Presenter: Ho Sung Jeon
Affiliation: Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, South Korea
Co-authors: Jun-Won Lee, Jung-Hee Lee, Young Jin Youn, Sung Gyun Ahn
Abstract
This case report describes a rare complication of left common iliac vein rupture and guidewire retention during balloon angioplasty in a patient with May-Thurner Syndrome. Life-saving interventions, including urgent contralateral balloon tamponade and stent deployment, highlight the critical role of early complication recognition and multidisciplinary approaches.
Introduction
May-Thurner Syndrome, caused by left iliac vein compression, is a common etiology of deep vein thrombosis. Venous rupture and guidewire retention during intervention are life-threatening complications requiring immediate action to control bleeding and restore blood flow.
Case Analysis
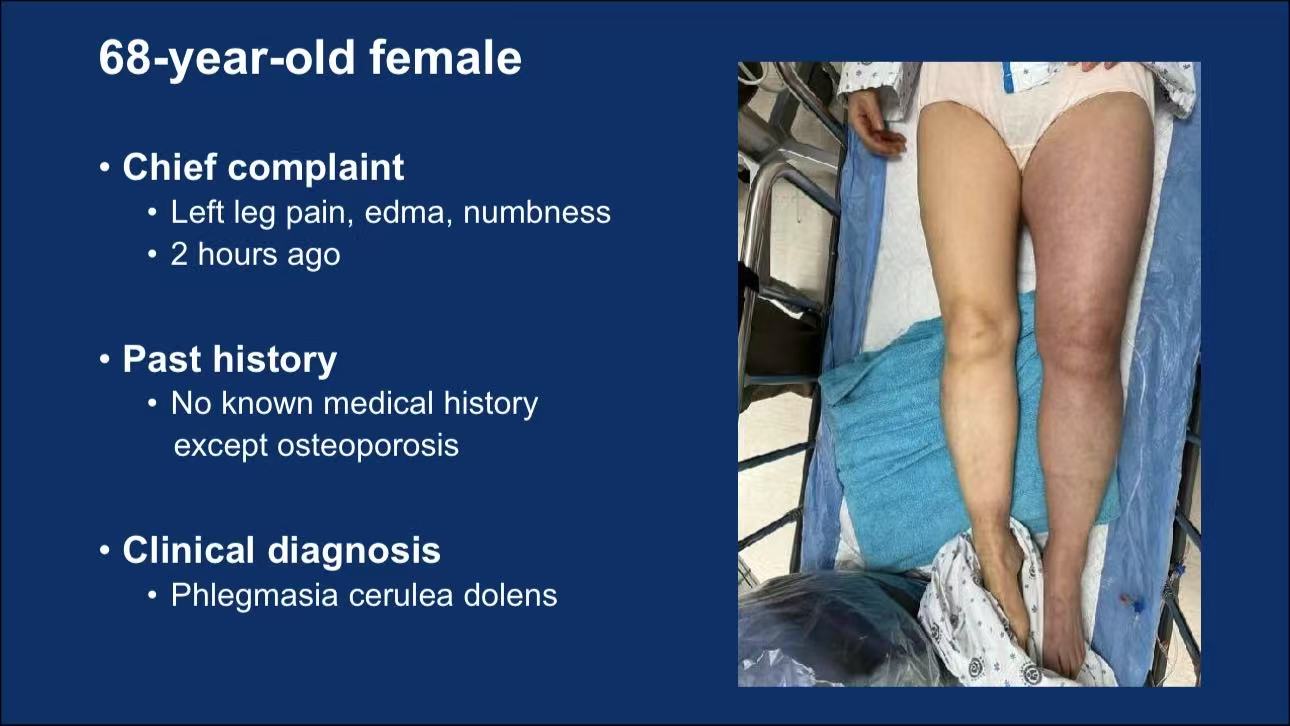
Patient Profile: A 68-year-old female presented with acute left leg pain, edema, and numbness. Past medical history included only osteoporosis. Clinical diagnosis was Phlegmasia Cerulea Dolens.
