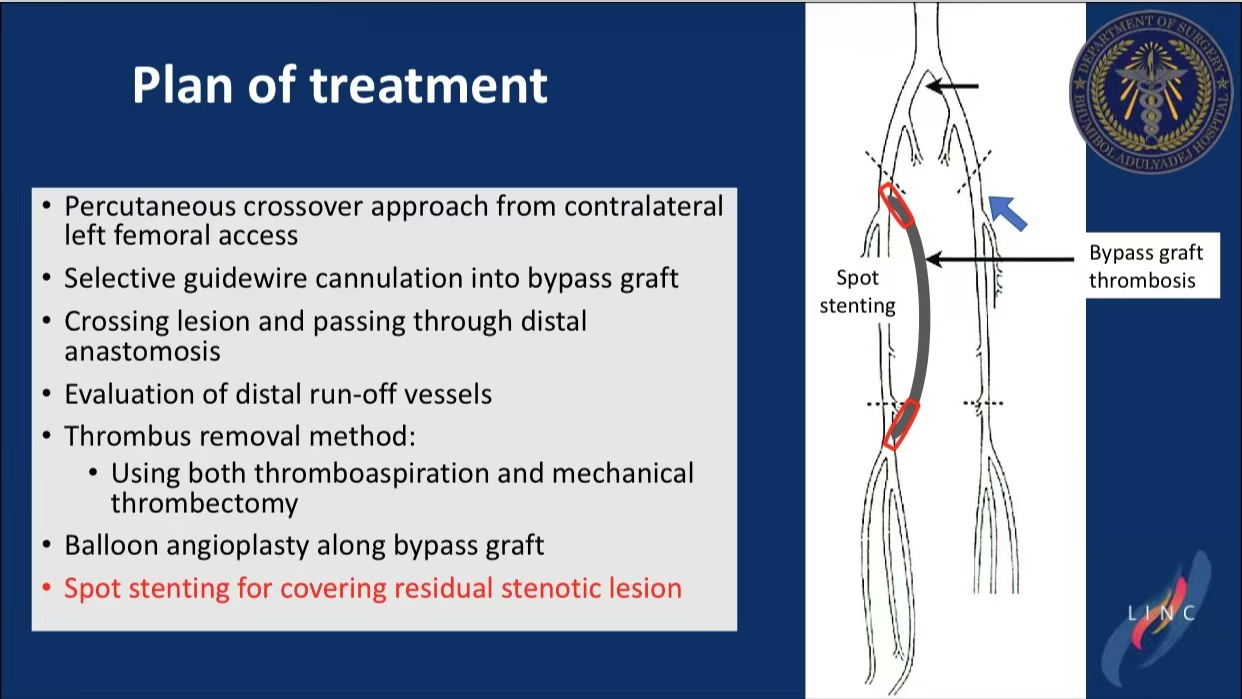
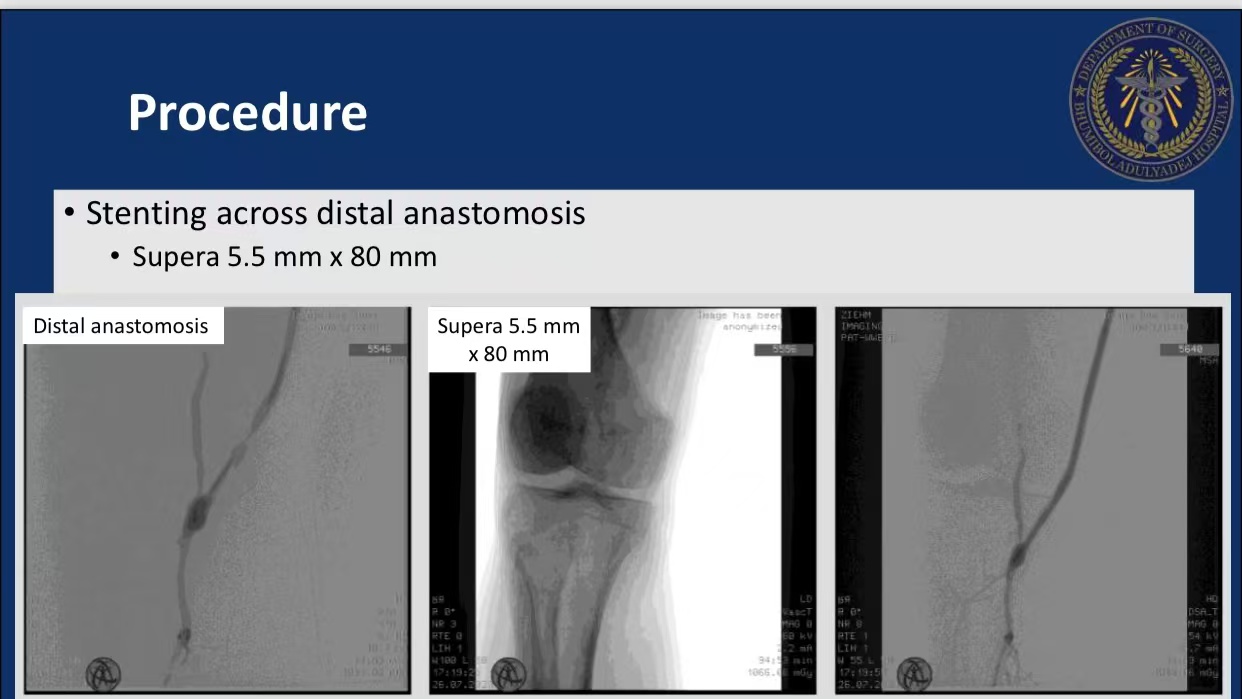
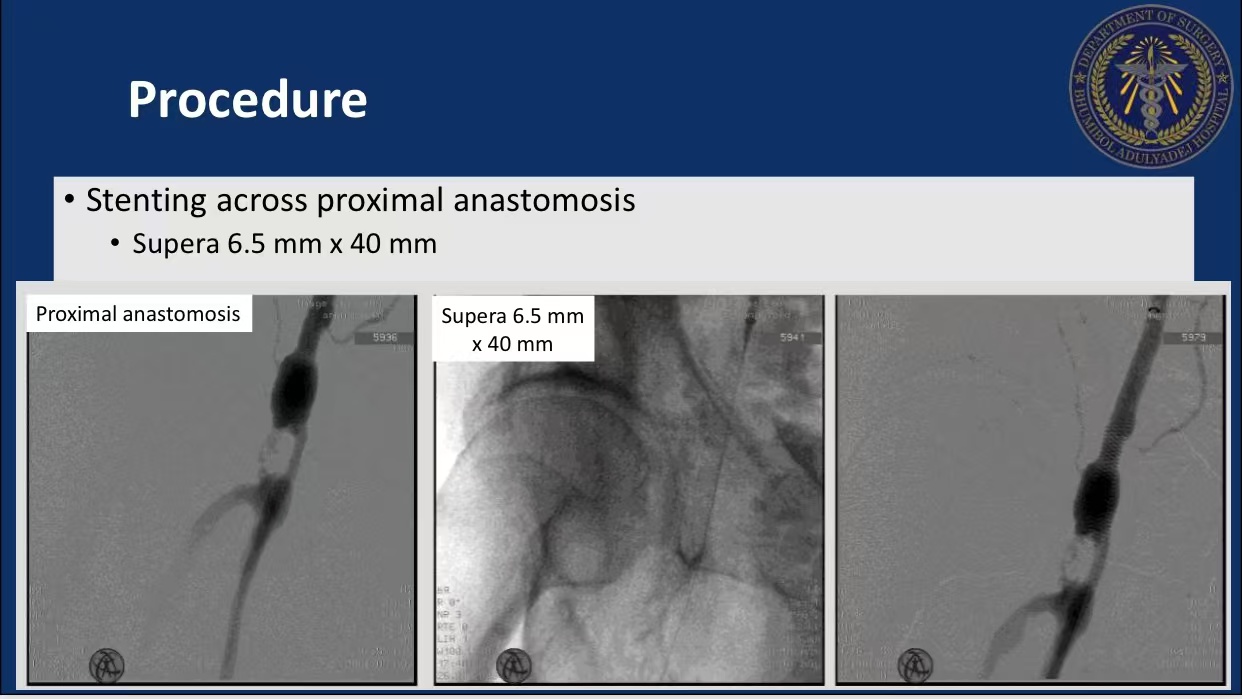
Stent Deployment: Supera® stents (5.5×80mm, 6.5×40mm) covered anastomotic sites.
At 9-month follow-up, the graft remained patent with healed wounds.
Conclusions
1.Percutaneous thrombectomy avoids redo surgery morbidity.
2.Combined thrombus removal and stenting optimizes revascularization.
3.Long-term surveillance is critical for durability assessment.