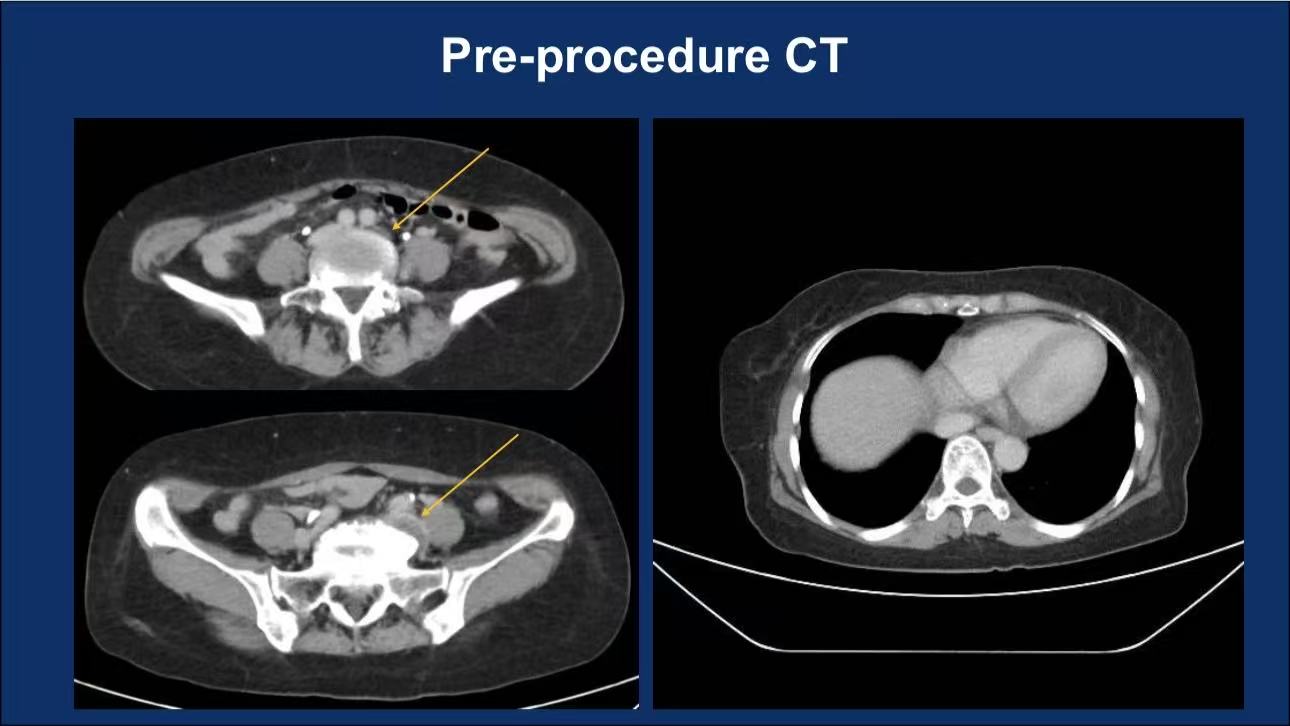
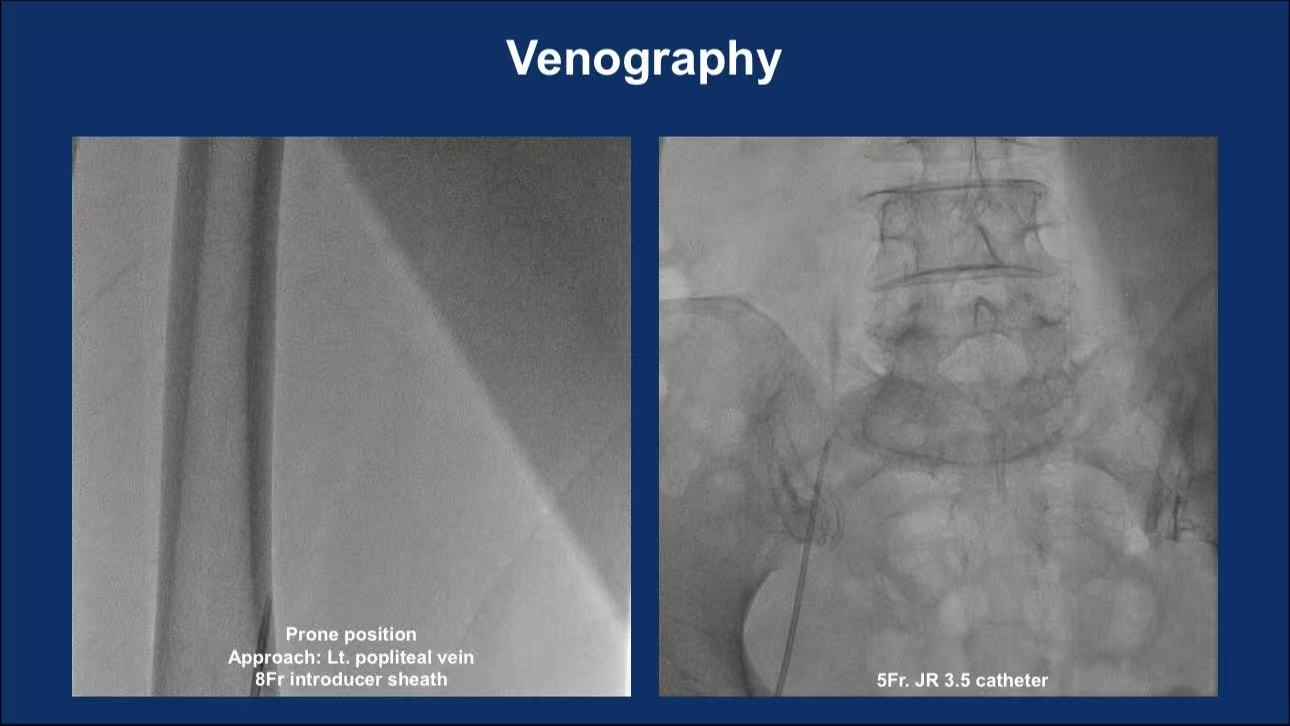
Imaging: Pre-procedural CT and venography revealed left common iliac vein stenosis with thrombosis.
Procedure:
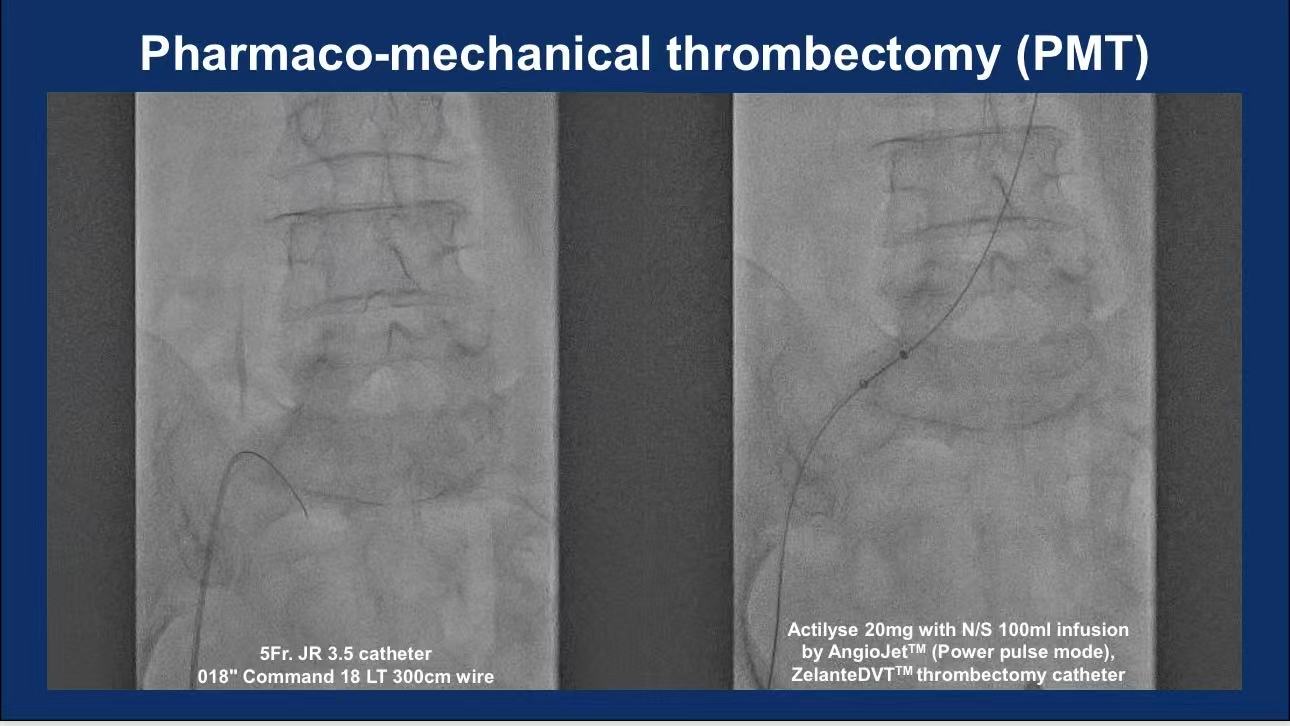
Initial Intervention: Pharmaco-mechanical thrombectomy (PMT) via left popliteal vein access using AngioJet™ (Power Pulse mode) and ZelanteDVT™ catheter.
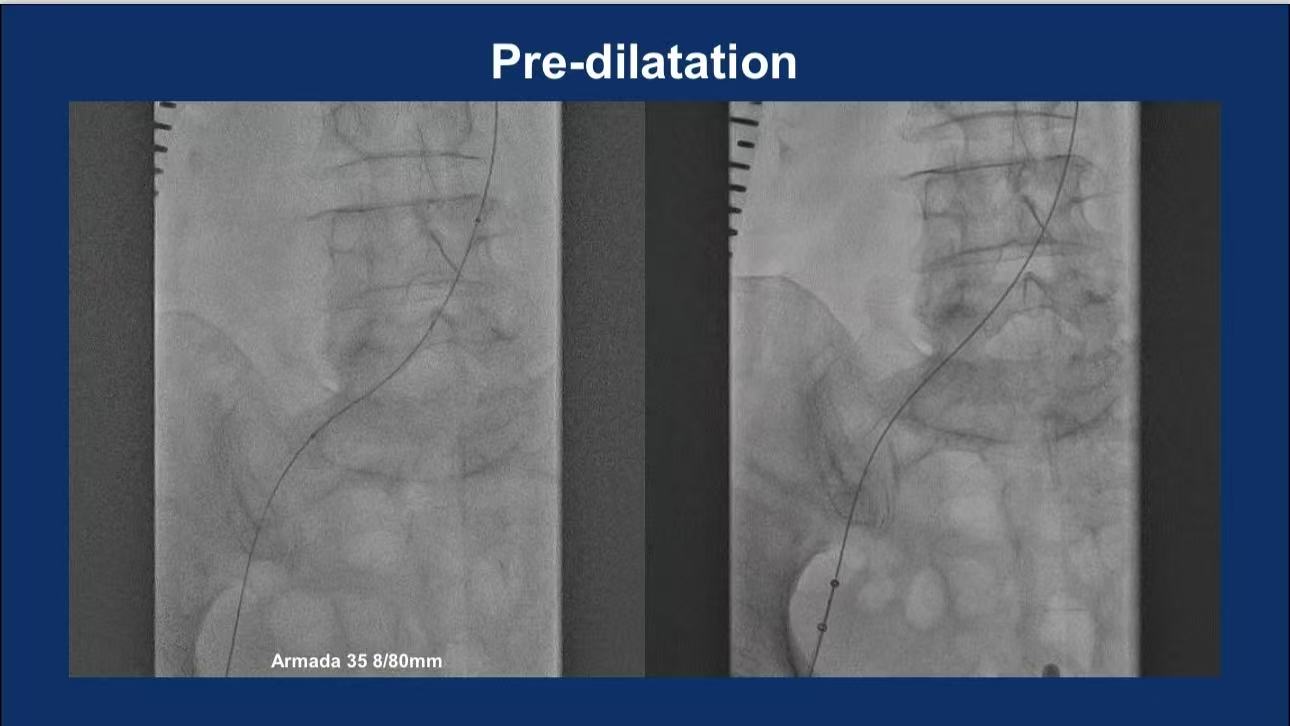
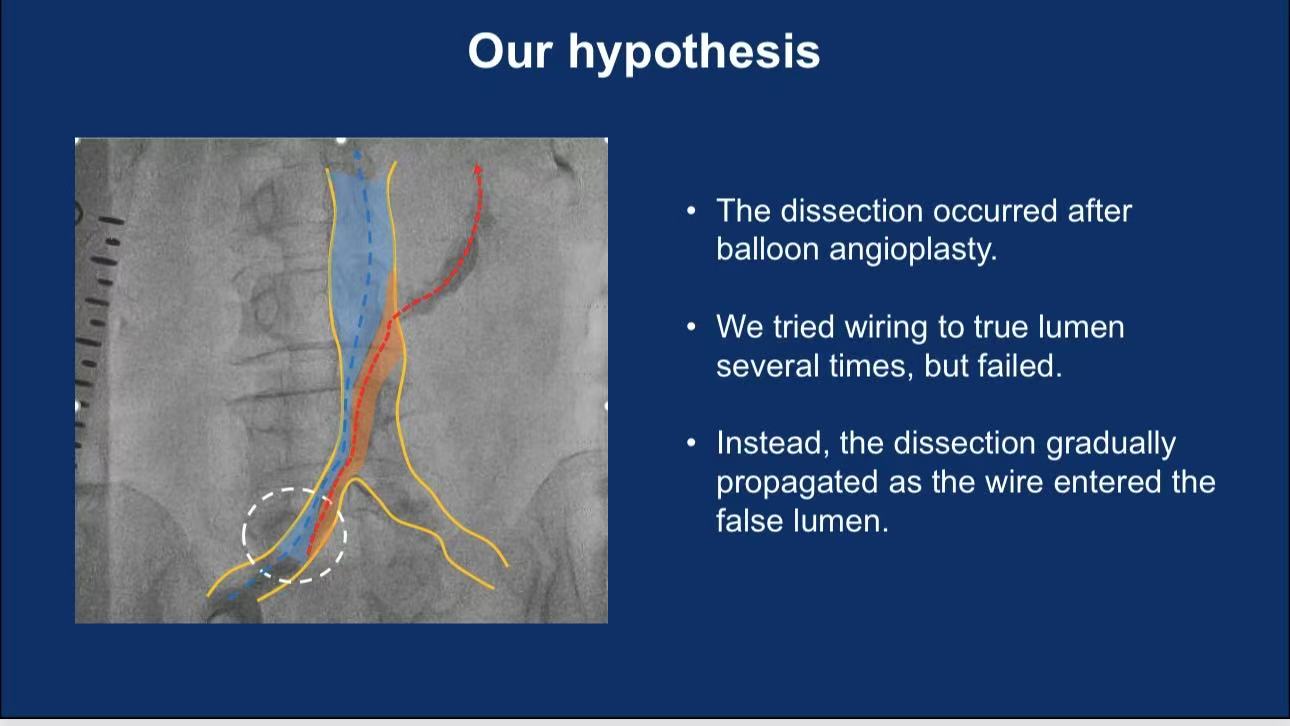
Post-balloon Complication: Vein rupture occurred after pre-dilation (Armada 35 8/80mm). Repeated attempts to wire the true lumen failed, leading to false lumen propagation.
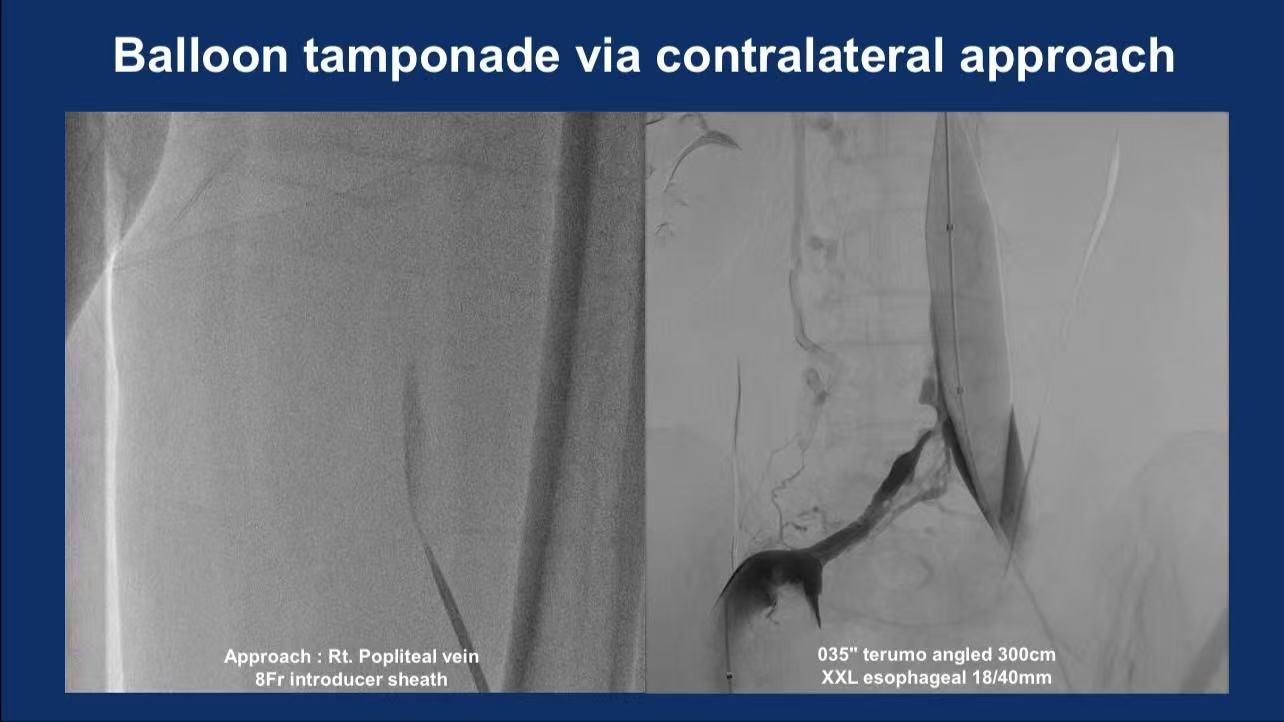
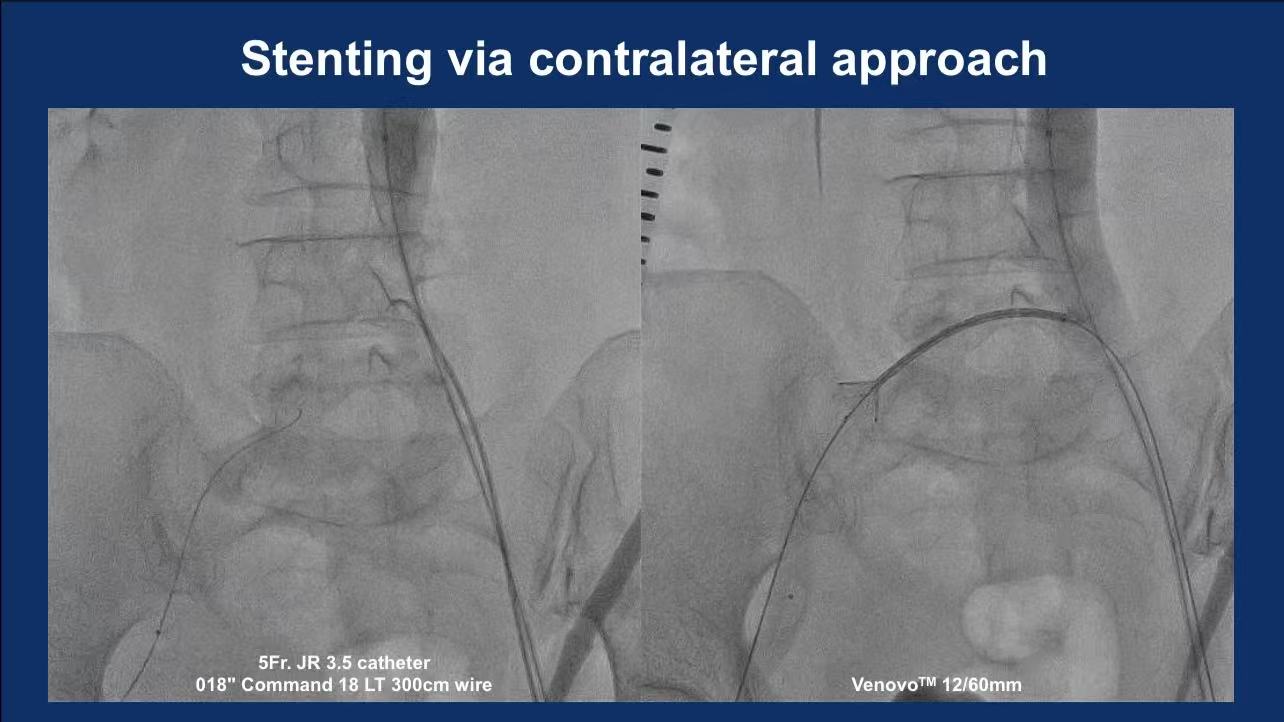
Rescue Strategy:
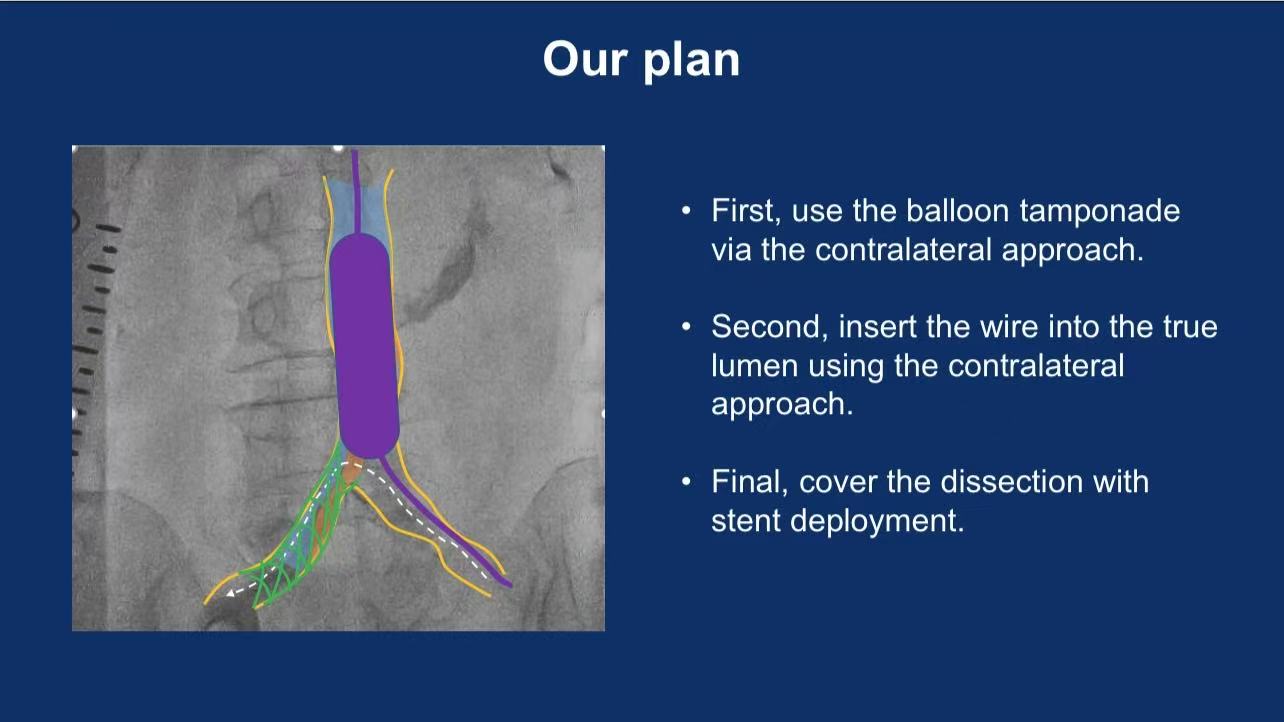
•Contralateral Balloon Tamponade: XXL Esophageal Balloon (18/40mm) via right popliteal access achieved hemostasis.
•Stent Deployment: Venovo™ 12/60mm stent was deployed using a 5Fr JR3.5 catheter and Command wire to seal the rupture.
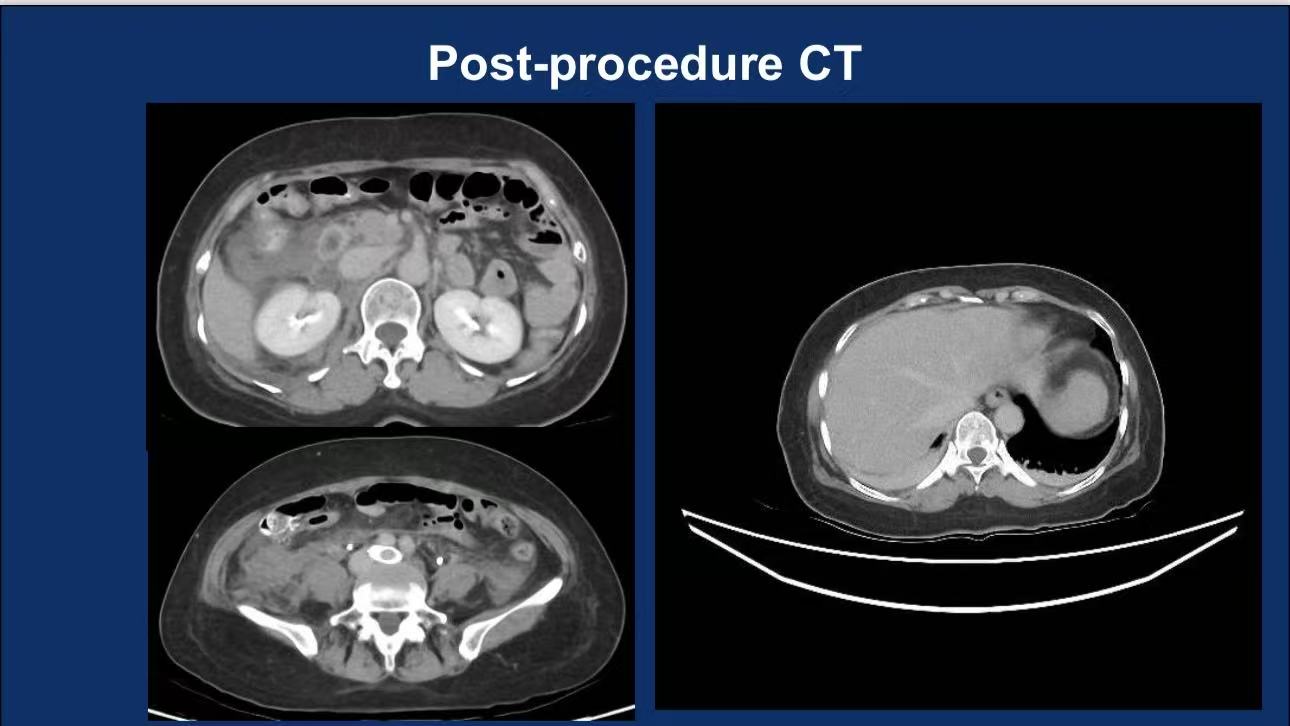
•Outcome: Final venography and CT confirmed stent patency and complete exclusion of the ruptured segment.
Conclusion
1.Thrombolysis in May-Thurner Syndrome carries bleeding risks requiring vigilant monitoring.
2.Contralateral balloon tamponade combined with stenting is a life-saving strategy for venous rupture.
3.Multidisciplinary collaboration and rapid decision-making are pivotal for favorable outcomes.